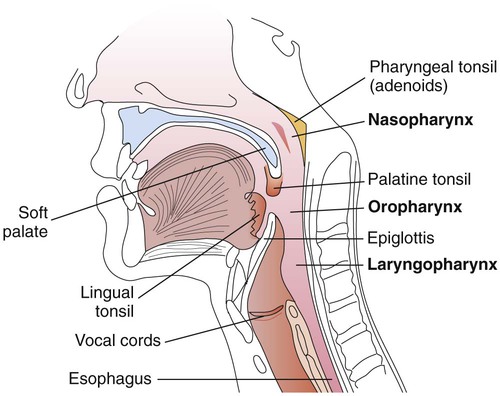
1. Explain the anatomy and structures of the upper respiratory tract, including the three parts of the pharynx. 2. Identify the principal causative organism of pharyngitis; name other organisms capable of causing pharyngitis. 3. Define the following conditions: laryngitis, epiglottis, and parotitis. List the etiologic organisms associated with these conditions. 4. Explain the pathogenic mechanisms (virulence factors) associated with Streptococcus pyogenes pharyngitis. 5. Define Vincent’s angina and peritonsillar abscesses. What organism do they share as the causative agent of disease? 6. Describe the disease process caused by pharyngeal infection with Corynebacterium diphtheriae; name the hallmark symptom of this infection and list the complications associated with infection. 7. Differentiate between stomatitis and thrush, and explain the testing process for each disease. 8. Outline the steps used in the culture of specimens for the isolation of Streptococcus pyogenes. 9. Explain the signs and symptoms and pathogenic mechanisms associated with disease caused by Bordetella pertussis. What special requirements are needed to detect this organism in culture? 10. List three types of periodontal infections that require culture to identify the causative agent of infection; name the bacteria associated with these infections. 11. Explain the unique characteristics of C and G streptococcus, and explain how they contribute to their pathogenesis. The respiratory tract is generally divided into two regions, the upper and the lower. The upper respiratory tract includes all the structures down to the larynx: the sinuses, throat, nasal cavity, epiglottis, and larynx; the throat is also called the pharynx. These anatomic structures are shown in Figure 70-1. The pharynx is a tubelike structure that extends from the base of the skull to the esophagus (see Figure 70-1). Made of muscle, this structure is divided into three parts: • Nasopharynx (portion of the pharynx above the soft palate) • Oropharynx (portion of the pharynx between the soft palate and epiglottis) • Laryngopharynx (portion of the pharynx below the epiglottis that opens into the larynx) An overview of the pathogenesis of respiratory tract infections is presented in Chapter 69. It is important to keep in mind that upper respiratory tract infections may spread and become more serious because the mucosa (mucous membrane) of the upper tract is continuous with the mucosal lining of the sinuses, eustachian tube, middle ear, and lower respiratory tract. Although different bacteria can cause pharyngitis or tonsillitis, the primary cause of bacterial pharyngitis is Streptococcus pyogenes (or group A beta-hemolytic streptococci). Viral pharyngitis or other causes of pharyngitis/tonsillitis must be differentiated from that caused by S. pyogenes, because pharyngitis resulting from S. pyogenes is treatable with penicillin and a variety of other anti-microbials, whereas viral infections are not. In addition, treatment is of particular importance because infection with S. pyogenes can lead to complications such as acute rheumatic fever and glomerulonephritis. These complications are referred to as poststreptococcal sequelae (diseases that follow a streptococcal infection) and are primarily immunologically mediated; these sequelae are discussed in greater detail in Chapter 15. S. pyogenes may also cause pyogenic infections (suppurations) of the tonsils, sinuses, and middle ear, or cellulitis as secondary pyogenic sequelae after an episode of pharyngitis. Accordingly, streptococcal pharyngitis is usually treated to prevent both the suppurative and nonsuppurative sequelae, as well as to decrease morbidity. Although bacteria other than group A streptococci may cause pharyngitis, this occurs less often. Large colony isolates of groups C and G streptococci (classified as Streptococcus dysgalactiae subsp. equisimilis) are pyogenic streptococci with similar virulence traits as S. pyogenes; symptoms of pharyngitis caused by these agents are also similar to S. pyogenes. In contrast to S. pyogenes, these agents are rarely associated with poststreptococcal sequelae, namely glomerulonephritis and possibly rheumatic fever. Recent studies have demonstrated that these streptococci can exchange genetic information with S. pyogenes and thus potentially obtain virulence factors usually associated with S. pyogenes such as M proteins, streptolysin O, and superantigen genes. Arcanobacterium haemolyticum is also a cause of pharyngitis among adolescents. Examples of agents that can cause pharyngitis or tonsillitis are listed in Table 70-1. TABLE 70-1 Examples of Bacteria That Can Cause Acute Pharyngitis and/or Tonsillitis Rhinitis (common cold) is an inflammation of the nasal mucous membrane or lining. Depending on the host response and the etiologic agent, rhinitis is characterized by variable fever, increased mucous secretions, inflammatory edema of the nasal mucosa, sneezing, and watery eyes. With rare exceptions, rhinitis is typically associated with viral infections (20%-25%); some of these agents are listed in Box 70-1. Rhinitis is common because of the large number of different causative viruses, and reinfections may occur. Bacterial agents associated with rhinitis (10%-15%) include Chlamydia pneumoniae, Mycoplasma pneumoniae, and Group A streptococci. Pharyngitis caused by Corynebacterium diphtheriae is less common than streptococcal pharyngitis. After an incubation period of 2 to 4 days, diphtheria usually presents as pharyngitis or tonsillitis. Patients are often febrile and complain of sore throat and malaise (body discomfort). The hallmark for diphtheria is the presence of an exudate or membrane that is usually on the tonsils or pharyngeal wall. The gray-white membrane is a result of the action of diphtheria toxin on the epithelium at the site of infection. Complications occur frequently with diphtheria and are usually seen during the last stage of the disease (paroxysmal stage). The most feared complications are those involving the central nervous system such as seizures, coma, or blindness. Information as to how this organism causes disease is discussed in Chapter 69. Additional specifics regarding this organism are provided in Chapter 17.
Upper Respiratory Tract Infections and Other Infections of the Oral Cavity and Neck
General Considerations
Anatomy
Pathogenesis
Diseases of the Upper Respiratory Tract, Oral Cavity, and Neck
Upper Respiratory Tract
Pharyngitis, Tonsillitis, and Peritonsillar Abscesses
Pharyngitis and Tonsillitis.
Epidemiology/Etiologic Agents.
Organism
Disease
Relative Frequency
Streptococcus pyogenes
Pharyngitis/tonsillitis/rheumatic fever/scarlet fever
15% to 35%
Group C and G beta-hemolytic streptococci
Pharyngitis/tonsillitis
<3% to 11%
Arcanobacterium (Corynebacterium) haemolyticum
Pharyngitis/tonsillitis/rash
<1% to 10%
Neisseria gonorrhoeae
Pharyngitis/disseminated disease
Rare*
Corynebacterium ulcerans
Pharyngitis
Rare
Mycoplasma pneumoniae
Pneumonia/bronchitis/pharyngitis
Rare
Yersinia enterocolitica
Pharyngitis/enterocolitis
Rare
Human immunodeficiency virus-1
Pharyngitis/acute retroviral disease
Rare
Rhinitis
Miscellaneous Infections Caused by Other Agents.
Corynebacterium diphtheriae.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Upper Respiratory Tract Infections and Other Infections of the Oral Cavity and Neck