Patient Story
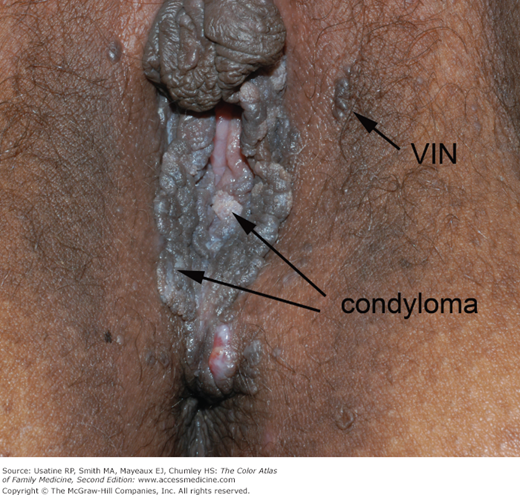
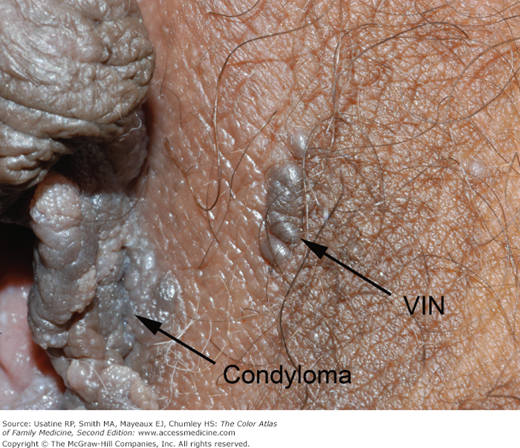
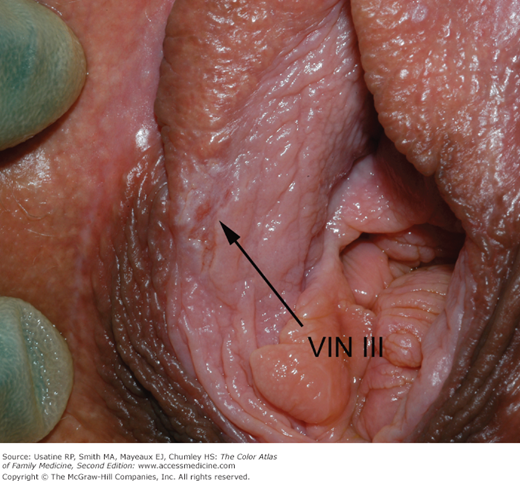
A 63-year-old black woman presents with a “knot” on her labia majora (Figures 87-1 and 87-2). She is a smoker but is otherwise healthy. The lesion is occasionally pruritic but is generally asymptomatic. She found it approximately 6 months ago, and it has been slowly increasing in size. There is no significant family history of cancer. On physical exam she is found to have exophytic condyloma acuminata around the introitus and a growth labelled vulvar intraepithelial neoplasia (VIN) that the patient called a “knot.” A 3-mm punch biopsy is performed and demonstrates VIN III. The patient is referred to gynecologic oncology.
Introduction
Epidemiology
- Vulvar cancer is the fourth most common gynecologic cancer (following cancer of the endometrium, ovary, and cervix) and accounts for 5% of lower female genital tract malignancies.1 There are approximately 3900 new cases and 870 deaths each year in the United States from this disease.1
- Worldwide, vulvar cancer is rare, especially in developing countries. Approximately 27,000 cases are reported annually, making the incidence rate between 1 and 1.5 per 100,000 women.2
- Seventy-five percent of VIN cases occur in premenopausal women, with no racial predisposition.
- Although the rate of invasive vulvar carcinoma has remained stable in the past two decades, the incidence of in situ disease (VIN) has more than doubled. This may be the result of improved surveillance and treatment of VIN, or the apparent increase in cases of VIN in younger women.3
Etiology and Pathophysiology
- VIN is the associated preneoplastic condition that is associated with the loss of epithelial cell maturation and nuclear abnormalities.
- The cervix, vagina, vulva, anus, and lower 3 cm of rectal mucosa is derived from the embryonic cloaca. Most squamous intraepithelial lesions in this area affect multiple anatomic sites.
- HPV 16 is estimated to contribute to approximately 77% of VIN lesions.4
- The risk of neoplastic progression appears to be lower with VIN than with cervical intraepithelial neoplasia. VIN I probably has minimal malignant potential, but VIN III often progresses to invasive cancer if left untreated (see “Biopsy” below).5
Risk Factors
- Risk factors are similar to those for vaginal and cervical dysplasia:6
- High-risk HPV infection.
- Cigarette smoking.
- Altered immune status.
- High-risk HPV infection.
Diagnosis
- The vulva is best examined using a good source of white light and magnification from a handheld magnifying lens or a colposcope. The examination should be systematic and incorporate all aspects of the vulvar surface. Vulvar examination may be aided by dilute acetic acid solution, which acts on the vulva much the same way as it does on the cervix and vagina. More acetic acid solution and a longer soaking time are required to achieve the acetowhite effect.
- VIN often appears as raised plaques and papules on the surface of the vulva and perineum (Figures 87-1 and 87-2).
- Approximately one quarter of these lesions are pigmented (usually brown).
- Fifty percent of VINs are white (leukoplakia) or become acetowhite after soaking with dilute acetic acid (Figure 87-3).
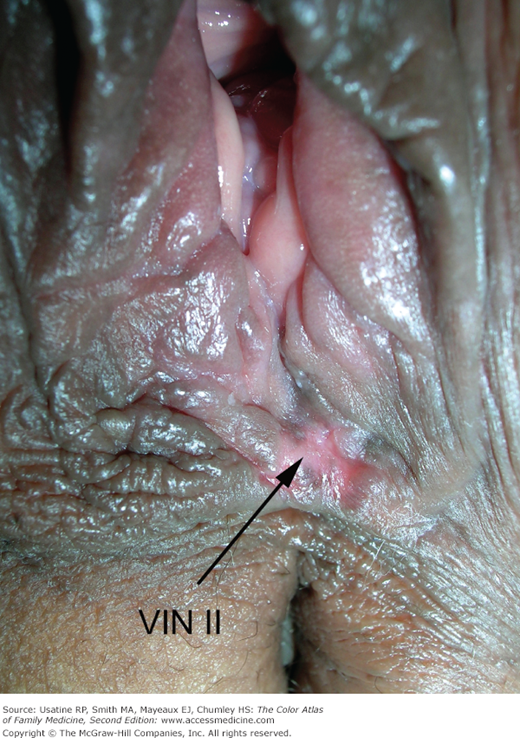
- Lesions may occasionally be red and ulcerate (Figure 87-4). White areas may also indicate malignant changes (Figures 87-5 and 87-6).
- VIN can appear warty, so lesions that are diagnosed as condyloma but do not respond to conservative therapy should be biopsied to rule out VIN.
- More than 50% of patients presenting with vulvar dysplasia are without symptoms. Of patients with symptoms, pruritus is the most common.
- Lesions may become confluent, involving the labia majora, minora, and perianal skin.
Figure 87-5
A 59-year-old woman with long history of condyloma presents with a vaginal irritation. In addition to her cystocele after her hysterectomy, she is found to have Trichomonas and evidence of atrophic changes. However, the most concerning areas are the leukoplakia at the 6-, 11-, and 12-o’clock positions. These are most suspicious for vulvar intraepithelial neoplasia. (Courtesy of Richard P. Usatine, MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree