It is now appreciated that genotypes of T. gondii prevalent in South America may be more virulent than those typically seen in North America or Europe. These genotypes may be associated with acute or recurrent ocular disease in immunocompetent individuals and have also been associated with pneumonitis and a fulminant sepsis picture in immunologically normal individuals. Thus a detailed history is critical for establishing a diagnosis.
The results of routine laboratory studies are usually unremarkable except for minimal lymphocytosis, an elevated erythrocyte sedimentation rate, and a nominal increase in serum aminotransferase levels. Evaluation of cerebrospinal fluid (CSF) in cases with evidence of encephalopathy or meningoencephalitis shows an elevation of intracranial pressure, mononuclear pleocytosis (10–50 cells/mL), a slight increase in protein concentration, and (occasionally) an increase in the gamma globulin level. PCR amplification of the Toxoplasma DNA target sequence in CSF may be beneficial. The CSF of chronically infected individuals is normal.
Infection of Immunocompromised Patients Patients with AIDS and those receiving immunosuppressive therapy for lymphoproliferative disorders are at greatest risk for developing acute toxoplasmosis. Toxoplasmosis has also been reported after treatment with antibodies to tumor necrosis factor. The infection may be due either to reactivation of latent infection or to acquisition of parasites from exogenous sources such as blood or transplanted organs. In individuals with AIDS, >95% of cases of Toxoplasma encephalitis (TE) are believed to be due to recrudescent infection. In most of these cases, encephalitis develops when the CD4+ T cell count falls below 100/µL. In immunocompromised hosts, the disease may be rapidly fatal if untreated. Thus, accurate diagnosis and initiation of appropriate therapy are necessary to prevent fulminant infection.
Toxoplasmosis is a principal opportunistic infection of the CNS in persons with AIDS. Although geographic origin may be related to frequency of infection, it has no correlation with the severity of disease in immunocompromised hosts. Individuals with AIDS who are seropositive for T. gondii are at high risk for encephalitis. Before the advent of current cART, about one-third of the 15–40% of adult AIDS patients in the United States who were latently infected with T. gondii developed TE. TE may still be a presenting infection in individuals who are unaware of their positive HIV status.
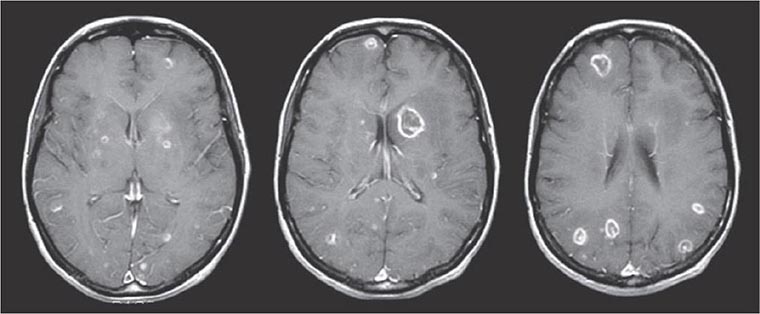
The signs and symptoms of acute toxoplasmosis in immunocompromised patients principally involve the CNS (Fig. 253-2). More than 50% of patients with clinical manifestations have intracerebral involvement. Clinical findings at presentation range from nonfocal to focal dysfunction. CNS findings include encephalopathy, meningoencephalitis, and mass lesions. Patients may present with altered mental status (75%), fever (10–72%), seizures (33%), headaches (56%), and focal neurologic findings (60%), including motor deficits, cranial nerve palsies, movement disorders, dysmetria, visual-field loss, and aphasia. Patients who present with evidence of diffuse cortical dysfunction develop evidence of focal neurologic disease as infection progresses. This altered condition is due not only to the necrotizing encephalitis caused by direct invasion by the parasite but also to secondary effects, including vasculitis, edema, and hemorrhage. The onset of infection can range from an insidious process over several weeks to an acute presentation with fulminant focal deficits, including hemiparesis, hemiplegia, visual-field defects, localized headache, and focal seizures.
FIGURE 253-2 Toxoplasmic encephalitis in a 36-year-old patient with AIDS. The multiple lesions are demonstrated by MRI scanning (T1-weighted with gadolinium enhancement). (Courtesy of Clifford Eskey, Dartmouth Hitchcock Medical Center, Hanover, NH; with permission.)
Although lesions can occur anywhere in the CNS, the areas most often involved appear to be the brainstem, basal ganglia, pituitary gland, and corticomedullary junction. Brainstem involvement gives rise to a variety of neurologic dysfunctions, including cranial nerve palsy, dysmetria, and ataxia. With basal ganglionic infection, patients may develop hydrocephalus, choreiform movements, and choreoathetosis. Toxoplasma usually causes encephalitis, and meningeal involvement is uncommon. CSF findings may be unremarkable or may include a modest increase in cell count and in protein—but not glucose—concentration. Nonetheless, the parasite may be detected by PCR in CSF from many patients with TE.
Cerebral toxoplasmosis must be differentiated from other opportunistic infections or tumors in the CNS of AIDS patients. The differential diagnosis includes herpes simplex encephalitis, cryptococcal meningitis, progressive multifocal leukoencephalopathy, and primary CNS lymphoma. Involvement of the pituitary gland can give rise to panhypopituitarism and hyponatremia from inappropriate secretion of vasopressin (antidiuretic hormone). HIV-associated neurocognitive disorder (HAND) may present as cognitive impairment, attention loss, and altered memory. Brain biopsy in patients who have been treated for TE but who continue to exhibit neurologic dysfunction often fails to identify organisms.
Autopsies of Toxoplasma-infected patients have demonstrated the involvement of multiple organs, including the lungs, gastrointestinal tract, pancreas, skin, eyes, heart, and liver. Toxoplasma pneumonia can be confused with Pneumocystis pneumonia (PcP). Respiratory involvement usually presents as dyspnea, fever, and a nonproductive cough and may rapidly progress to acute respiratory failure with hemoptysis, metabolic acidosis, hypotension, and (occasionally) disseminated intravascular coagulation. Histopathologic studies demonstrate necrosis and a mixed cellular infiltrate. The presence of organisms is a helpful diagnostic indicator, but organisms can also be found in healthy tissue. Infection of the heart is usually asymptomatic but can be associated with cardiac tamponade or biventricular failure. Infections of the gastrointestinal tract and the liver have been documented.
Congenital Toxoplasmosis Between 400 and 4000 infants born each year in the United States are affected by congenital toxoplasmosis. Acute infection in mothers acquiring T. gondii during pregnancy is usually asymptomatic; most such women are diagnosed via prenatal serologic screening. Infection of the placenta leads to hematogenous infection of the fetus. As gestation proceeds, the proportion of fetuses that become infected increases, but the clinical severity of the infection declines. Although infected children may initially be asymptomatic, the persistence of T. gondii can result in reactivation and clinical disease—most frequently chorioretinitis—decades later. Factors associated with relatively severe disabilities include delays in diagnosis and in initiation of therapy, neonatal hypoxia and hypoglycemia, profound visual impairment (see “Ocular Infection,” below), uncorrected hydrocephalus, and increased intracranial pressure. If treated appropriately, upwards of 70% of children have normal developmental, neurologic, and ophthalmologic findings at follow-up evaluations. Treatment for 1 year with pyrimethamine, a sulfonamide, and folinic acid is tolerated with minimal toxicity (see “Treatment,” below).
![]() Ocular Infection Infection with T. gondii is estimated to cause 35% of all cases of chorioretinitis in the United States and Europe. It was formerly thought that the majority of cases of ocular disease were due to congenital infection. New ocular toxoplasmosis in immunocompetent individuals occurs more commonly than was previously appreciated and has been associated with outbreaks in Victoria (British Columbia) and in South America. A variety of ocular manifestations are documented, including blurred vision, scotoma, photophobia, and eye pain. Macular involvement occurs, with loss of central vision, and nystagmus is secondary to poor fixation. Involvement of the extraocular muscles may lead to disorders of convergence and to strabismus. Ophthalmologic examination should be undertaken in newborns with suspected congenital infection. As the inflammation resolves, vision improves, but episodic flare-ups of chorioretinitis, which progressively destroy retinal tissue and lead to glaucoma, are common. The ophthalmologic examination reveals yellow-white, cotton-like patches with indistinct margins of hyperemia. As the lesions age, white plaques with distinct borders and black spots within the retinal pigment become more apparent. Lesions usually are located near the posterior pole of the retina; they may be single but are more commonly multiple. Congenital lesions may be unilateral or bilateral and show evidence of massive chorioretinal degeneration with extensive fibrosis. Surrounding these areas of involvement are a normal retina and vasculature. In patients with AIDS, retinal lesions are often large, with diffuse retinal necrosis, and include both free tachyzoites and cysts containing bradyzoites. Toxoplasmic chorioretinitis may be a prodrome to the development of encephalitis.
Ocular Infection Infection with T. gondii is estimated to cause 35% of all cases of chorioretinitis in the United States and Europe. It was formerly thought that the majority of cases of ocular disease were due to congenital infection. New ocular toxoplasmosis in immunocompetent individuals occurs more commonly than was previously appreciated and has been associated with outbreaks in Victoria (British Columbia) and in South America. A variety of ocular manifestations are documented, including blurred vision, scotoma, photophobia, and eye pain. Macular involvement occurs, with loss of central vision, and nystagmus is secondary to poor fixation. Involvement of the extraocular muscles may lead to disorders of convergence and to strabismus. Ophthalmologic examination should be undertaken in newborns with suspected congenital infection. As the inflammation resolves, vision improves, but episodic flare-ups of chorioretinitis, which progressively destroy retinal tissue and lead to glaucoma, are common. The ophthalmologic examination reveals yellow-white, cotton-like patches with indistinct margins of hyperemia. As the lesions age, white plaques with distinct borders and black spots within the retinal pigment become more apparent. Lesions usually are located near the posterior pole of the retina; they may be single but are more commonly multiple. Congenital lesions may be unilateral or bilateral and show evidence of massive chorioretinal degeneration with extensive fibrosis. Surrounding these areas of involvement are a normal retina and vasculature. In patients with AIDS, retinal lesions are often large, with diffuse retinal necrosis, and include both free tachyzoites and cysts containing bradyzoites. Toxoplasmic chorioretinitis may be a prodrome to the development of encephalitis.
DIAGNOSIS
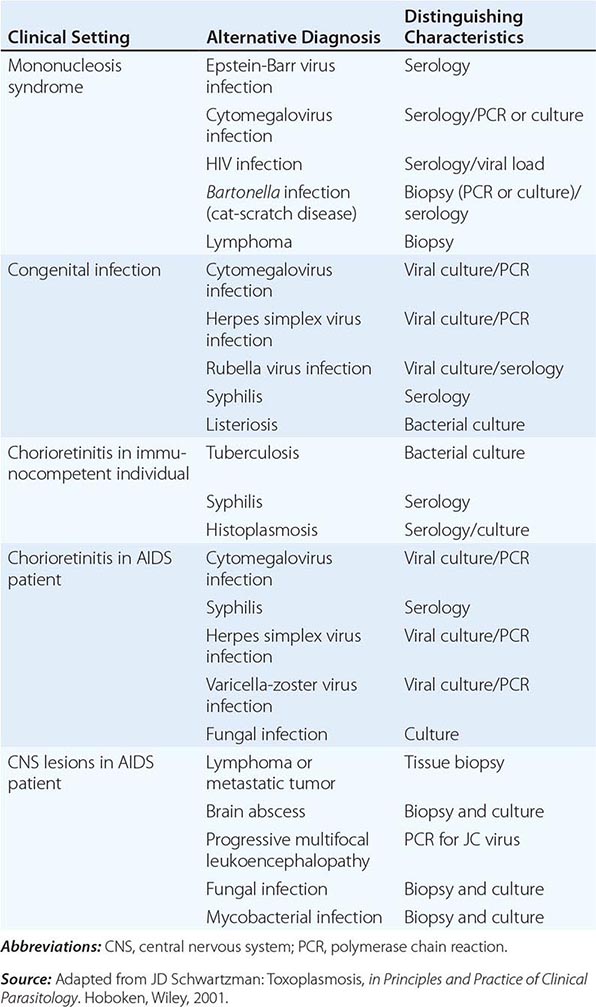
Tissue and Body Fluids The differential diagnosis of acute toxoplasmosis can be made by appropriate culture, serologic testing, and PCR (Table 253-1). Although available only at specialized laboratories, the isolation of T. gondii from blood or other body fluids can be accomplished after subinoculation of the sample into the peritoneal cavity of mice. If no parasites are found in the mouse’s peritoneal fluid 6–10 days after inoculation, its anti-Toxoplasma serum titer can be evaluated 4–6 weeks after inoculation. Isolation of T. gondii from the patient’s body fluids reflects acute infection, whereas isolation from biopsied tissue is an indication only of the presence of tissue cysts and should not be misinterpreted as evidence of acute toxoplasmosis. Persistent parasitemia in patients with latent, asymptomatic infection is rare. Histologic examination of lymph nodes may suggest the characteristic changes described above. Demonstration of tachyzoites in lymph nodes establishes the diagnosis of acute toxoplasmosis. Like subinoculation into mice, histologic demonstration of cysts containing bradyzoites confirms prior infection with T. gondii but is nondiagnostic for acute infection.
DIFFERENTIAL LABORATORY DIAGNOSIS OF TOXOPLASMOSIS |
Serology The procedures mentioned above have great diagnostic value but are limited by difficulties encountered either in the growth of parasites in vivo or in the identification of tachyzoites by histochemical methods. Serologic testing has become the routine method of diagnosis.
Diagnosis of acute infection with T. gondii can be established by detection of the simultaneous presence of IgG and IgM antibodies to Toxoplasma in serum. The presence of circulating IgA favors the diagnosis of an acute infection. The Sabin-Feldman dye test, the indirect fluorescent antibody test, and the enzyme-linked immunosorbent assay (ELISA) all satisfactorily measure circulating IgG antibody to Toxoplasma. Positive IgG titers (>1:10) can be detected as early as 2–3 weeks after infection. These titers usually peak at 6–8 weeks and decline slowly to a new baseline level that persists for life. Antibody avidity increases with time and can be useful in difficult cases during pregnancy for establishing when infection may have occurred. The serum IgM titer should be measured in concert with the IgG titer to better establish the time of infection; either the double-sandwich IgM-ELISA or the IgM-immunosorbent assay (IgM-ISAGA) should be used. Both assays are specific and sensitive, with fewer false-positive results than other commercial tests. The double-sandwich IgA-ELISA is more sensitive than the IgM-ELISA for detecting congenital infection in the fetus and newborn. Although a negative IgM result with a positive IgG titer indicates distant infection, IgM can persist for >1 year and should not necessarily be considered a reflection of acute disease. If acute toxoplasmosis is suspected, a more extensive panel of serologic tests can be performed. In the United States, testing is available at the Toxoplasma Serology Laboratory at Palo Alto Medical Foundation (http://www.pamf.org/serology/clinicianguide.html).
Molecular Diagnostics Molecular approaches can directly detect T. gondii in biologic samples independent of the serologic response. Results obtained with PCR have suggested high sensitivity, specificity, and clinical utility in the diagnosis of TE, and PCR technology may be becoming more readily available in resource-poor settings. Real-time PCR is a promising technique that can provide quantitative results. Isolates can be genotyped and polymorphic sequences can be obtained, with consequent identification of the precise strain. Molecular epidemiologic studies with polymorphic markers have been useful in correlating clinical signs and symptoms of disease with different T. gondii genotypes.
The Immunocompetent Adult or Child For the patient who presents with lymphadenopathy only, a positive IgM titer is an indication of acute infection—and an indication for therapy, if clinically warranted (see “Treatment,” below). The serum IgM titer should be determined again in 3 weeks. An elevation in the IgG titer without an increase in the IgM titer suggests that infection is present but is not acute. If there is a borderline increase in either IgG or IgM, the titers should be reassessed in 3–4 weeks.
The Immunocompromised Host A presumptive clinical diagnosis of TE in patients with AIDS is based on clinical presentation, history of exposure (as evidenced by positive serology), and radiologic evaluation. To detect latent infection with T. gondii, HIV-infected persons should be tested for IgG antibody to Toxoplasma soon after HIV infection is diagnosed. When these criteria are used, the predictive value is as high as 80%. More than 97% of patients with AIDS and toxoplasmosis have IgG antibody to T. gondii in serum. IgM serum antibody usually is not detectable. Although IgG titers do not correlate with active infection, serologic evidence of infection virtually always precedes the development of TE. It is therefore important to determine the Toxoplasma antibody status of all patients infected with HIV. Antibody titers may range from negative to 1:1024 in patients with AIDS and TE. Fewer than 3% of patients have no demonstrable antibody to Toxoplasma at diagnosis of TE.
Patients with TE have focal or multifocal abnormalities demonstrable by CT or MRI. Neuroradiologic evaluation should include double-dose contrast CT of the head. By this test, single and frequently multiple contrast-enhancing lesions (<2 cm) may be identified. MRI usually demonstrates multiple lesions located in both hemispheres, with the basal ganglia and corticomedullary junction most commonly involved; MRI provides a more sensitive evaluation of the efficacy of therapy than does CT (Fig. 253-2). These findings are not pathognomonic of Toxoplasma infection, because 40% of CNS lymphomas are multifocal and 50% are ring-enhancing. For both MRI and CT scans, the rate of false-negative results is ~10%. The finding of a single lesion on an MRI scan increases the likelihood of primary CNS lymphoma (in which solitary lesions are four times more likely than in TE) and strengthens the argument for the performance of a brain biopsy. A therapeutic trial of anti-Toxoplasma medications is frequently used to assess the diagnosis. Treatment of presumptive TE with pyrimethamine plus sulfadiazine or clindamycin results in quantifiable clinical improvement in >50% of patients by day 3. Leucovorin is administered to prevent bone marrow toxicity. By day 7, >90% of treated patients show evidence of improvement. In contrast, if patients fail to respond or have lymphoma, clinical signs and symptoms worsen by day 7. Patients in this category require brain biopsy with or without a change in therapy. This procedure can now be performed by a stereotactic CT-guided method that reduces the potential for complications. Brain biopsy for T. gondii identifies organisms in 50–75% of cases. PCR amplification of CSF may also confirm toxoplasmosis or suggest alternative diagnoses (Table 253-1), such as progressive multifocal leukoencephalopathy (JC virus positive) or primary CNS lymphoma (Epstein-Barr virus positive).
CT and MRI with contrast are currently the standard diagnostic imaging tests for TE. As in other conditions, the radiologic response may lag behind the clinical response. Resolution of lesions may take from 3 weeks to 6 months. Some patients show clinical improvement despite worsening radiographic findings.
Congenital Infection The issue of concern when a pregnant woman has evidence of recent T. gondii infection is whether the fetus is infected. PCR analysis of the amniotic fluid for the B1 gene of T. gondii has replaced fetal blood sampling. Serologic diagnosis is based on the persistence of IgG antibody or a positive IgM titer after the first week of life (a time frame that excludes placental leak). The IgG determination should be repeated every 2 months. An increase in IgM beyond the first week of life is indicative of acute infection. Up to 25% of infected newborns may be seronegative and have normal routine physical examinations. Thus assessment of the eye and the brain, with ophthalmologic testing, CSF evaluation, and radiologic studies, is important in establishing the diagnosis.
Ocular Toxoplasmosis The serum antibody titer may not correlate with the presence of active lesions in the fundus, particularly in cases of congenital toxoplasmosis. In general, a positive IgG titer (measured in undiluted serum if necessary) in conjunction with typical lesions establishes the diagnosis. Antibody production in ocular fluids, expressed in terms of the Goldmann-Witmer coefficient, has been described for diagnosis of ocular disease but does not always correlate with PCR results. If lesions are atypical and the serum antibody titer is in the low-positive range, the diagnosis is presumptive. The parasitic antigen–specific polyclonal IgG assay as well as parasite-specific PCR may facilitate the diagnosis. Accordingly, the clinical diagnosis of ocular toxoplasmosis can be supported in 60–90% of cases by laboratory tests, depending on the time of anterior chamber puncture and the panel of antibody analyses used. In the remaining cases, the possibility of a falsely negative laboratory diagnosis or of an incorrect clinical diagnosis cannot be clarified further.
PREVENTION
All HIV-infected persons should be counseled regarding sources of Toxoplasma infection. The chances of primary infection with Toxoplasma can be reduced by not eating undercooked meat and by avoiding oocyst-contaminated material (i.e., a cat’s litter box). Specifically, lamb, beef, and pork should be cooked to an internal temperature of 165°–170°F; from a more practical perspective, meat cooked until it is no longer pink inside usually satisfies this requirement. Hands should be washed thoroughly after work in the garden, and all fruits and vegetables should be washed. Ingestion of raw shellfish is a risk factor for toxoplasmosis, given that the filter-feeding mechanism of clams and mussels concentrates oocysts.
If the patient owns a cat, the litter box should be cleaned or changed daily, preferably by an HIV-negative, nonpregnant person; alternatively, patients should wash their hands thoroughly after changing the litter box. Litter boxes should be changed daily if possible, as freshly excreted oocysts will not have sporulated and will not be infectious. Patients should be encouraged to keep their cats inside and not to adopt or handle stray cats. Cats should be fed only canned or dried commercial food or well-cooked table food, not raw or undercooked meats. Patients need not be advised to part with their cats or to have their cats tested for toxoplasmosis. Blood intended for transfusion into Toxoplasma-seronegative immunocompromised individuals should be screened for antibody to T. gondii. Although such serologic screening is not routinely performed, seronegative women should be screened for evidence of infection several times during pregnancy if they are exposed to environmental conditions that put them at risk for infection with T. gondii. HIV-positive individuals should adhere closely to these preventive measures.
254 | Protozoal Intestinal Infections and Trichomoniasis |
PROTOZOAL INFECTIONS
GIARDIASIS
![]() Giardia intestinalis (also known as G. lamblia or G. duodenalis) is a cosmopolitan protozoal parasite that inhabits the small intestines of humans and other mammals. Giardiasis is one of the most common parasitic diseases in both developed and developing countries worldwide, causing both endemic and epidemic intestinal disease and diarrhea.
Giardia intestinalis (also known as G. lamblia or G. duodenalis) is a cosmopolitan protozoal parasite that inhabits the small intestines of humans and other mammals. Giardiasis is one of the most common parasitic diseases in both developed and developing countries worldwide, causing both endemic and epidemic intestinal disease and diarrhea.
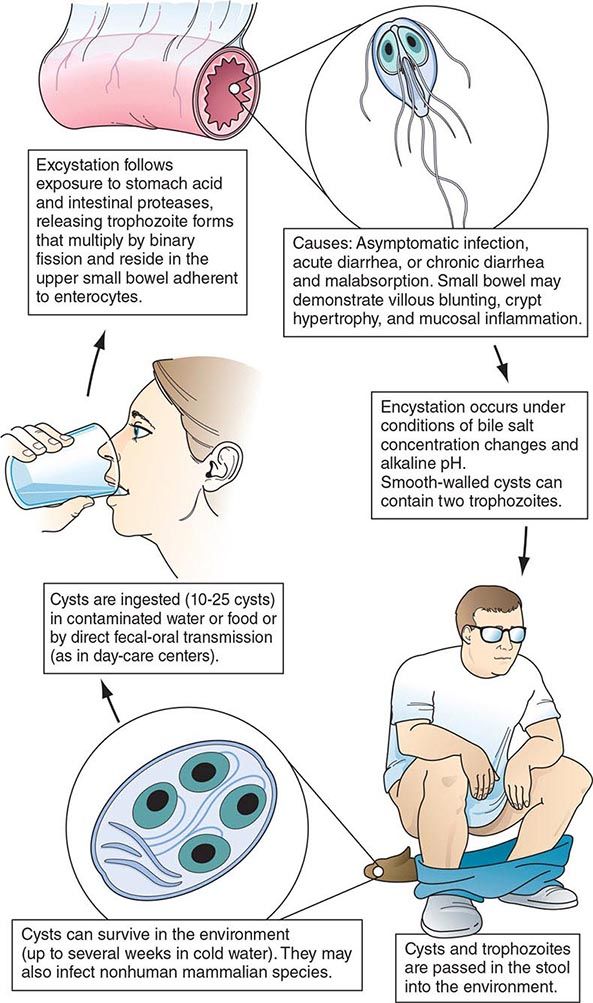
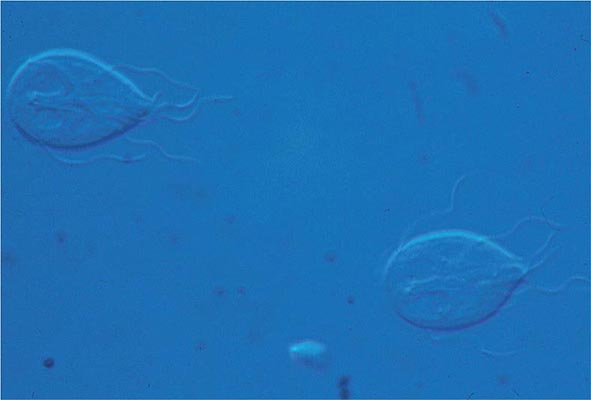
Life Cycle and Epidemiology (Fig. 254-1) Infection follows the ingestion of environmentally hardy cysts, which excyst in the small intestine, releasing flagellated trophozoites (Fig. 254-2) that multiply by binary fission. Giardia remains a pathogen of the proximal small bowel and does not disseminate hematogenously. Trophozoites remain free in the lumen or attach to the mucosal epithelium by means of a ventral sucking disk. As a trophozoite encounters altered conditions, it forms a morphologically distinct cyst, which is the stage of the parasite usually found in the feces. Trophozoites may be present and even predominate in loose or watery stools, but it is the resistant cyst that survives outside the body and is responsible for transmission. Cysts do not tolerate heating or desiccation, but they do remain viable for months in cold fresh water. The number of cysts excreted varies widely but can approach 107 per gram of stool.
FIGURE 254-1 Life cycle of Giardia. (Reprinted with permission from RL Guerrant et al [eds]: Tropical Infectious Diseases: Principles, Pathogens and Practice, 2nd ed, p 987. © 2006, with permission from Elsevier Science.)
FIGURE 254-2 Flagellated, binucleate Giardia trophozoites.
Ingestion of as few as 10 cysts is sufficient to cause infection in humans. Because cysts are infectious when excreted, person-to-person transmission occurs where fecal hygiene is poor. Giardiasis is especially prevalent in day-care centers; person-to-person spread also takes place in other institutional settings with poor fecal hygiene and during anal-oral contact. If food is contaminated with Giardia cysts after cooking or preparation, food-borne transmission can occur. Waterborne transmission accounts for episodic infections (e.g., in campers and travelers) and for major epidemics in metropolitan areas. Surface water, ranging from mountain streams to large municipal reservoirs, can become contaminated with fecally derived Giardia cysts. The efficacy of water as a means of transmission is enhanced by the small infectious inoculum of Giardia, the prolonged survival of cysts in cold water, and the resistance of cysts to killing by routine chlorination methods that are adequate for controlling bacteria. Viable cysts can be eradicated from water by either boiling or filtration.
![]() In the United States, Giardia (like Cryptosporidium; see below) is a common cause of waterborne epidemics of gastroenteritis. Giardia is common in developing countries, and infections may be acquired by travelers.
In the United States, Giardia (like Cryptosporidium; see below) is a common cause of waterborne epidemics of gastroenteritis. Giardia is common in developing countries, and infections may be acquired by travelers.
There are several recognized genotypes or assemblages of G. intestinalis. Human infections are due to assemblages A and B, whereas other assemblages are more common in other animals, including cats and dogs. Like beavers from reservoirs implicated in epidemics, dogs and cats have been found to be infected with assemblages A and B, an observation suggesting that these animals might be sources of human infection.
Giardiasis, like cryptosporidiosis, creates a significant economic burden because of the costs incurred in the installation of water filtration systems required to prevent waterborne epidemics, in the management of epidemics that involve large communities, and in the evaluation and treatment of endemic infections.
Pathophysiology The reasons that some, but not all, infected patients develop clinical manifestations and the mechanisms by which Giardia causes alterations in small-bowel function are largely unknown. Although trophozoites adhere to the epithelium, they are not invasive but may elicit apoptosis of enterocytes, epithelial barrier dysfunction, and epithelial cell malabsorption and secretion. Consequent lactose intolerance and, in a minority of infected adults and children, significant malabsorption are clinical signs of the loss of brush-border enzyme activities. In most infections, the morphology of the bowel is unaltered; however, in chronically infected, symptomatic patients, the histopathologic findings (including flattened villi) and the clinical manifestations at times resemble those of tropical sprue and gluten-sensitive enteropathy. The pathogenesis of diarrhea in giardiasis is not known.
The natural history of Giardia infection varies markedly. Infections may be aborted, transient, recurrent, or chronic. G. intestinalis parasites vary genotypically, and such variations might contribute to different courses of infection. Parasite as well as host factors may be important in determining the course of infection and disease. Both cellular and humoral responses develop in human infections, but their precise roles in disease pathogenesis and/or control of infection are unknown. Because patients with hypogammaglobulinemia suffer from prolonged, severe infections that are poorly responsive to treatment, humoral immune responses appear to be important. The greater susceptibilities of the young than of the old and of newly exposed persons than of chronically exposed populations suggest that at least partial protective immunity may develop.
Clinical Manifestations Disease manifestations of giardiasis range from asymptomatic carriage to fulminant diarrhea and malabsorption. Most infected persons are asymptomatic, but in epidemics the proportion of symptomatic cases may be higher. Symptoms may develop suddenly or gradually. In persons with acute giardiasis, symptoms develop after an incubation period that lasts at least 5–6 days and usually 1–3 weeks. Prominent early symptoms include diarrhea, abdominal pain, bloating, belching, flatus, nausea, and vomiting. Although diarrhea is common, upper intestinal manifestations such as nausea, vomiting, bloating, and abdominal pain may predominate. The duration of acute giardiasis is usually >1 week, although diarrhea often subsides. Individuals with chronic giardiasis may present with or without having experienced an antecedent acute symptomatic episode. Diarrhea is not necessarily prominent, but increased flatus, loose stools, sulfurous belching, and (in some instances) weight loss occur. Symptoms may be continual or episodic and may persist for years. Some persons who have relatively mild symptoms for long periods recognize the extent of their discomfort only in retrospect. Fever, the presence of blood and/or mucus in the stools, and other signs and symptoms of colitis are uncommon and suggest a different diagnosis or a concomitant illness. Symptoms tend to be intermittent yet recurring and gradually debilitating, in contrast with the acute disabling symptoms associated with many enteric bacterial infections. Because of the less severe illness and the propensity for chronic infections, patients may seek medical advice late in the course of the illness; however, disease can be severe, resulting in malabsorption, weight loss, growth retardation, and dehydration. A number of extraintestinal manifestations have been described, such as urticaria, anterior uveitis, and arthritis; whether these are caused by giardiasis or concomitant processes is unclear.
Giardiasis can be severe in patients with hypogammaglobulinemia and can complicate other preexisting intestinal diseases, such as that occurring in cystic fibrosis. In patients with AIDS, Giardia can cause enteric illness that is refractory to treatment.
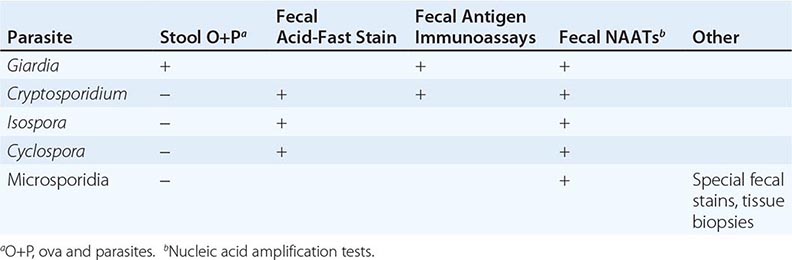
Diagnosis (Table 254-1) Giardiasis is diagnosed by detection of parasite antigens in the feces, by identification of cysts in the feces or of trophozoites in the feces or small intestines, or by nucleic acid amplification tests (NAATs). Cysts are oval, measure 8–12 μm × 7–10 μm, and characteristically contain four nuclei. Trophozoites are pear-shaped, dorsally convex, flattened parasites with two nuclei and four pairs of flagella (Fig. 254-2). The diagnosis is sometimes difficult to establish. Direct examination of fresh or properly preserved stools as well as concentration methods should be used. Because cyst excretion is variable and may be undetectable at times, repeated examination of stool, sampling of duodenal fluid, and biopsy of the small intestine may be required to detect the parasite. Tests for parasitic antigens in stool are at least as sensitive and specific as good microscopic examinations and are easier to perform. Newer NAATs are highly sensitive but are not always available for clinical use at present.
DIAGNOSIS OF INTESTINAL PROTOZOAL INFECTIONS |
Prevention Giardiasis can be prevented by consumption of uncontaminated food and water and by personal hygiene during the provision of care for infected children. Boiling or filtering potentially contaminated water prevents infection.
CRYPTOSPORIDIOSIS
![]() The coccidian parasite Cryptosporidium causes diarrheal disease that is self-limited in immunocompetent human hosts but can be severe in persons with AIDS or other forms of immunodeficiency. Two species of Cryptosporidium, C. hominis (especially in the United States, sub-Saharan Africa, and Asia) and C. parvum (in Europe), cause most human infections.
The coccidian parasite Cryptosporidium causes diarrheal disease that is self-limited in immunocompetent human hosts but can be severe in persons with AIDS or other forms of immunodeficiency. Two species of Cryptosporidium, C. hominis (especially in the United States, sub-Saharan Africa, and Asia) and C. parvum (in Europe), cause most human infections.
Life Cycle and Epidemiology Cryptosporidium species are widely distributed in the world. Cryptosporidiosis is acquired by the consumption of oocysts (50% infectious dose: ~132 C. parvum oocysts in nonimmune individuals), which excyst to liberate sporozoites that in turn enter and infect intestinal epithelial cells. The parasite’s further development involves both asexual and sexual cycles, which produce forms capable of infecting other epithelial cells and of generating oocysts that are passed in the feces. Cryptosporidium species infect a number of animals, and C. parvum can spread from infected animals to humans. Since oocysts are immediately infectious when passed in feces, person-to-person transmission takes place in day-care centers and among household contacts and medical providers. Waterborne transmission (especially that of C. hominis) accounts for infections in travelers and for common-source epidemics. Oocysts are quite hardy and resist killing by routine chlorination. Both drinking water and recreational water (e.g., pools, waterslides) have been increasingly recognized as sources of infection.
Pathophysiology Although intestinal epithelial cells harbor cryptosporidia in an intracellular vacuole, the means by which secretory diarrhea is elicited remain uncertain. No characteristic pathologic changes are found by biopsy. The distribution of infection can be spotty within the principal site of infection, the small bowel. Cryptosporidia are found in the pharynx, stomach, and large bowel of some patients and at times in the respiratory tract. Especially in patients with AIDS, involvement of the biliary tract can cause papillary stenosis, sclerosing cholangitis, or cholecystitis.
Clinical Manifestations Asymptomatic infections can occur in both immunocompetent and immunocompromised hosts. In immunocompetent persons, symptoms develop after an incubation period of ~1 week and consist principally of watery nonbloody diarrhea, sometimes in conjunction with abdominal pain, nausea, anorexia, fever, and/or weight loss. In these hosts, the illness usually subsides after 1–2 weeks. In contrast, in immunocompromised hosts (especially those with AIDS and CD4+ T cell counts <100/μL), diarrhea can be chronic, persistent, and remarkably profuse, causing clinically significant fluid and electrolyte depletion. Stool volumes may range from 1 to 25 L/d. Weight loss, wasting, and abdominal pain may be severe. Biliary tract involvement can manifest as mid-epigastric or right-upper-quadrant pain.
Diagnosis (Table 254-1) Evaluation starts with fecal examination for small oocysts, which are smaller (4–5 μm in diameter) than the fecal stages of most other parasites. Because conventional stool examination for ova and parasites (O+P) does not detect Cryptosporidium, specific testing must be requested. Detection is enhanced by evaluation of stools (obtained on multiple days) by several techniques, including modified acid-fast and direct immunofluorescent stains and enzyme immunoassays. Newer NAATs are being employed. Cryptosporidia can also be identified by light and electron microscopy at the apical surfaces of intestinal epithelium from biopsy specimens of the small bowel and, less frequently, the large bowel.
CYSTOISOSPORIASIS
The coccidian parasite Cystoisospora belli causes human intestinal disease. Infection is acquired by the consumption of oocysts, after which the parasite invades intestinal epithelial cells and undergoes both sexual and asexual cycles of development. Oocysts excreted in stool are not immediately infectious but must undergo further maturation.
Although C. belli infects many animals, little is known about the epidemiology or prevalence of this parasite in humans. It is most common in tropical and subtropical countries. Acute infections can begin abruptly with fever, abdominal pain, and watery nonbloody diarrhea and can last for weeks or months. In patients who have AIDS or are immunocompromised for other reasons, infections often are not self-limited but rather resemble cryptosporidiosis, with chronic, profuse watery diarrhea. Eosinophilia, which is not found in other enteric protozoan infections, may be detectable. The diagnosis (Table 254-1) is usually made by detection of the large (~25-μm) oocysts in stool by modified acid-fast staining. Oocyst excretion may be low-level and intermittent; if repeated stool examinations are unrevealing, sampling of duodenal contents by aspiration or small-bowel biopsy (often with electron microscopic examination) may be necessary. NAATs are promising newer diagnostic tools.
CYCLOSPORIASIS
![]() Cyclospora cayetanensis, a cause of diarrheal illness, is globally distributed: illness due to C. cayetanensis has been reported in the United States, Asia, Africa, Latin America, and Europe. The epidemiology of this parasite has not yet been fully defined, but waterborne transmission and food-borne transmission (e.g., by basil, sweet peas, and imported raspberries) have been recognized. The full spectrum of illness attributable to Cyclospora has not been delineated. Some infected patients may be without symptoms, but many have diarrhea, flulike symptoms, and flatulence and belching. The illness can be self-limited, can wax and wane, or, in many cases, can involve prolonged diarrhea, anorexia, and upper gastrointestinal symptoms, with sustained fatigue and weight loss in some instances. Diarrheal illness may persist for >1 month. Cyclospora can cause enteric illness in patients infected with HIV.
Cyclospora cayetanensis, a cause of diarrheal illness, is globally distributed: illness due to C. cayetanensis has been reported in the United States, Asia, Africa, Latin America, and Europe. The epidemiology of this parasite has not yet been fully defined, but waterborne transmission and food-borne transmission (e.g., by basil, sweet peas, and imported raspberries) have been recognized. The full spectrum of illness attributable to Cyclospora has not been delineated. Some infected patients may be without symptoms, but many have diarrhea, flulike symptoms, and flatulence and belching. The illness can be self-limited, can wax and wane, or, in many cases, can involve prolonged diarrhea, anorexia, and upper gastrointestinal symptoms, with sustained fatigue and weight loss in some instances. Diarrheal illness may persist for >1 month. Cyclospora can cause enteric illness in patients infected with HIV.
The parasite is detectable in epithelial cells of small-bowel biopsy samples and elicits secretory diarrhea by unknown means. The absence of fecal blood and leukocytes indicates that disease due to Cyclospora is not caused by destruction of the small-bowel mucosa. The diagnosis (Table 254-1) can be made by detection of spherical 8- to 10-μm oocysts in the stool, although routine stool O+P examinations are not sufficient. Specific fecal examinations must be requested to detect the oocysts, which are variably acid-fast and are fluorescent when viewed with ultraviolet light microscopy. Newer NAATs are proving to be sensitive. Cyclosporiasis should be considered in the differential diagnosis of prolonged diarrhea, with or without a history of travel by the patient to other countries.
MICROSPORIDIOSIS
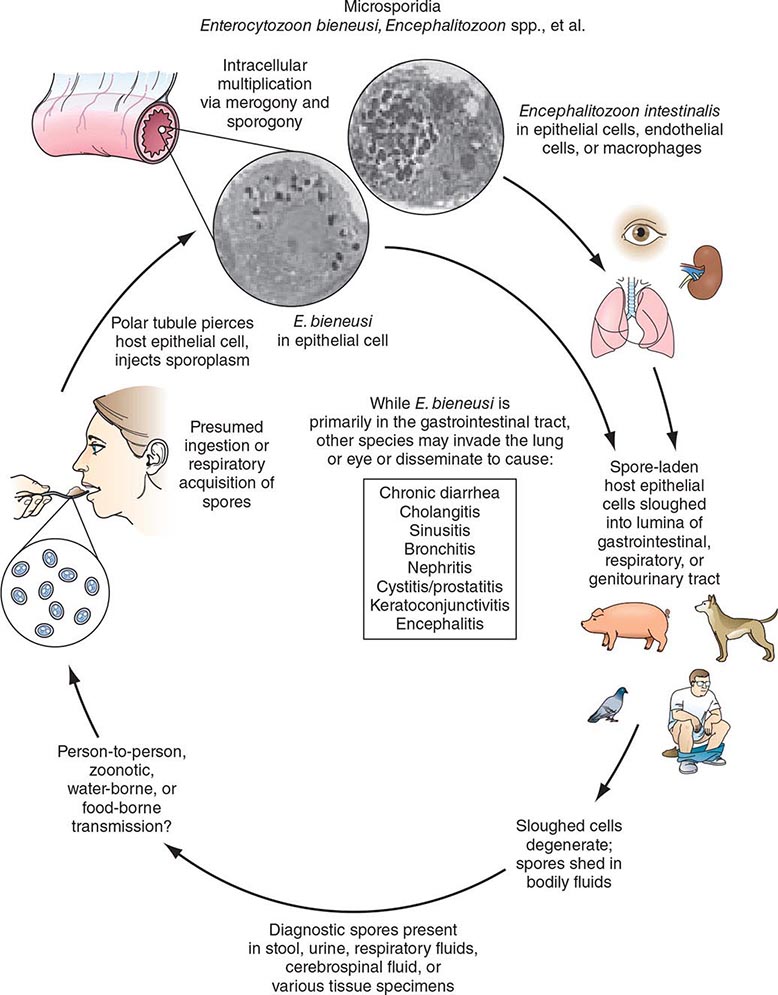
Microsporidia are obligate intracellular spore-forming protozoa that infect many animals and cause disease in humans, especially as opportunistic pathogens in AIDS. Microsporidia are members of a distinct phylum, Microspora, which contains dozens of genera and hundreds of species. The various microsporidia are differentiated by their developmental life cycles, ultrastructural features, and molecular taxonomy based on ribosomal RNA. The complex life cycles of the organisms result in the production of infectious spores (Fig. 254-3). Currently, eight genera of microsporidia—Encephalitozoon, Pleistophora, Nosema, Vittaforma, Trachipleistophora, Anncalia, Microsporidium, and Enterocytozoon—are recognized as causes of human disease. Although some microsporidia are probably prevalent causes of self-limited or asymptomatic infections in immunocompetent patients, little is known about how microsporidiosis is acquired.
FIGURE 254-3 Life cycle of microsporidia. (Reprinted with permission from RL Guerrant et al [eds]: Tropical Infectious Diseases: Principles, Pathogens and Practice, 2nd ed, p 1128. © 2006, with permission from Elsevier Science.)
Microsporidiosis is most common among patients with AIDS, less common among patients with other types of immunocompromise, and rare among immunocompetent hosts. In patients with AIDS, intestinal infections with Enterocytozoon bieneusi and Encephalitozoon (formerly Septata) intestinalis are recognized to contribute to chronic diarrhea and wasting; these infections had been found in 10–40% of patients with chronic diarrhea. Both organisms have been found in the biliary tracts of patients with cholecystitis. E. intestinalis may also disseminate to cause fever, diarrhea, sinusitis, cholangitis, and bronchiolitis. In patients with AIDS, Encephalitozoon hellem has caused superficial keratoconjunctivitis as well as sinusitis, respiratory tract disease, and disseminated infection. Myositis due to Pleistophora has been documented. Nosema, Vittaforma, and Microsporidium have caused stromal keratitis associated with trauma in immunocompetent patients.
Microsporidia are small gram-positive organisms with mature spores measuring 0.5–2 μm × 1–4 μm. Diagnosis of microsporidial infections in tissue often requires electron microscopy, although intracellular spores can be visualized by light microscopy with hematoxylin and eosin, Giemsa, or tissue Gram’s stain. For the diagnosis of intestinal microsporidiosis, modified trichrome or chromotrope 2R-based staining and Uvitex 2B or calcofluor fluorescent staining reveal spores in smears of feces or duodenal aspirates. Definitive therapies for microsporidial infections remain to be established. For superficial keratoconjunctivitis due to E. hellem, topical therapy with fumagillin suspension has shown promise (Chap. 246e). For enteric infections with E. bieneusi and E. intestinalis in HIV-infected patients, therapy with albendazole may be efficacious (Chap. 246e).
OTHER INTESTINAL PROTOZOA
![]() Balantidiasis Balantidium coli is a large ciliated protozoal parasite that can produce a spectrum of large-intestinal disease analogous to amebiasis. The parasite is widely distributed in the world. Since it infects pigs, cases in humans are more common where pigs are raised. Infective cysts can be transmitted from person to person and through water, but many cases are due to the ingestion of cysts derived from porcine feces in association with slaughtering, with use of pig feces for fertilizer, or with contamination of water supplies by pig feces.
Balantidiasis Balantidium coli is a large ciliated protozoal parasite that can produce a spectrum of large-intestinal disease analogous to amebiasis. The parasite is widely distributed in the world. Since it infects pigs, cases in humans are more common where pigs are raised. Infective cysts can be transmitted from person to person and through water, but many cases are due to the ingestion of cysts derived from porcine feces in association with slaughtering, with use of pig feces for fertilizer, or with contamination of water supplies by pig feces.
Ingested cysts liberate trophozoites, which reside and replicate in the large bowel. Many patients remain asymptomatic, but some have persisting intermittent diarrhea, and a few develop more fulminant dysentery. In symptomatic individuals, the pathology in the bowel—both gross and microscopic—is similar to that seen in amebiasis, with varying degrees of mucosal invasion, focal necrosis, and ulceration. Balantidiasis, unlike amebiasis, only rarely spreads hematogenously to other organs. The diagnosis is made by detection of the trophozoite stage in stool or sampled colonic tissue. Tetracycline (500 mg four times daily for 10 days) is an effective therapeutic agent.
Blastocystosis Blastocystis hominis remains an organism of uncertain pathogenicity. Some patients who pass B. hominis in their stools are asymptomatic, whereas others have diarrhea and associated intestinal symptoms. Diligent evaluation reveals other potential bacterial, viral, or protozoal causes of diarrhea in some but not all patients with symptoms. Because the pathogenicity of B. hominis is uncertain and because therapy for Blastocystis infection is neither specific nor uniformly effective, patients with prominent intestinal symptoms should be fully evaluated for other infectious causes of diarrhea. If diarrheal symptoms associated with Blastocystis are prominent, either metronidazole (750 mg thrice daily for 10 days) or TMP-SMX (160 mg/800 mg twice daily for 7 days) can be used.
Dientamoebiasis Dientamoeba fragilis is unique among intestinal protozoa in that it has a trophozoite stage but not a cyst stage. How trophozoites survive to transmit infection is not known. When symptoms develop in patients with D. fragilis infection, they are generally mild and include intermittent diarrhea, abdominal pain, and anorexia. The diagnosis is made by the detection of trophozoites in stool; the lability of these forms accounts for the greater yield when fecal samples are preserved immediately after collection. Since fecal excretion rates vary, examination of several samples obtained on alternate days increases the rate of detection. Iodoquinol (650 mg three times daily for 20 days) or paromomycin (25–35 mg/kg per day in three doses for 7 days) is appropriate for treatment.
TRICHOMONIASIS
Various species of trichomonads can be found in the mouth (in association with periodontitis) and occasionally in the gastrointestinal tract. Trichomonas vaginalis—one of the most prevalent protozoal parasites in the United States—is a pathogen of the genitourinary tract and a major cause of symptomatic vaginitis (Chap. 163).
Life Cycle and Epidemiology T. vaginalis is a pear-shaped, actively motile organism that measures about 10 × 7 μm, replicates by binary fission, and inhabits the lower genital tract of females and the urethra and prostate of males. In the United States, it accounts for ~3 million infections per year in women. While the organism can survive for a few hours in moist environments and could be acquired by direct contact, person-to-person venereal transmission accounts for virtually all cases of trichomoniasis. Its prevalence is greatest among persons with multiple sexual partners and among those with other sexually transmitted diseases (Chap. 163).
Clinical Manifestations Many men infected with T. vaginalis are asymptomatic, although some develop urethritis and a few have epididymitis or prostatitis. In contrast, infection in women, which has an incubation period of 5–28 days, is usually symptomatic and manifests with malodorous vaginal discharge (often yellow), vulvar erythema and itching, dysuria or urinary frequency (in 30–50% of patients), and dyspareunia. These manifestations, however, do not clearly distinguish trichomoniasis from other types of infectious vaginitis.
Diagnosis Detection of motile trichomonads by microscopic examination of wet mounts of vaginal or prostatic secretions has been the conventional means of diagnosis. Although this approach provides an immediate diagnosis, its sensitivity for the detection of T. vaginalis is only ~50–60% in routine evaluations of vaginal secretions. Direct immunofluorescent antibody staining is more sensitive (70–90%) than wet-mount examinations. T. vaginalis can be recovered from the urethra of both males and females and is detectable in males after prostatic massage. A new NAAT, APTIMA, is FDA approved and is highly sensitive and specific for urine and for endocervical and vaginal swabs from women.
SECTION 19 | HELMINTHIC INFECTIONS |
255e | Introduction to Helminthic Infections |
The word helminth is derived from the Greek helmins (“parasitic worm”). Helminthic worms are highly prevalent and, depending on the species, may exist as free-living organisms or as parasites of plant or animal hosts. The parasitic helminths have co-evolved with specific mammalian and other host species. Accordingly, most helminthic infections are restricted to nonhuman hosts, and only rarely do these zoonotic helminths accidentally cause human infections.
Helminthic parasites of humans belong to two phyla: Nemathelminthes, which includes nematodes (roundworms), and Platyhelminthes, which includes cestodes (tapeworms) and trematodes (flukes). Helminthic parasites of humans reside within the human body and hence are the cause of true infections. In contrast, parasites of other genera that reside only on mucocutaneous surfaces of humans (e.g., the parasites causing myiasis and scabies) are considered to represent infestations rather than infections.
Helminthic parasites differ substantially from protozoan parasites in several respects. First, protozoan parasites are unicellular organisms, whereas helminthic parasites are multicellular worms that possess differentiated organ systems. Second, helminthic parasites have complex life cycles that require sequential stages of development outside the human host. Thus, most helminths do not complete their replication within the human host; rather, they develop to a certain stage within the mammalian host and, as part of their obligatory life cycle, must mature further outside that host. During the “extra-human” stages of their life cycle, helminths exist either as free-living organisms or as parasites within another host species and thereafter mature into new developmental stages capable of infecting humans. Thus, with only two exceptions (Strongyloides stercoralis and Capillaria philippinensis, which are capable of internal reinfection), increases in the number of adult helminths (i.e., the “worm burden”) within the human host require repeated exogenous reinfections. In the case of protozoan parasites, a brief, even singular exposure (e.g., a single mosquito bite transmitting malaria) may lead rapidly to intense parasite loads and overwhelming infections; in contrast, for all but the two helminths noted above, increases in worm burden require multiple and usually ongoing exposures to infectious forms, such as ingestion of eggs of intestinal helminths or waterborne exposures to infectious cercariae of Schistosoma mansoni. This requirement is germane both to the consideration of helminthic infections in individuals and to ongoing global efforts to interrupt and/or minimize the acquisition of helminthic infections by humans.
Third, helminthic infections have a predilection toward stimulation of host immune responses that elicit eosinophilia within human tissues and blood. The many protozoan infections characteristically do not elicit eosinophilia in infected humans, with only three exceptions (two intestinal protozoan parasites, Cystoisospora belli and Dientamoeba fragilis, and tissue-borne Sarcocystis species). The magnitude of helminth-elicited eosinophilia tends to correlate with the extent of tissue invasion by larvae or adult helminths. For example, in several helminthic infections, including acute schistosomiasis (Katayama syndrome), paragonimiasis, and hookworm and Ascaris infections, eosinophilia is most pronounced during the early phases of infection, when migrations of infecting larvae and progression of subsequent developmental stages through the tissues are greatest. In established infections, local eosinophilia is often present around helminths in tissues, but blood eosinophilia may be intermittent, mild, or absent. In helminthic infections in which parasites are well contained within tissues (e.g., echinococcal cysts) or confined within the lumen of the intestinal tract (e.g., adult Ascaris or tapeworms), eosinophilia is usually absent.
NEMATODES
Nematodes are nonsegmented roundworms. Species of nematodes are remarkably diverse and abundant in nature. Among the many thousands of nematode species, few are parasites of humans. Most nematodes are free-living, and these species have variably evolved to survive in diverse ecologic niches, including saltwater, freshwater, or soil. The well-studied organism Caenorhabditis elegans is a free-living nematode. Nematodes can be either beneficial or deleterious parasites of plants. Parasitic nematodes have co-evolved with specific mammalian hosts and have no capacity to live their full life cycles in other hosts. Uncommonly, humans are exposed to infectious stages of nonhuman nematode parasites, and the resultant zoonotic nematode infections can elicit inflammatory and immune responses as larval forms migrate and die in the unsuitable human host. Examples include pulmonary coin lesions due to mosquito-transmitted infections with the dog heartworm Dirofilaria immitis; eosinophilic meningoencephalitis due to ingested eggs of the raccoon ascarid Baylisascaris procyonis; and eosinophilic meningitis due to ingestion of larvae of the rat lungworm Angiostrongylus cantonensis.
Nematode parasites of humans include worms that reside in the intestinal tract or localize in extraintestinal vascular or tissue sites. Roundworms are bisexual, with separate male and female forms (except for S. stercoralis, whose adult females are hermaphroditic in the human intestinal tract). Depending on the species, fertilized females release either larvae or eggs containing larvae. Nematodes have five developmental stages: an adult stage and four sequential larval stages. These parasites characteristically are surrounded by a durable outer cuticular layer. Nematodes have a nervous system; a muscular system, including muscle cells under the cuticle; and a developed intestinal tract, including an oral cavity and an elongated gut that ends in an anal pore. Adults may range in size from minute to >1 meter in length (with Dracunculus medinensis, for example, at the long end of this spectrum).
Humans acquire infections with nematode parasites by various routes, depending on the parasitic species. Ingestion of eggs passed in human feces is a major global health problem with many of the intestinal helminths (e.g., Ascaris lumbricoides). In other species, infecting larvae penetrate skin exposed to fecally contaminated soil (e.g., S. stercoralis) or traverse the skin after the bite of infected insect vectors (e.g., filariae). Some nematode infections are acquired by consumption of specific animal-derived foods (e.g., trichinellosis from raw or undercooked pork or wild carnivorous mammals). As noted above, only two nematodes, S. stercoralis and C. philippinensis, can internally reinfect humans.; thus, for all other nematodes, any increases in worm burden must be due to continued exogenous reinfections.
CESTODES
Tapeworms are the cestode parasites of humans. Adult tapeworms are elongated, segmented, hermaphroditic flatworms that reside in the intestinal lumen or, in their larval forms, may live in extraintestinal tissues. Tapeworms include a head (scolex) and a number of attached segments (proglottids). The worms attach to the intestinal tract via their scolices, which may possess suckers, hooks, or grooves. The scolex is the site of formation of new proglottids. Tapeworms do not have a functional gut tract; rather, each tapeworm segment passively and actively obtains nutrients through its specialized surface tegument. Mature proglottids possess both male and female sex organs, but insemination usually occurs between adjacent proglottids. Fertilized proglottids release eggs that are passed in the feces. When ingested by an intermediate host, an egg releases an oncosphere that penetrates the gut and develops further in tissues as a cysticercus. Humans acquire infection by ingesting animal tissues that contain cysticerci, and the resultant tapeworms develop and reside in the proximal small bowel (e.g., Taenia solium, T. saginata). Alternatively, if humans ingest eggs of these cestodes that have been passed in human or animal feces, oncospheres develop and can cause space-occupying extraintestinal cystic lesions in tissues; examples include cysticercosis due to T. solium and hydatid disease due to species of Echinococcus.
TREMATODES
Trematodes of medical importance include blood flukes, intestinal flukes, and tissue flukes. Adult flukes are often leaf-shaped flatworms. Oral and/or ventral suckers help adult flukes maintain their positions in situ. Flukes have an oral cavity but no distal anal pore. Nutrients are obtained both through their integument and by ingestion into the blind intestinal tract. Flukes are hermaphroditic except for blood flukes (schistosomes), which are bisexual. Eggs are passed in human feces (Fasciola, Fasciolopsis, Clonorchis, Schistosoma japonicum, S. mansoni), urine (S. haematobium), or sputum and feces (Paragonimus). Expelled eggs release miracidia—usually in water—that infect specific snail species. Within snails, parasites multiply and cercariae are released. Depending on the species, cercariae can penetrate the skin (schistosomes) or can develop into metacercariae that can be ingested with plants (e.g., watercress for Fasciola) or with fish (Clonorchis) or crabs (Paragonimus).
CONCLUSION
![]() Many of the so-called neglected tropical diseases are due to helminthic infections. The health impacts of many helminthic infections are varied and are based on the frequent need for repeated exposures to increase the worm burdens in infected humans. In global regions where exposures to specific helminths occur even in childhood (e.g., fecally derived intestinal nematodes, mosquito-transmitted filariae, or waterborne snail-transmitted schistosome infections), the morbidities in infected individuals can include nutritional, developmental, cognitive, and functional impairments. Ongoing global mass-treatment programs are currently aimed at diminishing the local prevalences of specific helminths and their consequent impacts on the health of local populations.
Many of the so-called neglected tropical diseases are due to helminthic infections. The health impacts of many helminthic infections are varied and are based on the frequent need for repeated exposures to increase the worm burdens in infected humans. In global regions where exposures to specific helminths occur even in childhood (e.g., fecally derived intestinal nematodes, mosquito-transmitted filariae, or waterborne snail-transmitted schistosome infections), the morbidities in infected individuals can include nutritional, developmental, cognitive, and functional impairments. Ongoing global mass-treatment programs are currently aimed at diminishing the local prevalences of specific helminths and their consequent impacts on the health of local populations.
256 | Trichinellosis and Other Tissue Nematode Infections |
Nematodes are elongated, symmetric roundworms. Parasitic nematodes of medical significance may be broadly classified as either predominantly intestinal or tissue nematodes. This chapter covers the tissue nematodes that cause trichinellosis, visceral and ocular larva migrans, cutaneous larva migrans, cerebral angiostrongyliasis, and gnathostomiasis. All of these zoonotic infections result from incidental exposure to infectious nematodes. The clinical symptoms of these infections are due largely to invasive larval stages that (except in the case of Trichinella) do not reach maturity in humans.
TRICHINELLOSIS
Trichinellosis develops after the ingestion of meat containing cysts of Trichinella (e.g., pork or other meat from a carnivore). Although most infections are mild and asymptomatic, heavy infections can cause severe enteritis, periorbital edema, myositis, and (infrequently) death.
![]() Life Cycle and Epidemiology Eight species of Trichinella are recognized as causes of infection in humans. Two species are distributed worldwide: T. spiralis, which is found in a great variety of carnivorous and omnivorous animals, and T. pseudospiralis, which is found in mammals and birds. T. nativa is present in Arctic regions and infects bears; T. nelsoni is found in equatorial eastern Africa, where it is common among felid predators and scavengers such as hyenas and bush pigs; and T. britovi is found in Europe, western Africa, and western Asia among carnivores but not among domestic swine. T. murrelli is present in North American game animals.
Life Cycle and Epidemiology Eight species of Trichinella are recognized as causes of infection in humans. Two species are distributed worldwide: T. spiralis, which is found in a great variety of carnivorous and omnivorous animals, and T. pseudospiralis, which is found in mammals and birds. T. nativa is present in Arctic regions and infects bears; T. nelsoni is found in equatorial eastern Africa, where it is common among felid predators and scavengers such as hyenas and bush pigs; and T. britovi is found in Europe, western Africa, and western Asia among carnivores but not among domestic swine. T. murrelli is present in North American game animals.
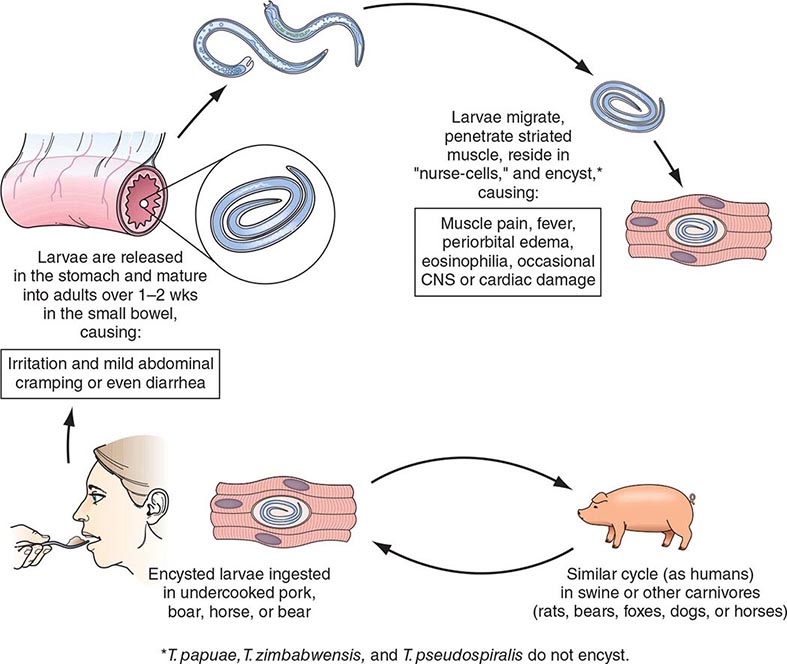
After human consumption of trichinous meat, encysted larvae are liberated by digestive acid and proteases (Fig. 256-1). The larvae invade the small-bowel mucosa and mature into adult worms. After ~1 week, female worms release newborn larvae that migrate via the circulation to striated muscle. The larvae of all species except T. pseudospiralis, T. papuae, and T. zimbabwensis then encyst by inducing a radical transformation in the muscle cell architecture. Although host immune responses may help to expel intestinal adult worms, they have few deleterious effects on muscle-dwelling larvae.
FIGURE 256-1 Life cycle of Trichinella spiralis (cosmopolitan); nelsoni (equatorial Africa); britovi (Europe, western Africa, western Asia); nativa (Arctic); murrelli (North America); papuae (Papua New Guinea); zimbabwensis (Tanzania); and pseudospiralis (cosmopolitan). CNS, central nervous system. (Reprinted from RL Guerrant et al [eds]: Tropical Infectious Diseases: Principles, Pathogens and Practice, 2nd ed, p 1218. © 2006, with permission from Elsevier Science.)
Human trichinellosis is often caused by the ingestion of infected pork products and thus can occur in almost any location where the meat of domestic or wild swine is eaten. Human trichinellosis may also be acquired from the meat of other animals, including dogs (in parts of Asia and Africa), horses (in Italy and France), and bears and walruses (in northern regions). Although cattle (being herbivores) are not natural hosts of Trichinella, beef has been implicated in outbreaks when contaminated or adulterated with trichinous pork. Laws that prohibit the feeding of uncooked garbage to pigs have greatly reduced the transmission of trichinellosis in the United States. About 12 cases of trichinellosis are reported annually in this country, but most mild cases probably remain undiagnosed. Recent U.S. and Canadian outbreaks have been attributable to consumption of wild game (especially bear meat) and, less frequently, of pork.
Pathogenesis and Clinical Features Clinical symptoms of trichinellosis arise from the successive phases of parasite enteric invasion, larval migration, and muscle encystment (Fig. 256-1). Most light infections (those with <10 larvae per gram of muscle) are asymptomatic, whereas heavy infections (which can involve >50 larvae per gram of muscle) can be life-threatening. Invasion of the gut by large numbers of parasites occasionally provokes diarrhea during the first week after infection. Abdominal pain, constipation, nausea, or vomiting also may be prominent.
Symptoms due to larval migration and muscle invasion begin to appear in the second week after infection. The migrating Trichinella larvae provoke a marked local and systemic hypersensitivity reaction, with fever and hypereosinophilia. Periorbital and facial edema is common, as are hemorrhages in the subconjunctivae, retina, and nail beds (“splinter” hemorrhages). A maculopapular rash, headache, cough, dyspnea, or dysphagia sometimes develops. Myocarditis with tachyarrhythmias or heart failure—and, less commonly, encephalitis or pneumonitis—may develop and accounts for most deaths of patients with trichinellosis.
Upon onset of larval encystment in muscle 2–3 weeks after infection, symptoms of myositis with myalgias, muscle edema, and weakness develop, usually overlapping with the inflammatory reactions to migrating larvae. The most commonly involved muscle groups include the extraocular muscles; the biceps; and the muscles of the jaw, neck, lower back, and diaphragm. Peaking ~3 weeks after infection, symptoms subside only gradually during a prolonged convalescence. Uncommon infections with T. pseudospiralis, whose larvae do not encapsulate in muscles, elicit prolonged polymyositis-like illness.
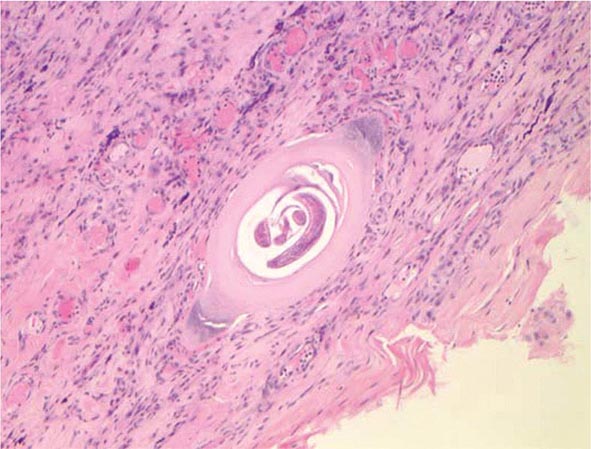
Laboratory Findings and Diagnosis Blood eosinophilia develops in >90% of patients with symptomatic trichinellosis and may peak at a level of >50% 2–4 weeks after infection. Serum levels of muscle enzymes, including creatine phosphokinase, are elevated in most symptomatic patients. Patients should be questioned thoroughly about their consumption of pork or wild animal meat and about illness in other individuals who ate the same meat. A presumptive clinical diagnosis can be based on fevers, eosinophilia, periorbital edema, and myalgias after a suspect meal. A rise in the titer of parasite-specific antibody, which usually does not occur until after the third week of infection, confirms the diagnosis. Alternatively, a definitive diagnosis requires surgical biopsy of at least 1 g of involved muscle; the yields are highest near tendon insertions. The fresh muscle tissue should be compressed between glass slides and examined microscopically (Fig. 256-2), because larvae may be missed by examination of routine histopathologic sections alone.
FIGURE 256-2 Trichinella larva encysted in a characteristic hyalinized capsule in striated muscle tissue. (Photo/Wadsworth Center, New York State Department of Health. Reprinted from MMWR 53:606, 2004; public domain.)
THERAPY FOR TISSUE NEMATODE INFECTIONS |
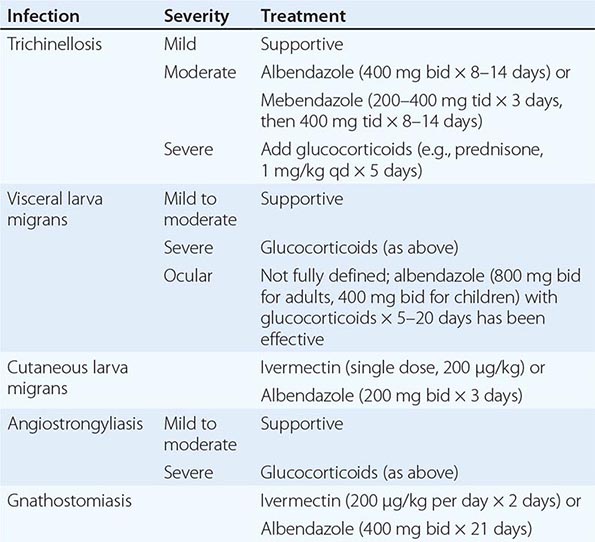
Prevention Larvae may be killed by cooking pork until it is no longer pink or by freezing it at –15°C for 3 weeks. However, Arctic T. nativa larvae in walrus or bear meat are relatively resistant and may remain viable despite freezing.
VISCERAL AND OCULAR LARVA MIGRANS
Visceral larva migrans is a syndrome caused by nematodes that are normally parasitic for nonhuman host species. In humans, these nematode larvae do not develop into adult worms but instead migrate through host tissues and elicit eosinophilic inflammation. The most common form of visceral larva migrans is toxocariasis due to larvae of the canine ascarid Toxocara canis; the syndrome is due less commonly to the feline ascarid T. cati and even less commonly to the pig ascarid Ascaris suum. Rare cases with eosinophilic meningoencephalitis have been caused by the raccoon ascarid Baylisascaris procyonis.
![]() Life Cycle and Epidemiology The canine roundworm T. canis is distributed among dogs worldwide. Ingestion of infective eggs by dogs is followed by liberation of Toxocara larvae, which penetrate the gut wall and migrate intravascularly into canine tissues, where most remain in a developmentally arrested state. During pregnancy, some larvae resume migration in bitches and infect puppies prenatally (through transplacental transmission) or after birth (through suckling). Thus, in lactating bitches and puppies, larvae return to the intestinal tract and develop into adult worms, which produce eggs that are released in the feces. Eggs must undergo embryonation over several weeks to become infectious. Humans acquire toxocariasis mainly by eating soil contaminated by puppy feces that contains infective T. canis eggs. Visceral larva migrans is most common among children who habitually eat dirt.
Life Cycle and Epidemiology The canine roundworm T. canis is distributed among dogs worldwide. Ingestion of infective eggs by dogs is followed by liberation of Toxocara larvae, which penetrate the gut wall and migrate intravascularly into canine tissues, where most remain in a developmentally arrested state. During pregnancy, some larvae resume migration in bitches and infect puppies prenatally (through transplacental transmission) or after birth (through suckling). Thus, in lactating bitches and puppies, larvae return to the intestinal tract and develop into adult worms, which produce eggs that are released in the feces. Eggs must undergo embryonation over several weeks to become infectious. Humans acquire toxocariasis mainly by eating soil contaminated by puppy feces that contains infective T. canis eggs. Visceral larva migrans is most common among children who habitually eat dirt.
Pathogenesis and Clinical Features Clinical disease most commonly afflicts preschool children. After humans ingest Toxocara eggs, the larvae hatch and penetrate the intestinal mucosa, from which they are carried by the circulation to a wide variety of organs and tissues. The larvae invade the liver, lungs, central nervous system (CNS), and other sites, provoking intense local eosinophilic granulomatous responses. The degree of clinical illness depends on larval number and tissue distribution, reinfection, and host immune responses. Most light infections are asymptomatic and may be manifest only by blood eosinophilia. Characteristic symptoms of visceral larva migrans include fever, malaise, anorexia and weight loss, cough, wheezing, and rashes. Hepatosplenomegaly is common. These features may be accompanied by extraordinary peripheral eosinophilia, which may approach 90%. Uncommonly, seizures or behavioral disorders develop. Rare deaths are due to severe neurologic, pneumonic, or myocardial involvement.
The ocular form of the larva migrans syndrome occurs when Toxocara larvae invade the eye. An eosinophilic granulomatous mass, most commonly in the posterior pole of the retina, develops around the entrapped larva. The retinal lesion can mimic retinoblastoma in appearance, and mistaken diagnosis of the latter condition can lead to unnecessary enucleation. The spectrum of eye involvement also includes endophthalmitis, uveitis, and chorioretinitis. Unilateral visual disturbances, strabismus, and eye pain are the most common presenting symptoms. In contrast to visceral larva migrans, ocular toxocariasis usually develops in older children or young adults with no history of pica; these patients seldom have eosinophilia or visceral manifestations.
Diagnosis In addition to eosinophilia, leukocytosis and hypergammaglobulinemia may be evident. Transient pulmonary infiltrates are apparent on chest x-rays of about one-half of patients with symptoms of pneumonitis. The clinical diagnosis can be confirmed by an enzyme-linked immunosorbent assay for toxocaral antibodies. Stool examination for parasite eggs is worthless in toxocariasis, since the larvae do not develop into egg-producing adults in humans.
CUTANEOUS LARVA MIGRANS
Cutaneous larva migrans (“creeping eruption”) is a serpiginous skin eruption caused by burrowing larvae of animal hookworms, usually the dog and cat hookworm Ancylostoma braziliense. The larvae hatch from eggs passed in dog and cat feces and mature in the soil. Humans become infected after skin contact with soil in areas frequented by dogs and cats, such as areas underneath house porches. Cutaneous larva migrans is prevalent among children and travelers in regions with warm humid climates, including the southeastern United States.
After larvae penetrate the skin, erythematous lesions form along the tortuous tracks of their migration through the dermal-epidermal junction; the larvae advance several centimeters in a day. The intensely pruritic lesions may occur anywhere on the body and can be numerous if the patient has lain on the ground. Vesicles and bullae may form later. The animal hookworm larvae do not mature in humans and, without treatment, will die after an interval ranging from weeks to a couple of months, with resolution of skin lesions. The diagnosis is made on clinical grounds. Skin biopsies only rarely detect diagnostic larvae. Symptoms can be alleviated by ivermectin or albendazole (Table 256-1).
ANGIOSTRONGYLIASIS
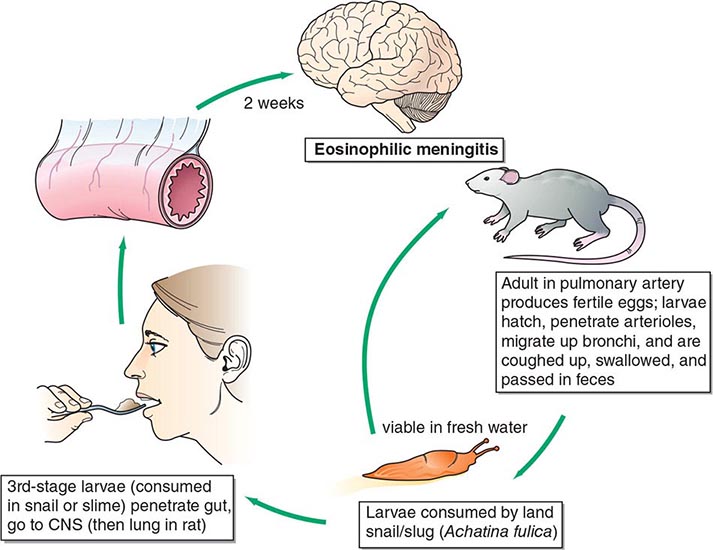
Angiostrongylus cantonensis, the rat lungworm, is the most common cause of human eosinophilic meningitis (Fig. 256-3).
FIGURE 256-3 Life cycle of Angiostrongylus cantonensis (rat lung worm), found in Southeast Asia, Pacific Islands, Cuba, Australia, Japan, China, Mauritius, and U.S. ports. CNS, central nervous system. (Reprinted from RL Guerrant et al [eds]: Tropical Infectious Diseases: Principles, Pathogens and Practice, 2nd ed, p 1225. © 2006, with permission from Elsevier Science.)
![]() Life Cycle and Epidemiology This infection occurs principally in Southeast Asia and the Pacific Basin but has spread to other areas of the world, including the Caribbean islands, countries in Central and South America, and the southern United States. A. cantonensis larvae produced by adult worms in the rat lung migrate to the gastrointestinal tract and are expelled with the feces. They develop into infective larvae in land snails and slugs. Humans acquire the infection by ingesting raw infected mollusks; vegetables contaminated by mollusk slime; or crabs, freshwater shrimp, and certain marine fish that have themselves eaten infected mollusks. The larvae then migrate to the brain.
Life Cycle and Epidemiology This infection occurs principally in Southeast Asia and the Pacific Basin but has spread to other areas of the world, including the Caribbean islands, countries in Central and South America, and the southern United States. A. cantonensis larvae produced by adult worms in the rat lung migrate to the gastrointestinal tract and are expelled with the feces. They develop into infective larvae in land snails and slugs. Humans acquire the infection by ingesting raw infected mollusks; vegetables contaminated by mollusk slime; or crabs, freshwater shrimp, and certain marine fish that have themselves eaten infected mollusks. The larvae then migrate to the brain.
Pathogenesis and Clinical Features The parasites eventually die in the CNS, but not before initiating pathologic consequences that, in heavy infections, can result in permanent neurologic sequelae or death. Migrating larvae cause marked local eosinophilic inflammation and hemorrhage, with subsequent necrosis and granuloma formation around dying worms. Clinical symptoms develop 2–35 days after the ingestion of larvae. Patients usually present with an insidious or abrupt excruciating frontal, occipital, or bitemporal headache. Neck stiffness, nausea and vomiting, and paresthesias are also common. Fever, cranial and extraocular nerve palsies, seizures, paralysis, and lethargy are uncommon.
Laboratory Findings Examination of cerebrospinal fluid (CSF) is mandatory in suspected cases and usually reveals an elevated opening pressure, a white blood cell count of 150–2000/μL, and an eosinophilic pleocytosis of >20%. The protein concentration is usually elevated and the glucose level normal. The larvae of A. cantonensis are only rarely seen in CSF. Peripheral-blood eosinophilia may be mild. The diagnosis is generally based on the clinical presentation of eosinophilic meningitis together with a compatible epidemiologic history.