A. Sympatholytics
1. β-Adrenergic blockers are less commonly used as first-line agents in hypertension as other agents may have a better safety profile for this indication in those older than the age of 60 years. β Blockers are indicated for long-term treatment of patients with coronary artery disease and heart failure and for their antihypertensive action in these patients.
a. Mechanism of Action. β Blockers can be classified according to whether they exhibit β1 selective versus nonselective properties and whether they possess intrinsic sympathomimetic activity.
b. Side Effects. Treatment of hypertension with β blockers involves certain risks, including bradycardia and heart block, congestive heart failure, bronchospasm, claudication, masking of hypoglycemia, sedation, impotence, and when abruptly discontinued may precipitate angina pectoris or even myocardial infarction. Patients with any degree of congestive heart failure cannot generally tolerate more than modest doses of β blockers, yet it is clear that when dosage is slowly increased and the drugs are given chronically, the antiadrenergic effect provides a significant benefit in chronic systolic heart failure. In patients with symptomatic asthma, β blockers should be avoided. β Blockers potentially increase the risk of serious hypoglycemia in diabetic patients because they blunt autonomic nervous system responses that would warn of hypoglycemia. Nevertheless, the incidence of hypoglycemia has not been shown to be increased in diabetic patients being treated with β-adrenergic antagonists to control hypertension.
c. Intravenous β Blockers. Perioperative β blockade can be used to continue preoperative therapy, but due to extensive first-pass activity for oral agents, the conversion to intravenous dosing is somewhat unpredictable.
2. α1 Receptor Blockers. Prazosin, terazosin, and doxazocin are oral, selective postsynaptic α1-adrenergic receptor antagonists resulting in vasodilating effects on both arterial and venous vasculature. Absence of presynaptic α2 receptor antagonism leaves intact the normal inhibitory effect on norepinephrine release from nerve endings. In addition to treating essential hypertension, prazosin may be of value for decreasing afterload in patients with congestive heart failure. Prazosin may also be a useful drug for the preoperative preparation of patients with pheochromocytoma.
a. Pharmacokinetics. Prazosin is nearly completely metabolized, and less than 60% bioavailability after oral administration suggests the occurrence of substantial first-pass hepatic metabolism (the fact that this drug is metabolized in the liver permits its use in patients with renal failure without altering the dose).
b. Cardiovascular Effects. Prazosin decreases systemic vascular resistance without causing reflex-induced tachycardia or increases in renin activity as occurs during treatment with hydralazine or minoxidil.
c. Side Effects. The side effects of prazosin include vertigo, fluid retention, and orthostatic hypotension.
3. α2 Agonists. Clonidine is a centrally acting selective partial α2-adrenergic agonist (220:1 α2 to α1 activity) that acts as an antihypertensive drug by virtue of its ability to decrease sympathetic output from the central nervous system. This drug has proved to be particularly effective in the treatment of patients with severe hypertension or renin-dependent disease. The usual daily adult dose is 0.2 to 0.3 mg orally. Another drug of the same class is intravenous dexmedetomidine, a much more α2 selective drug which is approved for sedation rather than hypertension, although it does have a blood pressure–lowering action.
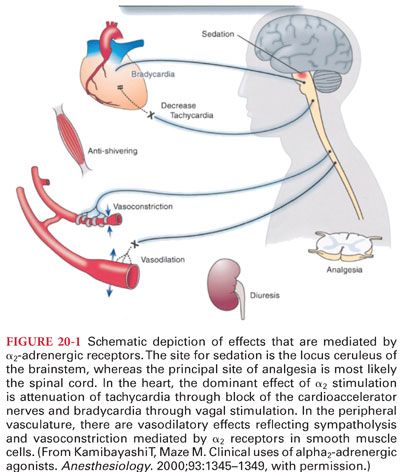
a. Mechanism of Action. α2-Adrenergic agonists produce clinical effects by binding to α2 receptors (Fig. 20-1). Decreased sympathetic nervous system activity is manifested as peripheral vasodilation and decreases in systemic blood pressure, heart rate, and cardiac output.
b. Pharmacokinetics. Clonidine is rapidly absorbed after oral administration and reaches peak plasma concentrations within 60 to 90 minutes. The transdermal route requires about 48 hours to produce steady-state therapeutic plasma concentrations.
c. Cardiovascular Effects. The ability of clonidine to decrease systemic blood pressure without paralysis of compensatory homeostatic reflexes is highly desirable. Renal blood flow and glomerular filtration rate are maintained in the presence of clonidine therapy.
d. Side Effects. The most common side effects produced by clonidine are sedation and xerostomia. Consistent with sedation is a 50% decrease in anesthetic requirements for inhaled anesthetics (minimum alveolar concentration) and injected drugs in patients pretreated with clonidine administered in the preanesthetic medication.
e. Rebound Hypertension. Abrupt discontinuation of clonidine therapy can result in rebound hypertension as soon as 8 hours and as late as 36 hours after the last dose. Rebound hypertension can usually be controlled by reinstituting clonidine therapy or by administering a vasodilating drug such as hydralazine or nitroprusside.
f. Other Clinical Uses. α-Adrenergic agonists (clonidine and dexmedetomidine) induce sedation, decrease anesthetic requirements, and improve perioperative hemodynamic (attenuate blood pressure and heart rate responses to surgical stimulation) and sympathoadrenal stability.
B. ACE inhibitors are most effective in treating systemic hypertension secondary to increased renin production. These drugs have been established as first-line therapy in patients with systemic hypertension, congestive heart failure, and mitral regurgitation.
1. Mechanism of Action. Angiotensin II normally binds to a specific cell membrane receptor (AT1) that ultimately leads to increased release of calcium from sarcoplasmic reticulum to produce vasoconstriction. Administration of ACE inhibitors as prodrugs increases oral bioavailability prior to their hepatic metabolism to the active drug.
2. Side Effects
a. Cough, upper respiratory congestion, rhinorrhea, and allergic-like symptoms seem to be the most common side effects of ACE inhibitors.
b. Decreases in glomerular filtration rate may occur in patients treated with ACE inhibitors.
c. Hyperkalemia is possible due to decreased production of aldosterone. The risk of hyperkalemia is greatest in patients with recognized risk factors (congestive heart failure with renal insufficiency).
3. Preoperative Management
a. Adverse circulatory effects during anesthesia are recognized in patients chronically treated with ACE inhibitors, but continuation of these drugs until the time of surgery is not associated with adverse consequences.
b. Exaggerated hypotension attributed to continued ACE inhibitor therapy has been responsive to crystalloid fluid infusion and/or administration of a catecholamine or vasopressin infusion.
C. Angiotensin II receptor inhibitors produce antihypertensive effects by blocking the vasoconstrictive actions of angiotensin II without affecting ACE activity. As with ACE inhibitors, hypotension following induction of anesthesia has been observed in patients being treated with angiotensin II receptor blockers causing some to recommend these drugs be discontinued on the day before surgery.
D. Calcium Channel Blocking Drugs. Calcium channel blocking drugs used as antihypertensives inhibit calcium influx through the voltage-sensitive L-type calcium channels in vascular smooth muscle. They are arterial specific, with little effect on venous circulation.
E. Phosphodiesterase (PDE) Inhibitors
1. The PDEs variably inhibit the breakdown of intracellular cyclic adenosine monophosphate and cyclic guanosine monophosphate (GMP). The intravenous PDE-3 inhibitor milrinone has replaced amrinone due to its reduced side effect profile. Its combined inotropic and vasodilator actions make it an ideal drug in the short-term treatment of heart failure, both in the intensive care and operative settings.
2. Concurrent administration of nitroglycerin and erectile dysfunction drugs within 24 hours is not recommended as life-threatening hypotension from exaggerated systemic vasodilation may occur.
IV. Nitric Oxide and Nitrovasodilators
A. Nitric Oxide (NO). NO is recognized as a chemical messenger in a multitude of biologic systems, with homeostatic activity in the modulation of cardiovascular tone (synthesized in endothelial cells from the amino acid L-arginine by NO synthetase). NO production has a large role in regulation of vascular tone throughout the body. As a therapeutic agent, inhaled NO (iNO) affects the pulmonary circulation but not the systemic circulation due its extremely rapid uptake by hemoglobin.
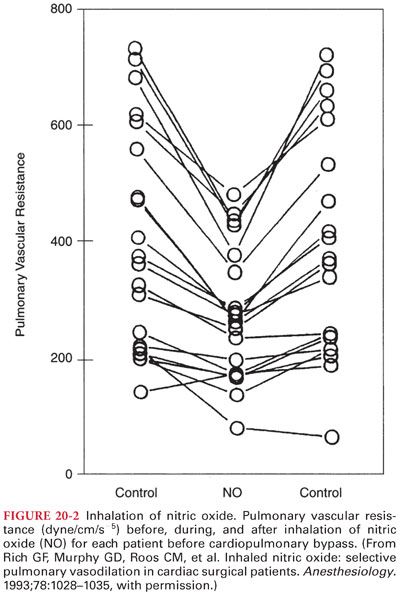
1. NO as a Pulmonary Vasodilator. iNO causes pulmonary arterial vasodilation that is proportional to the degree of pulmonary vasoconstriction (Fig. 20-2). By dilating vessels in alveoli where it is locally delivered, iNO usually improves oxygenation by improving ventilation: perfusion matching. iNO, 10 to 20 ppm, has been used for therapy of persistent pulmonary hypertension of the newborn.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


