Vitamins, Trace Elements and Metals
This chapter looks at vitamins and trace elements, and might usefully be read in conjunction with Chapter 14 (Nutrition). It also discusses certain elemental metals that are important in disease states.
At one time, vitamins were thought to be amines and hence the term ‘vitamines’ was coined for substances that are essential for life but needed in only minute amounts. Vitamins are now known to be organic compounds, not necessarily amines, which are essential for normal growth and development. They must be included in the diet because the body either cannot synthesize them at all or cannot do so in amounts sufficient for its needs.
Trace elements are inorganic compounds that, like vitamins, are essential for health and needed only in small amounts, known as the reference nutrient intake. A normal mixed diet should provide adequate amounts of vitamins and trace elements, and thus supplementation is not usually necessary.
Testing for vitamin and trace element deficiency should be carried out as soon as the diagnosis is suspected; the results of laboratory tests usually revert rapidly to normal once the patient has resumed eating a normal diet, for example after admission to hospital, and it may then be impossible to confirm the original diagnosis. Where the diagnosis is difficult, a trial of the micronutrient may be the most reliable and simplest method of assessment.
VITAMIN DEFICIENCIES
These may have the following causes:
inadequate intake: deficiencies are rarely seen in affluent populations except in:
individuals with an inadequate dietary intake or unusual diet,
chronic alcoholism,
patients with anorexia nervosa,
patients on parenteral or enteral nutrition,
inadequate absorption, for example malabsorption states,
excess loss, for example via gastrointestinal or renal tract,
enhanced utilization, for example sepsis or trauma.
VITAMIN EXCESS
Some vitamins (notably A and D) are toxic if taken in excess, and overdosage has recently become more common, possibly because of the increased availability of these compounds in over-the-counter preparations.
CLASSIFICATION OF VITAMINS
Vitamins are classified into two groups on the basis of their solubilities: fat soluble and water soluble. The distinction is of clinical importance because steatorrhoea may be associated with a deficiency of fatsoluble vitamins, with relatively little clinical evidence of lack of most of the water-soluble vitamins except B12 and folate.
Fat-soluble vitamins
The principal fat-soluble vitamins are:
A (retinol),
D (calciferol),
E (α-tocopherol),
K (2-methyl-1,4-naphthoquinone).
Each of these has more than one active chemical form, but variations in structure are minimal and in this chapter each vitamin is considered as a single substance.
Vitamin A (retinol)
Sources
Precursors of vitamin A (the carotenes) are found in the yellow and green parts of plants and are especially abundant in carrots. The active vitamin is formed by the hydrolysis of β-carotene in the intestinal mucosa;
each molecule can produce two molecules of vitamin A, which are absorbed as retinol esters and stored in the liver. Retinol is transported to tissues bound to the α-globulin retinol-binding protein (RBP).
each molecule can produce two molecules of vitamin A, which are absorbed as retinol esters and stored in the liver. Retinol is transported to tissues bound to the α-globulin retinol-binding protein (RBP).
Vitamin A is stored in animal tissues, particularly the liver, and is also present in milk products and eggs.
Functions
Rhodopsin (visual purple), the retinal pigment that is necessary for vision in poor light (scotopic vision), consists of a protein (opsin) combined with vitamin A. Rhodopsin decomposes in bright light. It is partly regenerated in the dark, but, because this is not quantitatively complete, vitamin A is needed to maintain retinol levels. Vitamin A is also essential for normal mucopolysaccharide synthesis and mucus secretion.
Clinical effects of vitamin A deficiency
The clinical effects of vitamin A deficiency include the following.
Owing to rhodopsin deficiency:
‘night blindness’ (nyctalopia): deficiency is associated with poor vision in dim light, especially when the eyes have recently been exposed to bright light.
Owing to deficient mucus secretion leading to drying and squamous metaplasia of ectodermal tissue:
Skin secretion is diminished and there may be hyperkeratosis of hair follicles. Dry, horny papules (follicular hyperkeratosis) are found mainly on the extensor surfaces of the thighs and forearms. Squamous metaplasia of the bronchial epithelium has also been reported and may be associated with a tendency to develop chest infections.
The conjunctiva and cornea become dry and wrinkled, with squamous metaplasia of the epithelium and keratinization of the tissue (xerosis conjunctivae and xerophthalmia). Bitot’s spots are elevated white patches, composed of keratin debris, found in the conjunctivae. Prolonged deficiency leads to keratomalacia, with ulceration and infection and consequent scarring of the cornea, causing blindness.
Poor bone growth in the skull, leading to cranial nerve compression.
Anaemia, which responds to vitamin A but not to iron therapy.
Causes of vitamin A deficiency
Hepatic stores of vitamin A are large and therefore clinical signs develop only after many months, or even years, of dietary deficiency. Such prolonged deficiency is very rare in affluent communities. In steatorrhoea, clinical evidence of vitamin A is rare, although plasma concentrations may be low. Deficiency is relatively common in poor countries, especially in children, and can cause blindness.
Diagnosis and treatment of vitamin A deficiency
The diagnosis is usually made on the basis of clinical criteria; very low plasma vitamin A concentrations usually confirm deficiency. In conditions such as noncirrhotic liver disease, in which plasma concentrations of RBP are low, concentrations of vitamin A may be decreased despite normal liver stores. In cirrhosis of the liver, the stores may be very low. Laboratory tests for the diagnosis of vitamin A deficiency consist of testing for plasma retinol concentration. Retinol-binding protein is also low in vitamin A deficiency, but this may also occur in protein deficiency and the acute-phase response.
Vitamin A deficiency can be treated with retinyl palmitate. High doses of vitamin A should be given to treat xerophthalmia and advanced skin lesions. ‘Night blindness’ and early retinal and corneal changes often respond rapidly to treatment, although corneal scarring may be irreversible.
Hypervitaminosis A
Vitamin A in large doses is toxic. Acute intoxication has been reported in Arctic regions as a result of eating polar bear liver, which has very high vitamin A content. More commonly, overdosage is due to the excessive use of vitamin preparations.
In acute poisoning, symptoms include nausea and vomiting, abdominal pain, drowsiness and headache. Pregnant women are usually advised not to eat liver, which is a storage organ for many vitamins, to avoid the risk of fetal damage.
Chronic hypervitaminosis A is associated with fatigue, insomnia, bone pain, loss of hair, desquamation and discoloration of the skin, hepatomegaly, headaches, abdominal pain, bone and joint pain, benign intracranial hypertension, osteoporosis and weakness.
Additionally, a very high intake of carrots or orange juice can lead to carotenaemia, which can mimic jaundice except that plasma bilirubin is normal.
Vitamin D (calciferol)
The metabolism and functions of vitamin D, the effects and treatment of its deficiency and hypocalcaemia are discussed in Chapter 6, as are disorders of bone, including rickets and osteomalacia.
Overdosage may cause hypercalcaemia. In chronic overdosage, stores of cholecalciferol are large and therefore hypercalcaemia may persist, or even progress, for several weeks after ingestion of the vitamin is stopped.
Vitamin E (α-tocopherol)
Vitamin E acts as an antioxidant, and deficiency can have many clinical sequelae.
Vitamin E deficiency
The common causes of vitamin E deficiency are poor intake and fat malabsorption, for example cystic fibrosis. Low plasma concentrations may also be seen in the rare hypobetalipoproteinaemia or abetalipoproteinaemia, in which there are low concentrations of the lowdensity lipoprotein (LDL) that is involved in carrying some of the fat-soluble vitamins (see lipid metabolism, Chapter 13). The clinical features of vitamin E deficiency include increased haemolysis, a possibly increased risk of atherosclerosis and, in low-birthweight babies, retrolental fibroplasias and intraventricular haemorrhages.
Laboratory tests for deficiency consist of measurement of plasma vitamin E levels (or perhaps better expressed as vitamin E to LDL cholesterol ratio); α-tocopherol is the most active form. Sometimes increased erythrocyte haemolysis can be measured in the laboratory as an index of vitamin E deficiency.
It has been proposed that supplementation of dietary antioxidants such as vitamins A, C and E may protect against atherosclerosis by reducing LDL oxidation. However, the results of some intervention trials have been disappointing, having failed to show any significant reduction in cardiovascular events for those on antioxidant supplementation. Vitamin E excess is rare.
Vitamin K
Vitamin K is needed for the synthesis of prothrombin and coagulation factors VII, IX and X in the liver, and deficiency is accompanied by a bleeding tendency with a prolonged prothrombin time. Clinically, vitamin K is sometimes given to reverse the actions of the anticoagulant warfarin in patients in whom it is causing bleeding problems, as evidenced by a prolonged prothrombin time or international normalized ratio (INR). Vitamin K is also involved in bone mineralization.
Vitamin K can be synthesized by bacteria in the ileum, from where it can be absorbed, and thus dietary deficiency is unlikely. However, deficiency may occur:
in patients with steatorrhoea – the vitamin, whether taken in the diet or produced by intestinal bacteria, cannot be absorbed normally,
after the administration of some broad-spectrum antibiotics, which may alter the intestinal bacterial flora and so reduce the synthesis of vitamin K, especially in children.
If vitamin K deficiency occurs, it can be corrected by parenteral administration.
In the newborn infant, plasma vitamin K concentrations are lower than in adults because very little can be transported across the placenta, the neonatal gut is only gradually colonized by bacteria capable of synthesizing vitamin K and protein synthesis has not yet reached full adult capacity, particularly in premature infants. Deficiency may be severe enough to cause haemorrhagic disease of the newborn infant, a condition that may present within 2-3 days of birth.
Laboratory tests for vitamin K deficiency are usually indirect, involving measurement of the prothrombin time. Although one can measure blood vitamin K or its metabolites or PIVKA (proteins induced by vitamin K absence) in specialized laboratories, these are rarely indicated. Overdose of vitamin K is rare and may sometimes cause haemolytic anaemia. Vitamin K treatment may perturb warfarin requirements of patients being anticoagulated.
Water-soluble vitamins
The water-soluble vitamins are:
the B complex:
thiamine (B1),
riboflavin (B2),
nicotinamide (niacin),
pyridoxine (B6),
folate (pteroylglutamate),
the vitamin B12 complex (cobalamins),
biotin and pantothenate,
ascorbate (vitamin C).
Thiamine, folate, vitamin B12 and ascorbate are actively absorbed from the intestinal tract and the rest diffuse passively through the intestinal mucosal wall.
The vitamin B complex
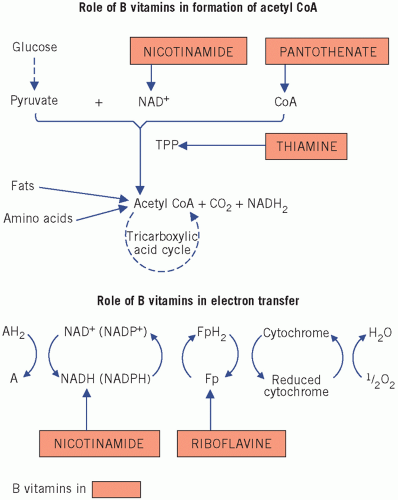
Most of these vitamins act as enzyme cofactors and many are synthesized by colonic bacteria. As the absorption of water-soluble vitamins from the large intestine is poor, probably most of those synthesized within the colon are unavailable to the body.
Clinical deficiency is rare in affluent communities. When deficiency does occur, it is usually multiple, involving most of the B group, and is associated with protein undernutrition; for this reason it may be difficult to decide which signs and symptoms are specific for an individual vitamin and which are part of a general undernutrition syndrome (Fig. 15.1). With the exception of vitamin B12, assay of these vitamins is rarely indicated and treatment is usually given empirically if a deficiency state is suspected.
Thiamine (B1)
Sources and causes of deficiency
Humans cannot synthesize thiamine. It is found in many dietary components; wheat germ, oatmeal and yeast are particularly rich sources. Adequate amounts are present in a normal diet and deficiency is most common in alcoholics and in patients with anorexia nervosa.
Functions
Thiamine is a component of thiamine pyrophosphate, which is an essential cofactor for decarboxylation of 2-oxoacids; one such reaction is the conversion of pyruvate to acetyl coenzyme A (see Chapter 12). In thiamine deficiency, pyruvate cannot be metabolized and accumulates in the blood. Thiamine pyrophosphate is also an essential cofactor for transketolase in the pentose-phosphate pathway.
Clinical effects of thiamine deficiency
Deficiency is usually due to excess ethanol intake with high carbohydrate but poor vitamin intake, although it can also be seen in intensive-care patients with high carbohydrate intake. One of the commonest causes worldwide is a diet high in un-enriched white flour or rice. The level of thiaminase, which breaks down thiamine, is high in raw fish.
Deficiency of thiamine causes beri beri, in which anorexia, emaciation, neurological lesions (motor and sensory polyneuropathy, amnesia and encephalopathy known as Wernicke-Korsakoff syndrome) and cardiac arrhythmias may occur. This form is called ‘dry’ beri beri (shoshin) and is associated with low cardiac output. In ‘wet’ beri beri there is peripheral oedema, sometimes associated with cardiac failure. Thiamine deficiency can be seen as part of the refeeding syndrome (see Chapter 14). Beri beri may be aggravated by a high-carbohydrate diet, possibly because this leads to an increased rate of glycolysis and therefore of pyruvate production.
Laboratory diagnosis of thiamine deficiency
One test for thiamine deficiency is the estimation of erythrocyte transketolase activity, with and without added thiamine pyrophosphate. Reduced activity, if due to thiamine deficiency, becomes normal after the addition of the cofactor. This test is rarely indicated and of little use once a normal diet, or vitamin supplementation, has been started because plasma concentrations are rapidly corrected. Other tests may be useful, including the measurement of both blood and urinary thiamine concentrations, and a raised blood pyruvate concentration is suggestive as is a lactic acidosis (see Chapter 4).
Riboflavin (B2)