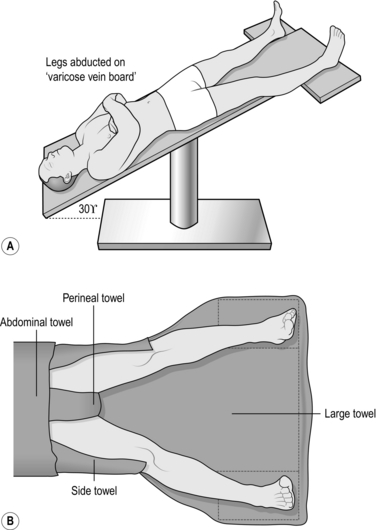
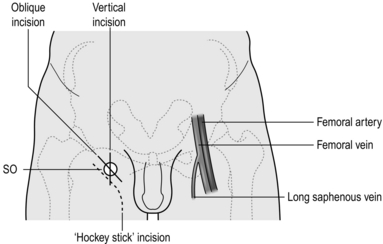
24 ‘Varicose veins’ of the leg are classified according to their size: 1. Trunk (true) varicose veins are large tortuous dilated protruding superficial veins. They result from superficial venous incompetence due to valvular damage. 2. Reticular veins are small (2–3 mm), protrude and do not blanch on pressure. 3. Thread or spider veins are small (<1mm) intradermal subcutaneous veins, which blanch on pressure. Both reticular and thread veins result from alterations in the subcutaneous collagen, probably with local venous incompetence. Venous complications where varicose vein surgery may help include: 1. bleeding from varicose veins, which may occur as a result of trauma from sports, such as rugby, or at the delicate ankle skin secondary to venous hypertension 2. superficial thrombophlebitis which can be secondary to minor trauma to varicose veins as well as other causes such as malignancy. When the thrombus extends to near the saphenofemoral or popliteal junction urgent intervention is indicated to prevent progression. If not, intervention should be considered once the acute phlebitis has settled. 3. Ankle venous hypertensive skin changes. These include frank ulceration as well as lipodermatosclerotic skin thickening with haemosiderin pigmentation; the term does not apply to the age-related development of thread veins at the ankle. Treating any superficial venous incompetence will reduce the risk of ulcer recurrence, although it does not improve the rate of ulcer healing. Varicose veins symptoms where surgery may help include: 1. Aching: Varicose veins produce a deep dull heavy aching fullness in the legs, which comes on when standing and is eased by elevating the leg or wearing support stockings. Any other leg discomfort is probably not due to venous disease, and venous treatment will not improve the discomfort. 2. Throbbing: The varicose veins can throb, and some patients refer to a sensation similar to water trickling down the leg. 3. Itching: The enlarged veins can itch, especially in warm conditions. This is worsened when eczematous skin changes develop. 4. Night cramps: These can be associated with varicose veins, although there are several other causes and intervention is not usually considered if this is the sole symptom. 5. Cosmesis: In Western society, especially amongst women, it is common to expose the legs. 6. Ankle oedema: This can also be associated with varicose veins, although there are many other causes and treatment solely for this symptom should generally be avoided. 1. The symptoms match the signs and therefore the indications for treatment (as outlined above). 2. The veins are primary and not secondary and associated with a vascular malformation or more complex aetiology. Hints that the varicose veins may not be simple and primary include a history of leg fracture; repeated DVTs; venous or leg complications from abdominal surgery and pregnancy; abnormally placed varicose veins (such as laterally along the leg, vulval, or abdominal wall varices); erythematous leg birth marks, leg or foot size discrepancy. Use of the hand held Doppler in the clinic adds little. 3. Magnetic resonance venography (MRV) Reserved for treating (not investigating) complex malformations and pelvic varices. There are three surgical steps to superficial venous disease intervention: 1. Dislocation of the superficial venous system from the deep venous system 2. Removal of the incompetent saphenous vein There are three ways of undertaking steps one and two: 1. Physically removing the saphenous vein (surgical ligation and stripping) 2. Thermally ablating the saphenous vein, the heat coming from an endovenous laser or radiofrequency source 3. Use of a sclerosant chemical to occlude the saphenous vein, which may be endovenous catheter-directed. 1. Carefully re-examine patients admitted for varicose vein surgery. Confirm or exclude incompetence in the long and short saphenous veins and in the calf perforating veins. 2. Skin mark with an arrow the origin of the saphenous vein incompetence in the groin or popliteal fossa. 3. With the patient standing, mark all prominent varicosities with indelible pen as ‘tram-lines’ on either side of the vein to avoid ‘tattooing’ through the incision. 4. Preoperative marking with Duplex scanning is useful for locating the termination of the short saphenous vein and the sites of incompetent perforating veins. 5. Consent the patient for the planned procedure, warning of the risks of recurrent varicose veins, bleeding, wound infection, scarring and numbness from cutaneous nerve neuropraxia. With recurrent varicose veins warn of the risk of worsening ankle oedema. 6. Ensure that the equipment, including the ultrasound machine, is available and working. 1. Have the skin of the groin and leg shaved before the operation. 2. Place the patient supine in the Trendelenburg position with approximately 30° of head-down tilt, both legs abducted by 20° from the midline and the ankles lying on a padded board. This allows easy access and reduces intra-operative haemorrhage (Fig. 24.1). 3. Prepare all exposed surfaces of the limb from the foot to the groin and up to the level of the umbilicus with aqueous 0.5% chlorhexidine acetate solution, while an assistant elevates the leg by lifting the patient’s foot. 1. Make an oblique incision just below and parallel to the inguinal ligament in the groin crease, over the saphenofemoral junction, which is lateral to the femoral pulse and medial to the adductor tendon/pubic tubercle (Fig. 24.2). 2. Deepen the incision through the subcutaneous fat, which is spread by digital retraction, divide Scarpa’s fascia and hold it apart by the insertion of a self-retaining retractor such as West’s. Modify the length of incision depending on the build of the patient. 1. Dissect the long saphenous vein out of the surrounding fat. Pass a controlling large tie around the vein and trace it upwards and towards the saphenofemoral junction. The perivenous plane is simple to open and is bloodless when entered. 2. Dissect out all tributaries that join the long saphenous vein near its termination, ligating them with 3/0 absorbable suture before dividing them. The superficial inferior epigastric vein, the superficial circumflex iliac vein, and the superficial and deep external pudendal veins all join the saphenous trunk near its termination. In addition, the posteromedial and anterolateral thigh veins terminate close to the saphenofemoral junction (Fig. 24.3). One or more of these veins may join together before emptying into the saphenous trunk. 3. After these tributaries have been divided, approach the saphenofemoral junction. The long saphenous vein dips down through the cribriform fascia over the foramen ovale to join the femoral vein. The femoral vein tends to be a lighter colour. Carefully separate the subcutaneous fat from the vein by blunt dissection to follow its path. Display the femoral vein for approximately 1 cm above the saphenofemoral junction, and clear any small tributaries entering from either side. Dissecting the femoral vein downwards risks damaging the superficial external pudendal artery, which may pass either anterior or posterior to the saphenous vein. If damaged, ligate and divide it with impunity. 4. Ligate the long saphenous vein in continuity with 2/0 absorbable suture, flush with the saphenofemoral junction, and divide it. For greater safety doubly ligate or transfix the saphenous stump. Alternatively, oversew the termination with a 3/0 polypropylene continuous suture. 5. Place a strong ligature around the divided distal end of the long saphenous trunk and hold it up to occlude retrograde blood flow, then make a small transverse venotomy below the ligature and introduce a disposable plastic stripper with a blunt tip into the saphenous vein. Gently manipulate the tip of the stripper downwards until it is a hand’s breadth below the knee, where it may remain in the saphenous vein or pass into a tributary (Fig. 24.4). If it will not pass, withdraw the stripper and re-insert it with a rotational action. Tie the ligature at the top end to prevent blood from leaking out of the divided long saphenous trunk. 6. Make a short oblique incision in one of the skin crease tension lines, 1 cm in length, over the palpable tip of the stripper. Ensure that the incision is large enough to allow the head of the stripper to pass. Palpate the vein containing the stripper and dissect it off the saphenous nerve. 7. Make a small side-hole in the vein through which the tip of the stripper can be delivered. Tie the proximal end of the stripper to the long saphenous vein with a strong, long length of suture. 8. Strip the long saphenous vein from the groin to the knee with steady downward traction (invert strip). Ease the stripper and the bunched up vein through the lower incision. Clamp the attached long saphenous vein and any tributaries, divide and ligate it with 2/0 polyglactin. 9. Prevent excessive bleeding from the stripper track by gently rolling a swab along the course of the vein before applying bandages. Some surgeons apply a sterile tourniquet to the leg to prevent excessive haemorrhage. 1. Keep the leg elevated 15° above the horizontal in bed. 2. Encourage early mobilization after applying additional compression bandages over the bandages put on in the theatre. This reduces haematoma formation and provides better support when the patient stands. Thromboembolism prophylaxis stockings do not provide sufficient compression. 3. Advise the patient to walk rather than stand still or sit with the feet down. 4. Discharge fit patients on the day of surgery with advice on compression stockings, exercise and adequate hydration postoperatively. 1. This is indicated if there is gross dilatation and reflux in the short saphenous trunk or its tributaries. 2. The location of the saphenopopliteal junction is very variable and, in a third of cases, the short saphenous vein enters the popliteal vein above or below the middle of the popliteal fossa. 3. Preoperative Duplex scanning and marking of the saphenopopliteal junction provide accurate information about the termination of the short saphenous vein and its proximal tributaries. 4. Carry out short saphenous vein ligation first if you intend to strip the long saphenous vein under the same anaesthetic. 1. Place the patient prone, with pillows under the chest, midriff and pelvis. This demands careful supervision from the anaesthetist to ensure that ventilation is maintained and the patient is safely placed on the operating table with adequate pressure area support. 2. If under general anaesthetic, place the operating table in 30° of head-down tilt and slightly abduct the legs to ease access. 1. Find the short saphenous vein in the popliteal fossa and dissect it from the surrounding fat and accompanying sural nerve, which is usually laterally placed. 2. Follow the short saphenous vein cranially as it dips down to the popliteal vein. Dissecting onto the popliteal vein can be difficult and risks damaging neighbouring structures. It is therefore wise to ligate the saphenous vein with an absorbable 2/0 suture as it dips down, and not at the popliteal vein junction. Ligate the saphenous vein more caudally and divide between the ligatures. Doubly ligate the stump of the short saphenous vein with 2/0 absorbable sutures. 3. In 2.5–10% of patients there is a tributary joining the short saphenous vein from above, known as the vein of Giacomini; carefully divide it between ligatures. 4. Stripping the short saphenous vein is not always undertaken:
Veins and lymphatics
MANAGING LEG SUPERFICIAL VENOUS DISEASE (VARICOSE VEIN SURGERY)
Appraise
 Venous flow: An occluded vein suggests the presence of thrombosis.
Venous flow: An occluded vein suggests the presence of thrombosis.
 Valve competency: Two-directional Doppler flow on calf compression and release indicates incompetence.
Valve competency: Two-directional Doppler flow on calf compression and release indicates incompetence.
 Vein wall compliance: A patent vein that is difficult to compress on direct pressure suggests wall scarring, as occurs following phlebitis or a DVT.
Vein wall compliance: A patent vein that is difficult to compress on direct pressure suggests wall scarring, as occurs following phlebitis or a DVT.
 In complex cases the Duplex ultrasound scan will help define the venous anatomy and distinguish between low and high flow arteriovenous malformations.
In complex cases the Duplex ultrasound scan will help define the venous anatomy and distinguish between low and high flow arteriovenous malformations.
Preparation
HIGH SAPHENOUS VEIN LIGATION (TRENDELENBURG’S OPERATION) AND STRIPPING OF LONG SAPHENOUS VEIN
Prepare
Access
Action
Postoperative
SAPHENOPOPLITEAL LIGATION AND STRIPPING
Appraise
Prepare
Action
 If it is, place a strong ligature around the divided end of the short saphenous trunk and hold it up to occlude retrograde blood flow, make a small transverse venotomy and introduce a disposable plastic stripper into the saphenous vein.
If it is, place a strong ligature around the divided end of the short saphenous trunk and hold it up to occlude retrograde blood flow, make a small transverse venotomy and introduce a disposable plastic stripper into the saphenous vein.
 Gently manipulate the tip of the stripper downwards until it is a hand’s breadth above the lateral maleolus. Make a 1-cm vertical incision in a skin crease tension lines over the palpable stripper tip. Dissect the sural nerve off the vein containing the stripper. Deliver the stripper through the vein.
Gently manipulate the tip of the stripper downwards until it is a hand’s breadth above the lateral maleolus. Make a 1-cm vertical incision in a skin crease tension lines over the palpable stripper tip. Dissect the sural nerve off the vein containing the stripper. Deliver the stripper through the vein.
 Tie the proximal end of the stripper to the short saphenous vein with a strong, long length of suture and strip the saphenous vein with steady downward traction.
Tie the proximal end of the stripper to the short saphenous vein with a strong, long length of suture and strip the saphenous vein with steady downward traction.
 Ease the stripper and the bunched up vein through the lower incision.
Ease the stripper and the bunched up vein through the lower incision.
 Clamp the attached saphenous vein and any tributaries, divide and ligate it with 2/0 polyglactin.
Clamp the attached saphenous vein and any tributaries, divide and ligate it with 2/0 polyglactin.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree