Tracheotomy
Paul F. Castellanos
Introduction
The surgical access to the airway has three spheres, each with different distinct anatomical considerations and clinical indications. These are the open surgical tracheotomy, the emergency tracheotomy or cricothyrotomy, and the percutaneous dilatational tracheotomy (PDT). The first two have a wide range of described techniques each with advocates and detractors. The indications for a surgical open tracheotomy include: the securing of the airway for its prolonged intubation and mechanical ventilation; the bypass of the upper airway for ventilatory protection, perhaps in preparation for major head and neck surgery; and the establishment of the airway below a narrowing to enable safe respiration after the structures above this point have become scarred, most often after prolonged orotracheal intubation.
Emergency airway access techniques include cricothyrotomy and “slash” tracheotomy, each done as quickly as possible in the context of an arrest with the single-minded indication being the preserving of the patient’s life. While the surgical anatomy is relevant in the general sense, it is far less of an issue than getting a tube into the airway by whatever means as quickly as humanly possible. This, therefore, involves relegating the process of airway protection and reducing the risk of complications to the surgical aftermath of the successful emergency procedure.
PDT is a relatively new sphere of airway surgery generally performed at the bedside within the intensive care unit (ICU) with minimal surgical instrumentation and simple surface anatomy guidance. The process includes, in most circumstances, some means to see into the airway such as a flexible or rigid video endoscope to establish where you are entering the airway from within. It is indicated for the critically ill ventilated patient who would otherwise have to be taken, ventilator and all, to the operating room (OR). Concerns about the potential for great and dire complications have made this sphere slow to evolve and fraught with controversy.
General Issues and Indications
The primary indication for tracheotomy is the bypassing of the larynx when prolonged intubation is necessary to reduce the risk of airway stenosis and secure airway access. Apart from these, other indications include the treatment of airway obstruction and the protection of the airway in anticipation of head and neck surgery. The timing of when to consider this operation in the context of prolonged intubation is both critical and controversial. There are data that support a 10- to 12-day window
of intubation as the target for converting from orotracheal intubation to tracheotomy access. Having performed many bedside laryngoscopy procedures in the context of tracheotomy, I have found a huge variability in the degree of laryngotracheal injury associated with prolonged intubation. I have developed a strategy for anticipating the need for conversion to tracheotomy.
of intubation as the target for converting from orotracheal intubation to tracheotomy access. Having performed many bedside laryngoscopy procedures in the context of tracheotomy, I have found a huge variability in the degree of laryngotracheal injury associated with prolonged intubation. I have developed a strategy for anticipating the need for conversion to tracheotomy.
Younger patients are commonly able to tolerate longer intubations. This does not apply to children whose airway care is out of the scope of this work. The closed head injury patients, who tend to be younger, are an exception to this generalization because they tend to be constantly fighting to get the ETT out of their throats, bucking and coughing. The pure physical erosion of this process is very damaging to the larynx and the constant “combat” is intrinsically dangerous. They either need to be converted to a tracheotomy or extubated in a controlled way as soon as prudent. This may be within the first 2 to 3 days of their care. Conversely, the comatose patient who needs no sedation and who has some chance of spontaneous recovery will often have a pristine larynx even after 2 or 3 weeks of OT intubation. They do not cough. They do not swallow. They just lay there. The other consideration is to get them out of a unit by converting them over to a tracheotomy. This is a care and logistics issue not related to avoiding injury to the larynx.
On the other end of the spectrum is the patient with known or suspected extra-esophageal reflux. Even a couple of days of intubation in these patients can result in profound ulcerative laryngitis and edema. These patients commonly fail extubation for unclear reasons after having been weaned off the ventilator, but still get a tracheotomy because additional efforts at extubation also fail. They are a group of patients I refer to as having an “at risk” airway. Apart from their reflux-related throat disease, other factors that can alone or in concert produce this increased risk of airway edema and vulnerability are: immunosuppression; microvascular disease; diabetes mellitus; and history of recent airway instrumentation. In the context of these additional risks, my recommendation is to proceed with an early tracheotomy to protect the larynx. The trachea is also at risk from all of these factors. See below in the complications section to address this issue.
The surgically matured tracheostomy is indicated in a couple of clinical scenarios. The first is in a patient whose neurologic condition is so poor or so inexorable that there is essentially no chance they will ever be decannulated. Examples of such conditions include huge strokes, extensive brain injury, or high quadriplegia. The second scenario is in the care of patients with intractable aspiration who are being treated by one of a variety of laryngeal closure or diversion techniques and need a permanent stoma to avoid airway obstruction if the cannula ever fell out or became plugged and had to be removed. In both cases, this technique allows a low maintenance stoma and the safety of a channel that will remain open for hours to days with no cannula at all in many cases. The down side is that if the clinical assessment is incorrect and the person’s condition does improve, the stoma will have to be closed by a somewhat extensive operation.
Open Tracheostomy Techniques
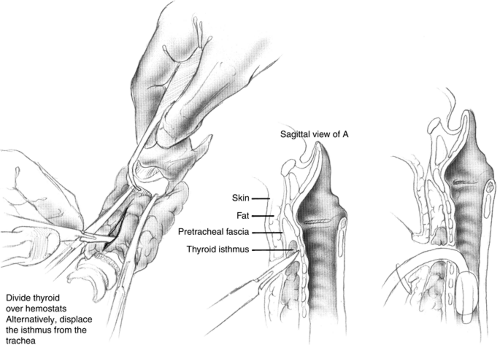
There are innumerable techniques for performing a tracheotomy and a tracheostomy (Fig. 1). The distinction between the two is of a surgically mature stoma in the latter, though both involve an opening or “otomy” into the trachea as an intrinsic feature of the operation. Vertical or transverse skin incisions are often debated. The vertical is more easily made with little risk of needing to ligate large anterior jugular veins but heals less well than a transverse incision that can be put into a skin crease. The deep dissection often includes the need to either divide or reposition the thyroid isthmus. Dividing it gives a broad access to the trachea but makes a much bigger wound with a larger amount of devitalized tissue within it in the form of cauterized or suture-ligated thyroid. Therefore, this wound is more apt to drain and become fetid. Conversely, the potential for inadvertent decannulation is lower and the ease of replacing the cannula is far greater in the wound with the additional dissection. I personally favor leaving the thyroid isthmus intact to reduce the wound problems and to support the cartilage in the vicinity of the tracheotomy by the extensive blood supply that the thyroid provides to the trachea. I suture the cannula base to the neck to secure it against inadvertent removal until the track has “formed.”
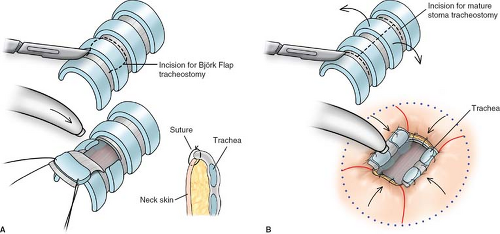
The type of tracheal incision is also an area of great controversy. My recommendation is to avoid disrupting the circular integrity of the trachea as much as you can. Keeping the axial blood supply is very beneficial to eventual safe decannulation without significant stenosis (see section on complications). A generous transverse incision is preferable to an inferiorly based (and therefore random) cartilage flap known as a “Bjork flap” to protect the trachea and reduce the stenosis risk (Fig. 2). Leaving one or two undisturbed rings below the cricoid is also beneficial to increase the protection to the cricoid.
Erosion up toward the larynx is common, particularly in obese patients or those with very short necks. These body types promote the development of stenosis by the upward displacement of the cannula and the consequent disrupting of the anterior tracheal wall. The classic surface appearance is of a tracheostomy wound with a dense vertical scar beneath it indicating that the initial entry point into the airway was far lower than it ended up (Fig. 3). A higher cannula placement point can therefore be justified in these patients to help avoid this. Moving quickly to decannulation is more important in this population. They can be considered to be at a very high risk of post tracheotomy complications.
The technique I advocate for a “mature stoma” tracheostomy involves the generation of laterally based cartilage flaps sewn to the skin by multiple buried absorbable sutures (I use 4-0 PDS on a taper needle like an RB-1) (Fig. 4). I use a vertical incision through two rings in the midline connected above and below by a generous transverse incision. This is termed an “I” flap by virtue of the shape of the capital letter “I.” The cartilage of each flap is supported by lateral axial blood and mucosa, so there is no “random” feature to the support of this tissue that may promote iatrogenic stenosis. All the suture materials I use in this technique are absorbable so as to avoid the need for suture removal from a difficult to access area. I also place all of my sutures while the patient is still intubated from above through the larynx so that there is no encumbrance from the respiratory circuit coming through the skin while trying to sew the cartilage flaps down (Fig. 5; see also Figs. 2 and 4).
Complications of Tracheotomy
I have found no technique that enables one to avoid all of the common complication of this procedure. These are: inadvertent decannulation, or the loss of the airway from the separation of the trachea from the airway appliance; local infection; stenosis or cicatricial scarring above, within, or below the airway entry point; cartilaginous or membranous tracheomalacia; and the potential of injury to the critical neighboring structures such as the esophagus posteriorly and the innominate artery anteriorly. Internal disruption of tissue is the cause of most of these complications and is sometimes contributed to by the gradual increase in cuff volume used to maintain minute ventilation. This de facto airway dilator
of the infrastomal airway will eventually erode the mucosa and scar the distal trachea. This is a very difficult clinical problem to repair. Erosion into the anterior or posterior wall may also occur, thus entering the adjacent structures. Although, in my experience, erosion of this type is more likely the result of the contour and direction of the airway relative to the cannula design, the angle of the tip of the cannula, the cannula’s flexibility, and the surface of the patient’s neck and chest. Depending on these factors, the tip of the tube may be pointing into the “party wall” with the esophagus or the anterior trachea toward the largest artery of the body apart from the aorta (Fig. 6). The dilation that occurs, even in the absence of erosion, can be its own disease in the form of tracheomalacia. This can make the process of decannulation laborious, long, and potentially unsuccessful. Other factors such as the patient’s overall state of nutrition, the ventilatory pressures being used, and patient movements like repeated swallowing and coughing play a role in this erosive and dilatational process. Because of these host factors, potentially dire complications can occur even under the most meticulous attention. As a caretaker of these complications, I have a list of recommendation to help avoid them: (a) cuff pressure monitoring multiple times per day and (b) keeping track of the total volume in a cuff. Changes in cuff pressure and volume will indicate a gradual dilation of the trachea and may herald the damage that leads to complications. (c) Endoscopic evaluation of the airway through the tracheotomy tube can guide appliance choice and its adjustment to avoid the piercing of the walls in any direction. If done with a “side port” attachment, the circuit for ventilation is maintained and the distention of the airway as it is during normal mechanical ventilation can make this assessment more accurate.
of the infrastomal airway will eventually erode the mucosa and scar the distal trachea. This is a very difficult clinical problem to repair. Erosion into the anterior or posterior wall may also occur, thus entering the adjacent structures. Although, in my experience, erosion of this type is more likely the result of the contour and direction of the airway relative to the cannula design, the angle of the tip of the cannula, the cannula’s flexibility, and the surface of the patient’s neck and chest. Depending on these factors, the tip of the tube may be pointing into the “party wall” with the esophagus or the anterior trachea toward the largest artery of the body apart from the aorta (Fig. 6). The dilation that occurs, even in the absence of erosion, can be its own disease in the form of tracheomalacia. This can make the process of decannulation laborious, long, and potentially unsuccessful. Other factors such as the patient’s overall state of nutrition, the ventilatory pressures being used, and patient movements like repeated swallowing and coughing play a role in this erosive and dilatational process. Because of these host factors, potentially dire complications can occur even under the most meticulous attention. As a caretaker of these complications, I have a list of recommendation to help avoid them: (a) cuff pressure monitoring multiple times per day and (b) keeping track of the total volume in a cuff. Changes in cuff pressure and volume will indicate a gradual dilation of the trachea and may herald the damage that leads to complications. (c) Endoscopic evaluation of the airway through the tracheotomy tube can guide appliance choice and its adjustment to avoid the piercing of the walls in any direction. If done with a “side port” attachment, the circuit for ventilation is maintained and the distention of the airway as it is during normal mechanical ventilation can make this assessment more accurate.
Inadvertent decannulation warrants special mention. It is possibly the most common complication of tracheotomy and tends to occur early after the procedure has been performed and before scar has formed to maintain the trachea in registration with the skin incision. This enables the tip of the cannula to fall out entirely or to sit within a false passage anterior to the tracheal lumen. The patient may be able to breath, in the latter situation, through the cannula for a short time but usually the loss of tidal volumes and decreased gas exchange begin to indicate a problem. If the driving pressures are increased or “bag ventilation” is employed enabling far higher air pressure and volume delivery, a pneumothorax soon follows and a dire downward spiral can result. The cannula can sometimes be replaced by “feel,” if the problem is caught early and the tracheal wall is still widely open. If not, manipulating the cannula can fully close off the communication between the skin and the trachea. Intubation from above should be considered under such circumstances. If intubation
from above is not successful or the patient has arrested, removal of the existing cannula and digital exploration of the wound should be attempted. The anterior tracheal wall may be palpated and the opening into the trachea found. If so, an ETT can be used to reintubate the airway and provide for some degree of ventilation while chest tubes are being placed. The tracheotomy cannula can be passed by Seldinger technique once the situation is stabilized. Depending on why the cannula became dislodged in the first place, it may be reasonable to introduce an extra long cannula such as the Shiley XLT that comes with a proximal or distal extra long segment (Mallinckrodt, St. Louis, MO).
from above is not successful or the patient has arrested, removal of the existing cannula and digital exploration of the wound should be attempted. The anterior tracheal wall may be palpated and the opening into the trachea found. If so, an ETT can be used to reintubate the airway and provide for some degree of ventilation while chest tubes are being placed. The tracheotomy cannula can be passed by Seldinger technique once the situation is stabilized. Depending on why the cannula became dislodged in the first place, it may be reasonable to introduce an extra long cannula such as the Shiley XLT that comes with a proximal or distal extra long segment (Mallinckrodt, St. Louis, MO).
 Fig. 3. A: This stoma began at the level of the transverse scar and eroded upward. The jagged edges are made up of granulation tissue and cartilage that has lost it circular shape. B: This very old tracheostomy lacks obvious granulation tissue but clearly has eroded up from its original starting point near the thoracic inlet up to its ending spot below the larynx. Both patients experienced severe airway complications from the tracheotomies. “A” required a segmental tracheal resection prior to being able to be decannulated. “B” was able to be decannulated after a series of minimally invasive procedures to widen his airway from the inside.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|