Nutrition
This chapter gives an outline of certain nutritional abnormalities and how they overlap with aspects of chemical pathology. It is not, however, a substitute for a nutrition textbook. The reader may also find Chapters 12 and 13 (on carbohydrate and lipid disorders, respectively), Chapter 15 (on vitamin/trace elements) and Chapter 16 (on gastrointestinal function) relevant. Nutrition is an important topic, as about 1 billion of the world’s population are overweight yet, ironically, at the same time approximately 1 billion are undernourished or starving.
Adequate nutrition is essential for a variety of reasons, including optimal cardiovascular function, muscle strength, respiratory ventilation, protection from infection, wound healing and psychological wellbeing.
The principles of carbohydrate and lipid metabolism and gastrointestinal digestion and absorption all have important implications in the management of nutrition, and of intravenous (parenteral) nutrition in particular. These principles, including those of fluid and electrolyte homeostasis, must be fully understood in order to manage patients receiving parenteral nutrition.
Daily energy loss as heat is about 120 kJ (30 kcal) per kilogram of body weight in a normal adult. In addition, there is a daily protein turnover of about 3 g/kg body weight (about 0.5 g of nitrogen), of which about 0.15 g of nitrogen/kg body weight is excreted (1 g of nitrogen is derived from about 6.25 g of protein). These losses are usually balanced by dietary intake of equivalent amounts of energy, as carbohydrate, fat and protein. Glucose provides 4 kcal/g, and fat 9 kcal/g.
Excess energy is stored as glycogen and triglyceride. If expenditure exceeds intake, these energy stores are drawn upon. In a well-nourished adult, enough energy is stored as hepatic glycogen to last at least a day, and therefore post-operative patients without complications do not need intravenous feeding. Once this store has been depleted, energy is derived from triglyceride, and later from body tissue components such as the proteins of cells, including those of muscle. This may cause severe ketosis from the metabolism of fats and ketogenic amino acids and increase nitrogen turnover and loss. The daily energy and nitrogen requirements are not constant, as we will now see.
STARVATION
During starvation the body tries to maintain blood glucose levels in the acute phase and in the longer term to preserve body protein mass.
Hepatic glycogen stores are largely consumed within 24 h. The obligatory glucose requirements of the brain, erythrocytes and other organs are met by gluconeogenesis. During the first week or so of acute starvation, up to 150 g of protein is utilized to achieve this. Insulin levels decrease, resulting in amino acid (mainly alanine) release from protein, glycogen conversion to glucose, and adipocyte fatty acid release for energy needs. Plasma insulin concentration is reduced, but concentrations of glucagon, glucocorticoids, catecholamines and growth hormone are raised. Thus, blood glucose concentrations are generally maintained despite starvation.
In later starvation, ketone bodies replace glucose as the predominant brain fuel (ketoadaptive phase) and a metabolic acidosis may result. The ketone bodies also inhibit muscle protein degradation and the flow of alanine into the circulation. There is thus a decrease in urinary nitrogen excretion, a decline in hepatic gluconeogenesis and increased brain oxidation of ketone bodies while plasma amino acid concentrations decrease. Plasma insulin is reduced, as are glucagon, glucocorticoids, catecholamines and growth hormone.
Starvation results in initial rapid weight loss, mostly due to protein breakdown and diuresis. The latter is partly due to increased renal tubule urea load and results in renal loss of calcium, phosphate and
potassium. Continuing starvation results in a slower decline in body weight, as after the gluconeogenic phase fat is catabolized. This is associated with water conservation about 3-5 days later. The basal metabolic rate (BMR) decreases and the kidney becomes the most important gluconeogenic organ, using glutamine to synthesize glucose.
potassium. Continuing starvation results in a slower decline in body weight, as after the gluconeogenic phase fat is catabolized. This is associated with water conservation about 3-5 days later. The basal metabolic rate (BMR) decreases and the kidney becomes the most important gluconeogenic organ, using glutamine to synthesize glucose.
Feeding converts the situation to an anabolic state. The level of ketone bodies falls, along with a decline in urinary nitrogen. Thus, positive nitrogen balance can be achieved with fat gain.
TRAUMA AND SEPSIS
In the face of trauma, including burns, the body strives for wound healing and the evoked response is directly related to the severity of the injury. Two phases have been described.
Early ebb or shock phase Here, in an attempt to survive, there is a decrease in body energy expenditure to conserve resources. Plasma insulin concentration is reduced but concentrations of glucagon, glucocorticoids, catecholamines and growth hormone are raised. There is reduced oxygen consumption and decreased glucose oxidation.
Later flow or hypermetabolic phase Should blood volume be restored and circulation satisfactory, then the flow phase may take place. Concentrations of hormones, such as glucagon, glucocorticoids, catecholamines and growth hormone, increase, as may that of insulin. Consequently, gluconeogenesis (which may lead to hyperglycaemia) occurs, as does proteolysis. Urinary nitrogen loss can range from more than 25 g/day in severe burns to 10 g/day in the case of an uncomplicated surgical procedure. Accelerated muscle proteolysis results in a loss of lean body mass. Furthermore, there is increased fat catabolism, and lipolysis provides the predominant non-protein source of energy in traumatized patients.
Resting energy expenditure increases after trauma or sepsis, by 20 per cent in long bone fracture to 100 per cent in severe burns and trauma. Most adults require 1750-2500 kcal/day. Indeed, even in undernourished patients, more than 2500 kcal/day is rarely needed, as their BMR is lower. Only in severely traumatized patients, such as those with major burns, is 3000 kcal/day necessary. Most patients need 11-16 g nitrogen/day; rarely is 20 g nitrogen/day needed (protein requirement = 6.25 × nitrogen requirement).
NUTRITIONAL ASSESSMENT
The diagnosis of undernutrition is mainly a clinical one. In many cases, patient weight is suitable to assess nutritional status, with a loss of 10 per cent or more being suggestive of possible undernutrition. However, this can be inaccurate if there are significant changes in body water and does not provide adequate information about body fat or protein stores.
A good dietary history is essential for helping to assess nutritional status. Ask about food intake, including type of food and frequency. A useful screening method is the malnutrition universal screening tool (MUST).
Examination of the patient is also essential, including weight and height. Body mass index (BMI) is a useful indicator of nutrition, with the main exceptions being patients with oedema or dehydration.
Other tests include the following:
Fat assessment Measurement of triceps skin-fold thickness using suitable calipers may be useful but is dependent on operator technique, the presence of oedema and skin pliability.
Skeletal muscle protein Arm muscle circumference (AMC) can be calculated from the mid-arm circumference and triceps skin-fold thickness by the following equation:
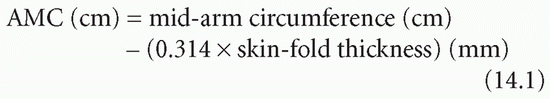
Operator technique may result in inaccuracies in mid-arm circumference measurement.
Hand-grip strength gives indirect evidence of body protein status by looking at muscle strength.
Biochemical tests (these rarely have a major role in assessing nutritional status) Measurement of circulating visceral proteins has been used to assess the impairment of hepatic protein production indirectly. Various plasma proteins have been used:
Albumin: this protein has a plasma half-life of about 20 days but is a poor index of nutritional status as it is influenced by degree of hydration, loss from the body (e.g. gastrointestinal or renal), hepatic well-being and intravascular/extravascular movement (see Chapter 19), and thus has little place as a nutritional marker.
Transferrin: this has a shorter half-life, of about 9 days, and may be a better guide to nutritional status, although it is dependent upon iron status.
Other plasma proteins or peptides that have been studied as potential markers of nutritional status include retinol-binding protein, insulin-like growth factor 1 (IGF-1) and fibronectin, but these are rarely used. Prealbumin, now referred to as transthyretin, may be a marker not so much of poor nutrition but of adequate nutritional replacement when plasma concentrations rise.
Urinary creatinine-to-height ratio can be a measure of lean body mass, but this test has the problem of requiring accurate urine collection.
24-h urinary urea excretion (mmol/L) × 0.034 approximates to urinary nitrogen excretion. This can be used as a guide to nitrogen, and thus protein, requirements, that is, catabolic status.
Complex laboratory tests are available, such as the assessment of total body fat by impedance measurement, or total body nitrogen to assess protein status. However, these are usually used only in research settings and not in routine clinical practice.
Laboratory tests may also show fatty acid deficiencies (see Chapter 13) and/or vitamin and trace element abnormalities (see Chapter 15). Poor nutrition may cause impaired immunological function with decreased lymphocyte count and abnormalities of delayed hypersensitivity.
Prognostic nutritional index
The prognostic nutritional index (PNI) has been devised as a marker of nutritional status and incorporates a number of the components discussed above including plasma albumin and transferrin concentration, skinfold thickness and lymphocyte function.
Subjective global assessment
This looks at a number of subjective weightings on key variables, including weight loss, gastrointestinal disorders, functional capacity and physical signs of deficiency. Weighting A is well nourished, B moderately nourished and C poorly nourished.
UNDERNUTRITION
This starts with reduced intake or nutrient loss. The stores of nutrients are depleted, which leads to biochemical and metabolic consequences and, eventually, clinical symptoms and signs.
Kwashiorkor occurs in individuals with visceral protein loss associated with impaired immunological function, although other nutritional components are satisfactory. Visceral proteins are decreased, but body weight, mid-arm circumference and triceps skin-fold thickness are relatively normal. Conversely, marasmus is generalized undernutrition with reduction in weight, mid-arm circumference and skin-fold thickness, although visceral proteins are relatively normal.
Do not forget that patients can be undernourished while in the hospital ward, particularly the elderly and those who are severely ill, post surgery or in intensive care; alas, about 10-40 per cent of all adults in hospitals or nursing homes may be undernourished.
Nutritional support or artificial nutrition
Nutritional support can take many forms. For example, in coeliac disease (Chapter 16), a gluten-free diet is important, and for lactose intolerance, specific dietary restriction of lactose is required.
Normally, however, whole nutritional support should be considered:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


