Patient Story
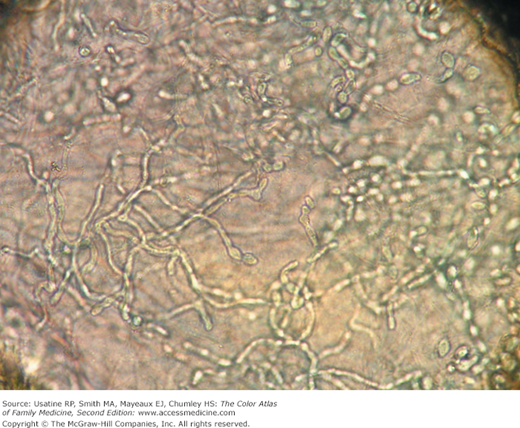
A 59-year-old man presents with itching in the groin (Figure 139-1). On examination, he was found to have scaly erythematous plaques in the inguinal area. A skin scraping was treated with Swartz-Lamkins stain and the dermatophyte was highly visible under the microscope (Figure 139-2). He was treated with a topical antifungal medicine until his tinea cruris resolved.
Introduction
Epidemiology
- Using data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey (NHAMCS) (1995-2004), there were more than 4 million annual visits for dermatophytoses and 8.4% were for tinea cruris.1
- Tinea cruris is more common in men than women (three-fold) and rare in children.
Etiology and Pathophysiology
- Most commonly caused by the dermatophytes: Trichophyton rubrum, Epidermophyton floccosum, Trichophyton mentagrophytes, and Trichophyton verrucosum. T. rubrum is the most common organism.2
- Can be spread by fomites, such as contaminated towels.
- The fungal agents cause keratinases, which allow invasion of the cornified cell layer of the epidermis.2
- Autoinoculation can occur from fungus on the feet or hands.
Risk Factors
- Wearing tight-fitting or wet clothing or underwear has traditionally been suggested; however, in a study of Italian soldiers, none of the risk factors analyzed (e.g., hyperhidrosis, swimming pool attendance) were significantly associated with any fungal infection.3
- Obesity and diabetes mellitus may be risk factors.4
Diagnosis
The cardinal features are scale and signs of inflammation. In light-skinned persons inflammation often appears pink or red and in dark-skinned persons the inflammation often leads to hyperpigmentation (Figures 139-3 and 139-4). Occasionally, tinea cruris may show central sparing with an annular pattern as in Figure 139-5, but most often is homogeneously distributed as in Figures 139-3 and 139-4.
Figure 139-3
Tinea cruris in an older black man with hyperpigmentation secondary to the inflammatory response. A silvery scale is also seen and psoriasis should be considered in the differential diagnosis. In such a case, performing a potassium hydroxide preparation is crucial to making an accurate diagnosis as it is not possible to know the diagnosis by appearance only. (Courtesy of Richard P. Usatine, MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree