Overview
Diseases of the skin vary from inflammatory disorders to highly malignant neoplasms. This chapter will discuss disorders of pigmentation, melanocytic proliferations (both benign and malignant), other pigmented lesions, non–melanocytic preneoplastic and neoplastic disorders, inherited skin neoplasia syndromes, acute and chronic inflammatory dermatoses, bullous diseases, other inflammatory skin diseases (including erythema nodosum), infectious disorders, and cutaneous manifestations of systemic disorders.
Disorders of Pigmentation
Overview: The three common disorders of pigmentation discussed below are vitiligo, freckles, and lentigo. These disorders represent predominantly cosmetic problems, but rarely may be mistaken for a premalignant lesion.
Morphology
- Gross: Macules or patches of skin with loss of pigment.
- Areas affected: Hands, wrists, and perioral and anogenital regions.
Pathogenesis of vitiligo: Partial or complete loss of melanocytes, possibly of autoimmune etiology.
Important points
- Vitiligo versus albinism: Albinism is lack of melanin pigment due to genetic deficiency of tyrosinase.
- Vitiligo is associated with other autoimmune diseases, and is often seen in patients with Hashimoto thyroiditis, type 1 diabetes mellitus, or Addison disease.
Basic description: Hyperpigmented lesions occurring as a result of an increased amount of melanin pigment.
Important point: A freckle darkens with sunlight.
Melanocytic Proliferations
Overview: Melanocytic proliferations vary from the benign melanocytic nevus to the highly aggressive malignant melanoma.
Basic description: Benign proliferation of nevus cells, which are derived from melanocytes.
Types of melanocytic nevus
- Junctional nevus: Proliferation of nevus cells confined to the basal portion of the epidermis.
- Compound nevus: Proliferation of nevus cells at the basal portion of the epidermis and upper dermis.
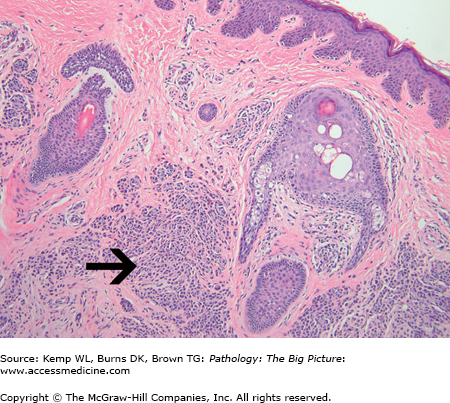
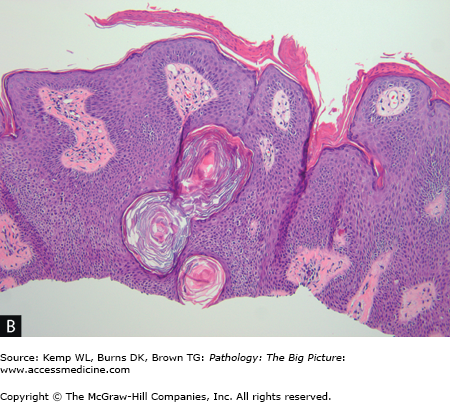
- Intradermal nevus: Proliferation of nevus cells confined to the dermis (Figure 20-1).
Microscopic morphology of melanocytic nevus: Nests of uniform round cells with inconspicuous nucleoli and few if any mitotic figures. As cells get deeper into the dermis, they acquire more of a neural appearance as a result of maturation of the cells.
Basic description: Proliferation of dysplastic nevus cells; dysplastic nevi are precursors of malignant melanoma.
Morphology of dysplastic nevus
- Gross: Variable pigmentation; > 5 mm in size; irregular borders.
- Microscopic: Fusion and coalescence of nests of nevus cells in epidermis. Also, single nevus cells are present in basal portion of epidermis. The nevus cells have cytologic atypia.
Basic description: Malignant tumor of melanocytes.
Four types of malignant melanoma
- Superficial spreading melanoma: Has a radial growth pattern for a significant period of time.
- Lentigo maligna melanoma: Patients are older adults.
- Nodular melanoma: Has a vertical growth pattern early in its development.
- Acral lentiginous melanoma: Affects most commonly the nail bed, the sole of the foot, or the palms in African Americans.
Pathogenesis: Melanomas are caused by ultraviolet radiation that damages the DNA of melanocytes. Mutations in CDKN2A, which alter transcription and cell cycle control, are thought to play a prominent role in melanoma formation.
Growth patterns of melanoma
- Radial: Grows horizontally; not associated with metastases.
- Vertical: Grows downward into the dermis; is associated with metastases.
Risk factors for melanoma: Sun exposure, especially in fair skinned individuals. Although melanomas do not often arise from nevi, a history of atypical nevi, giant nevi (> 20 cm), or a large number of nevi are risk factors for melanoma.
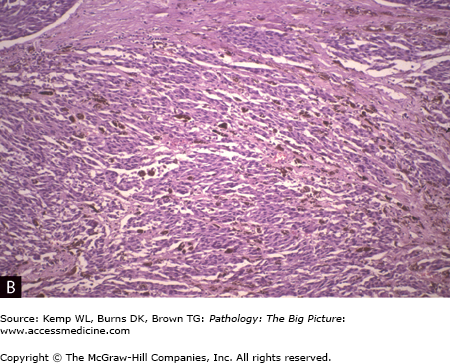
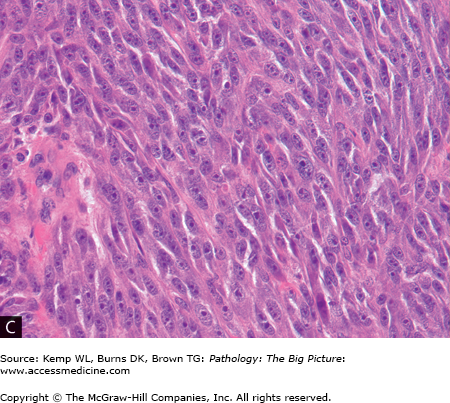
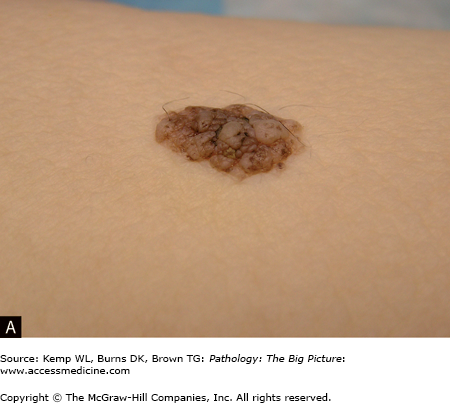
Morphology of melanoma (Figure 20-2 A–C)
- Gross: > 10 mm in size, variable pigmentation (can be hypopigmented), irregular borders.
- Microscopic: Large cells with prominent nucleoli forming poorly defined nests; single cells are present. Neoplastic cells may or may not produce melanin.
- Important point: For staging of a melanoma, depth of penetration into the dermis is crucial. The greater the depth of penetration, the more likelihood of metastases.
Figure 20-2.
Malignant melanoma. A, This patient had two large, untreated and undiagnosed nodular malignant melanomas on her back. Malignant melanoma often produces pigment, which can be seen grossly as well as microscopically (B). However, not all malignant melanomas produce pigment, and this tumor must always be considered in the diagnosis of malignancies with large pleomorphic cells and prominent nucleoli (C). Hematoxylin and eosin, B, 200×; C, 400×.
Clinical presentation of malignant melanoma
- Warning signs of melanoma: Increasing size of nevus; itching and/or pain; change in size, shape, or color of nevus; growth of new nevus; irregular borders.
- Favorable prognostic factors: Depth of invasion (Breslow depth) of < 1.7 mm; absence of mitotic figures.
Important point: S-100 and HMB-45 are commonly used tumor markers for melanoma.
Other Pigmented Lesions
Morphology (Figure 20-3 A and B)
- Gross: Tan to dark brown papule or nodule with a “stuck-on” appearance.
- Microscopic: Sheets of basal-like cells, hyperkeratosis, and keratin-filled cysts.
Epidemiology: Middle-aged and older adults.
Sign of Leser-Trélat: Sudden onset of multiple seborrheic keratoses, which is a cutaneous manifestation of internal malignancy (associated with adenocarcinoma of the gastrointestinal tract).
Morphology (Figure 20-4)
- Gross and microscopic: Hyperplastic (i.e., acanthosis) and hyperpigmented papules.
- Areas affected: Flexor regions, including the posterior neck, axilla, and groin.
Types of acanthosis nigricans
- Benign: Commonly associated with insulin resistance and obesity.
- Malignant: Can be a cutaneous manifestation of internal malignancy (associated with gastrointestinal adenocarcinoma).
Non—Melanocytic Preneoplastic and Neoplastic Lesions
Morphology
- Gross: Rough, sandpaper-like lesion, which may have a keratin horn.
- Microscopic: Dysplasia of keratinocytes in basal portion of epidermis; can have parakeratosis.
Risk factor: Actinic keratoses are caused by exposure to ultraviolet light and exposure to sun.
Important point: Actinic keratosis is a precancerous lesion that has the potential to develop into squamous cell carcinoma.
Mutations: Commonly of p53 gene.
Risk factors: Sun exposure; older patients. Other risk factors include chronic ulcers, osteomyelitis, and burns (Marjolin ulcer).
Incidence: Second most common type of skin cancer (80–100,000 cases per year).
Important point: Cutaneous squamous cell carcinoma rarely metastasizes (only 5% of cases metastasize). Multiple squamous cell carcinomas may arise at the sites of arsenic exposure.
Precursors of cutaneous squamous cell carcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree