Patient Story
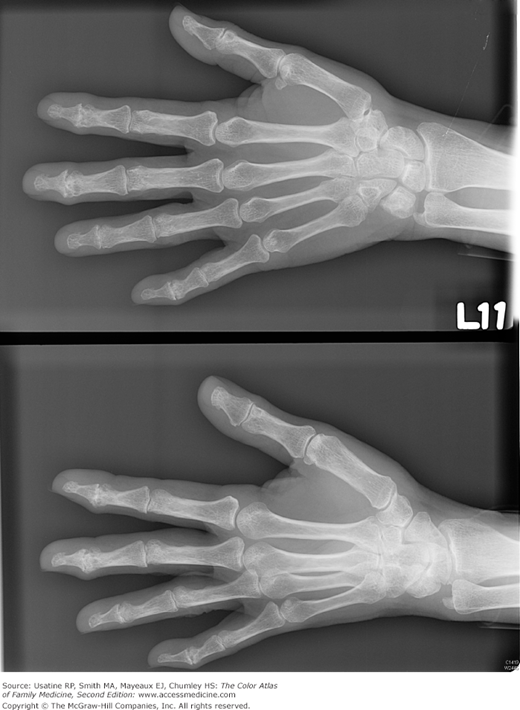
A 70-year-old woman presents with pain and swelling in the joints of both hands, which impedes her normal activities. Her pain is better in the morning after resting and worse after she has been working with her hands. She denies stiffness. On examination, you find bony enlargement of some distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints on both hands (Figure 96-1). Radiographs confirm the presence of Heberden and Bouchard nodes. She begins taking 1 g of acetaminophen twice a day and has significant improvement in her pain and function.
Introduction
Epidemiology
- Osteoarthritis is the most common type of arthritis, affecting 10% of men and 13% of women age 60 years or older.1,2
- Incidence and prevalence will likely increase given the obesity epidemic and the aging of the population.2
- In the Framingham cohort (mean age 71 years at baseline) women and men developed symptomatic knee osteoarthritis at the rate of 1% and 0.7% per year, respectively.1
- Risk of developing osteoarthritis increases with knee injury in adolescence or adulthood (relative risk [RR] = 2.95) and obesity (RR = 1.51 to 2.07).1
- Occupational physical activity and abnormal joint loading also increase the risk.1,2
Etiology and Pathophysiology
- Biomechanical factors and inflammation upset the balance of articular cartilage biosynthesis and degradation.
- Chondrocytes attempt to repair the damage; eventually, however, enzymes produced by the chondrocytes digest the matrix and accelerate cartilage erosion.
- Inflammatory molecules related to cytokine production, prostaglandin and arachidonic acid metabolism may be involved in susceptibility to osteoarthritis.3
Risk Factors
Diagnosis
The American College of Rheumatology uses the following criteria for the most common joints involved in osteoarthritis.
- Knee—Knee pain, osteophytes on radiograph, and 1 of 3: age older than 50 years, stiffness less than 30 minutes, or crepitus on physical examination (sensitivity = 91%, specificity = 86%).4
- Hip—Hip pain and 2 of 3: erythrocyte sedimentation rate (ESR) less than 20 mm/h; femoral or acetabular osteophytes by radiograph; superior, axial, or medial joint space narrowing by radiograph (sensitivity = 89%, specificity = 91%).5
- Hand—Hand pain, aching, or stiffness and 3 of 4: hard tissue enlargement of 2 or more DIP joints, fewer than 3 swollen metacarpophalangeal (MCP) joints, hand tissue enlargement of 2 or more selected joints, deformity of 1 or more selected joints. Selected joints include second and third DIP, second and third PIP, first carpometacarpal (CMC) on both hands (sensitivity = 94%, specificity = 87%).6
- Typically, joint pain is worsened with movement and relieved by rest. A small subset may demonstrate inflammatory symptoms including prolonged stiffness.
- Loss of function (i.e., impaired gait with knee or hip osteoarthritis, impaired manual dexterity with hand osteoarthritis).
- Radicular pain when vertebral column osteophytes impinge nerve roots.
- Bony enlargement of the DIP joints (Heberden nodes) or PIP joints (Bouchard nodes) (Figure 96-1).
- Not typically indicated. Normal ESR and synovial fluid white blood cell count (WBC) less than 2000/mm.3,4
- Imaging.
- Loss of joint space or osteophytes on radiographs (Figures 96-2, 96-3, 96-4, and 96-5).