Overview
Vessels are the conduits by which blood is distributed to and from the organs. Obstruction or occlusion of vessels leads to ischemia of the organs, which causes cell death (necrosis). The most common cause of obstruction or occlusion of vessels is arteriosclerosis (“hardening of the arteries”).
Pressure within the vessels is determined by a combination of contraction of cardiac muscle and resistance created by the vessels themselves. Changes in this system (e.g., increased vascular resistance) can lead to hypertension, which can cause irreversible damage of the vessels. Examples of structural changes include narrowing of the lumen and dilations of vessels (i.e., aneurysms). Other disorders (e.g., vasculitis) as well as hypertension can cause vascular injury. This chapter will discuss arteriosclerosis and atherosclerosis, systemic hypertension, aortic dissection, pulmonary hypertension, aneurysms, vasculitis, and vascular proliferations.
Arteriosclerosis
Overview: Arteriosclerosis is also known as “hardening” or sclerosis of the arteries and occurs in three main forms, Mönckeberg medial calcification, arteriolosclerosis, and atherosclerosis.
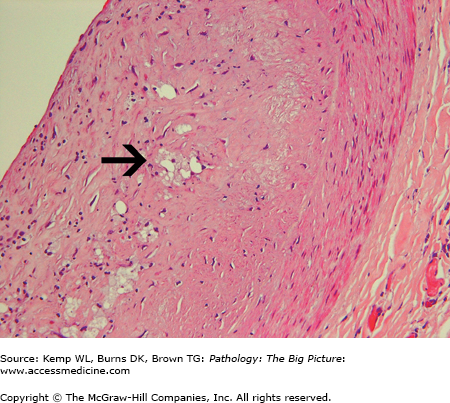
Mönckeberg medial calcification: A condition of little clinical significance because the changes are nonstenotic. It is characterized by medial calcification (“pipestem rigidity”) of the muscular arteries (often radial and ulnar arteries) in elderly men.
Atherosclerosis
Chronic endothelial cell injury by hyperlipidemia, hypertension, toxins in cigarette smoke, elevated levels of homocysteine, and hemodynamic forces (e.g., turbulent blood flow) leads to endothelial cell dysfunction.
Endothelial cells regulate vasodilation and constriction, promote hemostasis, and otherwise prevent thrombosis. Endothelial dysfunction promotes thrombosis and increased permeability as well as allows monocytes and lymphocytes to adhere to the surface and migrate into the intima.
Low-density lipoproteins (LDL) can move into and out of the intima; however, the presence of macrophages (derived from blood monocytes) results in production of enzymes that oxidize LDL. Oxidized LDL is engulfed by macrophages through scavenger receptors.
Finally, smooth muscle cells migrate into the intima: The smooth muscle cells convert from a contractile role in the media to a secretory role in the intima, where they produce extracellular matrix. Smooth muscle cells secrete extracellular matrix components (e.g., collagen) that contribute to the development of plaque. Smooth muscle cells, like macrophages, are capable of engulfing oxidized LDL.
- Atherosclerosis begins as an intimal process; the changes in the media occur secondary to changes in the intima.
- Macrophages that engulf LDL die and release oxidized LDL, causing intracellular and extracellular lipid to accumulate within plaque.
- Elevated levels of high-density lipoproteins (HDL) are protective. HDL removes LDL from the wall of the vessel. Moderate alcohol consumption and exercise have been demonstrated to increase HDL levels.
- Major and modifiable risk factors (i.e., modifiable through changes in lifestyle): Smoking, diabetes mellitus, hypertension, and hyperlipidemia. The term “metabolic syndrome” describes a group of metabolic risk factors that includes insulin-resistance hyperlipidemia, hypertension, and abdominal obesity.
- Major and nonmodifiable risk factors: Male gender (after menopause, female risk for atherosclerosis is the same as that of males), advanced age, and family history, which is usually polygenic in origin.
- Other risk factors: Chlamydia pneumoniae infection, elevated levels of homocysteine, and elevated levels of lipoprotein-a (Lpa). Lpa is similar in shape to plasminogen and thus interferes with the generation of plasmin, predisposing to thrombosis.
- Elastic and medium-sized muscular arteries, most severely at ostia where laminar flow is disrupted. Laminar flow protects vessels from the development of atherosclerosis.
- In general, there is a descending order of prominence of vascular involvement: abdominal aorta (Figure 9-1), coronary arteries, popliteal arteries, internal carotid arteries, and circle of Willis. However, patients with severe coronary artery atherosclerosis can have a relatively disease-free aorta.
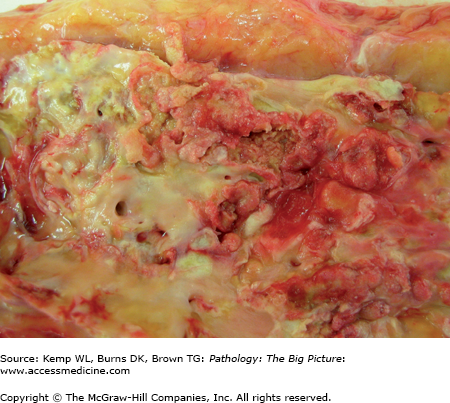
Figure 9-1.
Aortic atherosclerosis. This close-up of the intimal surface of the longitudinally opened aorta reveals severe atherosclerosis. The roughened surface of the aorta is due to innumerable atherosclerotic plaques, which are hemorrhagic and friable. Within the blood stream, a portion of these friable plaques can break free and embolize farther down the vasculature, sometimes producing infarcts.
Overview: The first three complications listed below—occlusion of vessel, disruption of plague, and emboli—can lead to ischemia and infarcts of organs. Aneurysms can lead to rupture of the vessel and resultant hemorrhage. Peripheral vascular disease is a specific condition with characteristic symptoms related to atherosclerosis of the arteries in the lower extremities.
Occlusion of vessel: Symptoms, signs, and results depend upon organ supplied.
Disruption of plaque: Hemorrhage within plaque or rupture or ulceration of plaque (with exposure of the thrombogenic components) can result in thrombus formation.
Emboli: Plaque can break free and be carried in the blood stream farther down the vessel.
Aneurysm: Atherosclerosis begins as an intimal process, but over time the thickened intima puts pressure on and causes atrophy of the media, often resulting in an aneurysm (i.e., dilation or saccular outpouching of the vessel).
Peripheral vascular disease
- Clinical presentation: Claudication, which is characterized by ache or cramping in the extremities with exertion that is relieved by standing still. Patients also have cool extremities, diminished distal pulses, and shiny, hairless skin. Patients with severe peripheral vascular disease have pain at rest. Ischemic ulcerations are a common cause of morbidity.
- Cause: Atherosclerosis of vessels of the lower extremities.
- Clinical presentation: Claudication, which is characterized by ache or cramping in the extremities with exertion that is relieved by standing still. Patients also have cool extremities, diminished distal pulses, and shiny, hairless skin. Patients with severe peripheral vascular disease have pain at rest. Ischemic ulcerations are a common cause of morbidity.
General morphology: Grossly recognizable atherosclerosis begins as a fatty streak and progresses to a fibroatheroma.
- Fatty streak: Intimal accumulation of foam cells (Figure 9-2).
- Atheroma: Intimal accumulation of foam cells and extracellular lipid.
- Fibroatheroma: Atheroma with development of a fibrous cap.
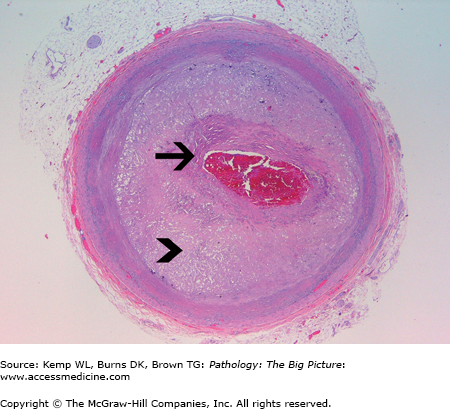
Microscopic morphology of a fibroatheroma: There are three main components of a fibroatheroma (Figure 9-3).
Fibrous cap: A thick fibrous cap is more stable and less likely to develop complications (e.g., hemorrhage or rupture). The fibrous cap is composed of smooth muscle cells and extracellular matrix (e.g., collagen).
Atheromatous core: Contains extracellular lipid, macrophages with intracellular lipid, and necrotic tissue.
Shoulder of plaque: Has macrophages, leukocytes, and blood vessels.
Figure 9-3.
Atherosclerosis, coronary artery. The cross-section of this coronary artery reveals a large atherosclerotic plaque with a thin fibrous cap (arrow) and thick atheromatous core (arrowhead). Currently, the plaque is producing more than 75% stenosis of the lumen of the vessel and most likely resultant ischemia of tissue downstream from the obstruction. Also, atherosclerotic plaques with a thin fibrous cap are prone to rupture, with potential resultant thrombus formation. Hematoxylin and eosin, 20×.
Systemic Hypertension
Basic description: Elevated systemic blood pressure (systolic pressure ≥ 140 mm Hg or diastolic pressure ≥ 90 mm Hg).
Epidemiology: Hypertension occurs in 15–30% of adults. The incidence increases with age (60% of people older than age 65 have hypertension). It is more common in males and in African Americans.
Types of systemic hypertension: Hypertension may be primary (essential), with no underlying cause, or secondary, with an underlying cause. In addition, hypertension can be classified as benign or malignant, depending upon its clinical course and symptoms.
Primary (essential) hypertension: Hypertension not associated with an underlying disease. It represents 90–95% of cases of systemic hypertension.
Secondary hypertension: Hypertension due to another disease process. Causes of secondary hypertension are usually renal, endocrine, cardiac, neurologic, or stress-induced in origin (Table 9-1).
- Renal causes: Often due to activation of the renin-angiotensin-aldosterone system and can be parenchymal and vascular in origin. Renal parenchymal causes include chronic renal failure, acute glomerulonephritis, and renin-producing tumors. Renal vascular causes include renal artery stenosis caused by atherosclerosis or another process (e.g., fibrous dysplasia).
- Endocrine causes: Cushing syndrome, Conn syndrome (aldosterone-secreting tumor), acromegaly, pheochromocytoma, hyperthyroidism, and hypothyroidism.
- Cardiovascular causes: Coarctation of the aorta, polyarteritis nodosa, increased intravascular volume, and increased cardiac output.
- Neurologic causes: Increased intracranial pressure, sleep apnea, acute stress, and brain tumors.
- Stress–induced causes: Pain, anxiety, and hypoglycemia.
Source of Cause of Hypertension by Organ System | Specific Causes |
|---|---|
Renal | Chronic renal failure, acute glomerulonephritis, and renal artery stenosis due to atherosclerosis or fibrous dysplasia |
Endocrine | Both Cushing and Conn syndromes, acromegaly, pheochromocytoma, hyperthyroidism, and hypothyroidism |
Cardiovascular | Coarctation of the aorta, polyarteritis nodosa |
Neurologic | Increased intracranial pressure, sleep apnea, brain tumors |
Idiopathic (“benign”) hypertension: Has a slow clinical course. Patients can survive with the disease for 10–20 years or more. Note, that despite the designation of “benign,” all forms of hypertension are associated with increased morbidity and mortality.
Malignant hypertension: Has a rapid clinical course. Death occurs within 1 to 3 years. Patients have retinal hemorrhage, papilledema, and renal failure. Malignant hypertension can arise in the background of “benign” hypertension, or it can arise de novo.
- Chronic hypertension: Defined as hypertension present prior to 20 weeks’ gestation.
- Gestational hypertension: Defined as hypertension occurring after 20 weeks’ gestation, which resolves within 2 weeks of termination of the pregnancy.
- Preeclampsia (toxemia): Hypertension occurring during the second half of gestation in association with significant (> 300 mg/24 h) proteinuria. Edema is common but is no longer considered a diagnostic criterion. Hyperuricemia is frequently present.
- Severe preeclampsia: Meets the diagnostic criteria for preeclampsia, plus patients have evidence of end-organ dysfunction. Signs and symptoms of severe preeclampsia include oliguria, severe headache, abdominal pain, elevated liver enzymes, thrombocytopenia, and pulmonary and cerebral edema.
- Eclampsia: Meets the diagnostic criteria for severe preeclampsia; also, patients have seizures.
- HELLP syndrome: Form of severe preeclampsia characterized by hemolysis, elevated liver enzymes, and low platelet count (thrombocytopenia).
- Primary hypertension: The pathogenesis of primary (essential) hypertension is complex and the result of many factors. The two main components determining blood pressure are cardiac output and total peripheral resistance. Total peripheral resistance is a balance between vasoconstricting forces (including angiotensin II and catecholamines) and vasodilating forces (including prostaglandins and nitric oxide). Many other factors play a role in primary hypertension, including low pH and hypoxia in certain organs (e.g., kidney).
- Secondary hypertension: The pathogenesis is usually more straightforward than in essential hypertension. For example, if the patient has a pheochromocytoma (tumor of the adrenal medulla), the hypertension results from the elevated level of catecholamines. In renal artery stenosis, hypertension results from the elevated level of renin produced by the kidney because of a perceived low volume state, with an ultimate increase in angiotensin II and aldosterone.
- Atherosclerosis: Hypertension is one of the four major modifiable risk factors.
- Cardiac hypertrophy: Predisposes to sudden death and congestive heart failure. Hypertrophy is a compensatory mechanism, but compensation may ultimately be inadequate to sustain effective cardiac output, resulting in congestive heart failure.
- Intracerebral hemorrhage: Often centered on basal ganglia or thalamus.
- Arteriolosclerosis: Can lead to organ ischemia and most commonly to renal failure.
- Aortic dissection: (see discussion of aortic dissection below).
- Retinopathy.
- Gross: Enlarged heart due to concentric hypertrophy.
- Microscopic
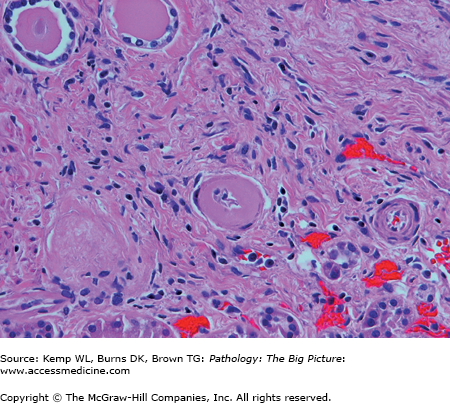
- Hyaline arteriolosclerosis: Associated with benign hypertension. It is eosinophilic, acellular thickening of the wall of arterioles (Figure 9-4).
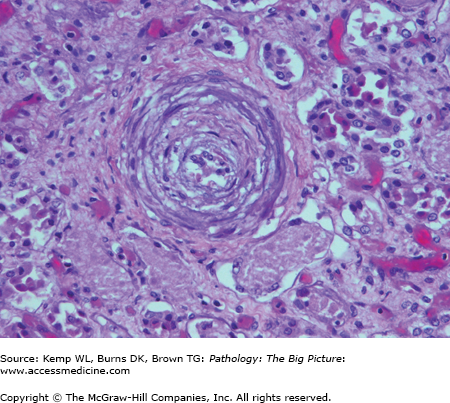
- Hyperplastic arteriolosclerosis: Associated with malignant hypertension. It is a concentric, cellular thickening (i.e., onion-skinning) of the wall associated with fibrinoid necrosis (Figure 9-5).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


- Hyaline arteriolosclerosis: Associated with benign hypertension. It is eosinophilic, acellular thickening of the wall of arterioles (Figure 9-4).