Traumatic Injury to the Diaphragm
H. Leon Pachter
Spiros G. Frangos
Ronald J. Simon
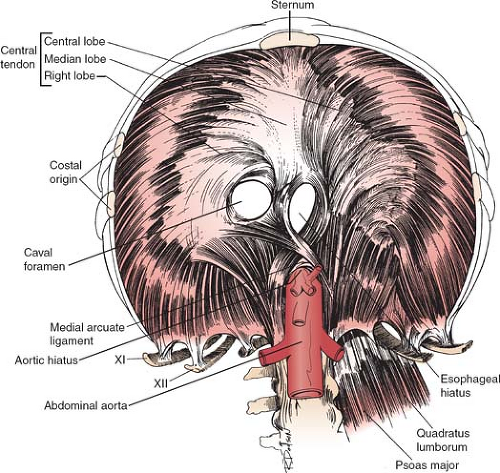
The primary muscle responsible for breathing is the diaphragm, a musculoaponeurotic barrier that separates the thoracic and the abdominal cavities. Muscle fibers originate higher anteriorly from the sternum’s xiphoid process. Their origins laterally and posteriorly are more inferior; they arise from the costal cartilages and osseous portions of the lower ribs and the lumbar vertebral bodies and their intervertebral discs (Fig. 1). These fibers all insert into the diaphragm’s aponeurotic portion known as the central tendon. The right dome is naturally 2 cm higher than the left owing to the mass effect of the underlying liver.
Three major orifices—the caval, esophageal, and aortic—allow for the passage of major structures (Fig. 1). The aponeurotic caval opening, which is found at the T-8 level, allows the inferior vena cava and often the right phrenic nerve to traverse body cavities. The diaphragm’s lumbar origin includes left and right crural fibers, which form the boundaries of the esophageal and aortic hiatus. The esophagus and the vagus nerves traverse the esophageal hiatus—a gap between the right crural fibers—at the T-10 level. The aortic hiatus, which is formed by the fibers of the left and the right crura, is located at the T-12 level and allows for passage of the aorta, thoracic duct, and variably the azygos and the hemiazygos veins.
The diaphragm’s blood supply comes from inferior and superior phrenic arteries arising directly from the thoracoabdominal aorta. Superior epigastric and intercostal arteries provide blood to the muscle’s costal margins. Venous drainage is through phrenic veins directly into the inferior vena cava. The motor nerve supply of the diaphragm is through left and right phrenic nerves. The left phrenic nerve passes through the muscular diaphragm more anteriorly than the right phrenic nerve, which passes through the aponeurotic central tendon through or in close proximity to the caval opening. The two main trunks typically divide into three main branches: anterior, anterolateral, and posterior.
An understanding of diaphragmatic anatomy by surgeons who care for trauma patients is important to avoid missed injuries. Additionally, the variable topography of the muscle—especially when assessing for trajectory in penetrating trauma—must be recognized. A patient’s positioning (e.g., supine vs. erect) and phase and depth of ventilation affect the location of the left and right diaphragmatic domes, which can vary by as much as 10 cm. Each individual’s natural build and pulmonary pathophysiology (e.g., chronic obstructive pulmonary disease) also play a role in the muscle’s topography. Furthermore, a firm grasp of diaphragmatic anatomy is important in minimizing iatrogenic phrenic nerve injury during operative repair.
Left hemidiaphragm injuries may be more common than right as a result of the anatomic (in penetrating trauma) and force-distribution (in blunt trauma) protection afforded by the extensive solid parenchymal mass of the liver. There exists some controversy into whether this is truly the case or whether we are simply being
fooled by the injured left hemidiaphragm’s clinical predominance. Untreated right-sided injuries are less likely to produce untoward sequelae as a result of the barrier protection that the liver provides. Bilateral dome injury is uncommon regardless of mechanism as is herniation into the mediastinum. The American Association for the Surgery of Trauma (AAST) organ injury scale for the diaphragm is depicted in Table 1.
fooled by the injured left hemidiaphragm’s clinical predominance. Untreated right-sided injuries are less likely to produce untoward sequelae as a result of the barrier protection that the liver provides. Bilateral dome injury is uncommon regardless of mechanism as is herniation into the mediastinum. The American Association for the Surgery of Trauma (AAST) organ injury scale for the diaphragm is depicted in Table 1.
Table 1 AAST Organ Injury Scale—Diaphragma | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
The diaphragm is uncommonly injured in an isolated fashion. Diaphragmatic injury resulting from blunt trauma usually accompanies injury to local structures including ribs and abdominal solid viscera, especially the liver and the spleen. Pelvic and long-bone fractures and traumatic brain injury are frequently seen in these patients, an association, which is not surprising given the significant force required to rupture a hemidiaphragm. Penetrating injury to the diaphragm is also usually accompanied by injuries to one or more nearby viscera, including the lungs, the liver, the stomach, the spleen, the kidneys, and the colon. Bullets lead to a greater number of local visceral injuries than do knives. A high index of suspicion for a diaphragmatic injury remains the key with penetrating thoracoabdominal or high velocity deceleration mechanisms.
Penetrating Trauma
When evaluating for the possibility of a diaphragmatic injury, the location of the wound is important and can be readily inspected in the emergency room. Nonetheless, it is the trajectory of the foreign body relative to the diaphragm that is even more important. Unfortunately, this is much more difficult to ascertain by history and physical examination. Penetrating injuries between the nipples and the lower costal margin place the diaphragm at risk for injury. Anterior and lateral thoracoabdominal penetrating injuries are more likely to lacerate the diaphragm than are those to the back along the same axial plane. Traumatic injuries to the diaphragm as a result of penetrating trauma are usually small (1 to 3 cm) lacerations and are not associated with acute herniation. These patients rarely have any symptoms associated to the diaphragmatic injury alone.
The incidence of diaphragmatic injury as a result of penetrating thoracoabdominal trauma is not well delineated in existing studies because of variability in the denominator data (i.e., the study population). Additionally, inclusion and exclusion criteria, including anatomical boundaries and indications for operative exploration, are inconsistent between the studies.
Although penetrating injury to the diaphragm is more common than blunt, the natural history of these smaller diaphragmatic injuries is unclear. This leaves clinicians with two vital questions: what is the incidence of occult injury (rather than any injury, which would have been diagnosed and treated regardless) and what percentage of these untreated patients go on to sustain complications (i.e., herniation) from these lesions if left untreated. Without these answers, the optimal treatment of known or suspected injuries is left to one’s own experience and judgment.
Blunt Trauma
When considering blunt diaphragmatic injury, a thorough assessment of the severity of the event must be made as the potential for an injury is entirely related to mechanism. This injury occurs as a result of significant deceleration mechanism or truncal impact, contributing to a rapid and abrupt increase in intra-abdominal pressure. For a victim of a motor vehicle collision, the approximate velocity of the incident must be considered because high delta-V (i.e., significant change in velocity) decelerations are more likely to lead to rupture of a hemidiaphragm. Occupant compartment intrusion and seat belt use also play a vital role. For a victim of a fall, it is important to ascertain the height and the surface of impact so as to extrapolate for the deceleration forces.
Traumatic injuries to the diaphragm as a result of blunt trauma are larger than penetrating lacerations (usually longer than 5 cm) and are commonly associated with acute herniation. These patients may have symptoms associated to the diaphragmatic injury, including shortness of breath or respiratory distress especially in those larger defects with herniation. However, with the plethora of associated injuries, which commonly require immediate treatment in these often critically ill patients, there is a high likelihood of a delay in diagnosis or a missed injury of the diaphragm. Because pulmonary symptoms associated with a blunt force diaphragmatic injury are nonspecific, a high index of suspicion is mandatory.
Chronic Diaphragmatic Hernia
Patients with missed or untreated diaphragmatic injuries often present in a delayed fashion with symptoms related to intestinal herniation or strangulation. Over time, small diaphragmatic holes may increase in size given the constant activity of the muscle, and the pressure gradient between the pleural and the peritoneal cavities pulls intraperitoneal organs into the chest. Presentations run the gamut from nausea and vomiting from bowel obstruction, to pain from volvulus or incarceration, to septic shock from strangulated dead gut. Undoubtedly, the sequelae of a missed diaphragm injury can be devastating.
The diagnosis of a diaphragmatic injury in a patient who does not otherwise warrant immediate thoracic or abdominal surgical intervention can be challenging. Generally, the ability to make an accurate diagnosis outside an operating room (OR) relates to the size of the defect.
Physical Examination
The physical exam is unreliable for diagnosing diaphragmatic injury following blunt or penetrating trauma. There are no truly sensitive signs to detect an underlying injury. Following penetrating injuries, the trajectory of the knife or bullet is more important than the actual location of the skin wound, but it is usually difficult to elicit accurately. Probing a thoracoabdominal wound, especially one overlying the ribcage, is generally discouraged for fear of creating or exacerbating a pneumothorax. The insertion of a cotton applicator superficially by an experienced surgeon may however provide some indication of trajectory, and there are circumstances—obese patients, wounds to the back, or with apparent tangential trajectories—where this maneuver, when applied cautiously, may be useful for ruling out an underlying injury.
The physical exam lacks sensitive or specific signs of a diaphragm injury following blunt trauma as well. However, there are certain signs, which are suggestive of injury, including unilateral decreased breath sounds, bowel sounds in the chest, and respiratory distress. The multiple associated injuries usually found in patients with ruptured diaphragms often delay the diagnosis from being made in the emergency department.
Imaging
A chest radiograph is commonly performed but rarely diagnostic. This is especially true for penetrating trauma where diaphragm injuries are smaller and plain films are seldom helpful. A chest X-ray more commonly will make the diagnosis following a blunt mechanism and in these circumstances may appear dramatic. Examples of such radiographic evidence include air or an air–fluid level within a hollow viscus overlying the thorax or with the additional “classic” finding of the coiling supradiaphragmatic nasogastric tube. Suggestive findings include abnormality in the contour, shape, or elevation of the hemidiaphragm, pleural effusion or atelectasis, and mediastinal shift to the side contralateral to the injury. The chances of seeing these signs are even further reduced in patients on positive pressure ventilation, as the contour of the lower lobes of the lungs, when expanded under pressure, mimics that of the intact diaphragm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree