http://evolve.elsevier.com/Edmunds/NP/
Thyroid Supplements
Thyroxine (T4) is the mainstay of treatment for uncomplicated hypothyroidism. T4 or triiodothyronine (T3) is used for suppressive treatment for conditions such as thyroid cancer. Treatment for hypothyroidism and suppressive treatment for individuals with a history of thyroid cancer generally require lifelong replacement with thyroid hormone.
Therapeutic Overview
Regulation of a basal metabolism is achieved through complex coordination of the hypothalamic-pituitary-thyroid feedback control system (Figure 52-1). T4 and T3 are released from the thyroid gland in response to circulating serum levels of thyroid stimulating hormone (TSH) secreted by the pituitary gland. In turn, TSH secretion is influenced by thyroid-releasing hormone (TRH) that is secreted by the hypothalamus. The feedback mechanism creates an inverse relationship between serum levels of T3-T4 and TSH-TRH. When T3 and T4 serum levels rise, TSH and TRH secretions are suppressed.
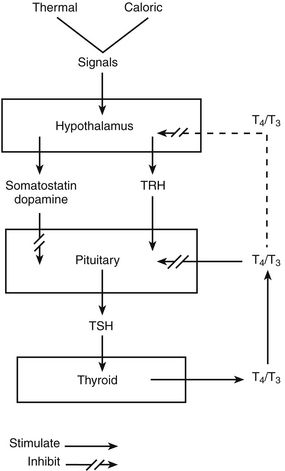
FIGURE 52-1 Regulation of thyroid-stimulating hormone secretion.
Thyroxine (T4) and triiodothyronine (T3) from the thyroid gland exert negative feedback on the pituitary by blocking the action of TRH. Negative feedback of T4 and T3 at the level of the hypothalamus is less well established. Somatostatin and dopamine each tonically inhibits TSH secretion. (From Berne RM, Levy MN: Physiology, ed 4, St Louis, 1998, Mosby; The Endocrine Society: Management of thyroid dysfunction during pregnancy and postpartum, 2007. Accessed at www.endo-society.org.)
TRH and TSH levels can be measured directly. An elevated TSH, along with low circulating levels of free (unbound) T3 and T4, is diagnostic of primary hypothyroidism. Conversely, a low or undetectable TSH with high circulating levels of free T3 and T4 is diagnostic of thyrotoxicosis. A low TSH accompanied by low T4 and T3 of a high TSH with high levels of T4 and T3 is characteristic or a central cause (secondary or tertiary) of hypothyroidism or thyrotoxicosis, respectively. Although rarely indicated, a stimulation test for TRH may be obtained if secondary hypothyroidism is suspected.
The thyroid gland releases T4 (90%), T3 (10%), and reverse T3 (rT3) (<1%). Elevated rT3 may be an indication of euthyroid sick syndrome. This test usually is reserved for use when standard thyroid function tests (TFTs) yield inconclusive results.
T3 and T4 have a high affinity for protein. T3 is 99.7% protein bound, whereas T4 is 99.97% protein bound. Only the unbound portion is metabolically active. In the peripheral tissue, T4 is converted to T3 through the removal of iodine. Therefore, in most cases, it is necessary to administer only T4 because the body will produce T3 from T4. The physiologic effects of thyroid hormones are attributed to the peripheral T3.
Thyroid hormones exert their effect on nearly every system of the body through a variety of mechanisms. Basal metabolic rate is regulated by thyroid hormones. Thyroid hormones also influence oxygen consumption, respiratory rate, body temperature, heart rate, stroke volume, enzyme system activity, the rate of fat, protein, and carbohydrate metabolism, and growth and maturation. They are especially important in central nervous development. Some research suggests that screening of pregnant women for thyroid disorders may actually interfere with the brain development and intelligence of some children.
Pathophysiology
In children, thyroid hormones are essential for overall normal growth and development. Without thyroid hormone, development of the central nervous system is impaired. Undetected deficiency of thyroid hormone may begin to affect children shortly after birth (as evidenced by cretinism).
Adults also may develop numerous problems related to a decreased metabolic rate. Cardiovascular, gastrointestinal, musculoskeletal, and neurologic function may be impaired by inadequate thyroid hormones.
Primary hypothyroidism, the most common form of hypothyroidism, is caused by a failure within the thyroid gland. Secondary hypothyroidism is caused by lack of TSH secretion from the pituitary. Tertiary hypothyroidism is caused by lack of TRH secretion from the hypothalamus.
Primary hypothyroidism has a variety of causes. One common cause is iatrogenic—that is, the result of therapy for thyrotoxicosis or other drugs such as lithium. Other causes include idiopathic thyroid atrophy and autoimmune destruction of the thyroid, such as Hashimoto’s thyroiditis or postpartum thyroid disease.
Disease Process
Hypothyroidism is the metabolic state that results from deficient thyroid hormones. In adults, it is most common in women and is characterized by signs and symptoms consistent with altered energy metabolism, such as fatigue, lethargy, sensitivity to cold, dry skin, and menstrual disturbances. If untreated, it can progress to life-threatening myxedema, with characteristic appearance and physical symptoms, especially of the skin, and cardiovascular instability.
Table 52-1 lists altered laboratory findings in thyroid dysfunction. TSH is the most sensitive and useful test in the diagnosis of hypothyroidism. Free T4 and T3 are also useful. The amount of circulating and unbound hormones is reduced in patients with this disorder.
Mechanism of Action
A thyroid supplement serves to replace inadequate levels of endogenous T3 and T4. If an exogenous thyroid hormone is given to a euthyroid patient, endogenous secretion of TSH and TRH will be suppressed, as will the body’s production of T3 and T4.
Basal metabolic rate and metabolism of carbohydrates, proteins, and fats are increased by thyroid supplements. These drugs also exert a direct effect on tissue (e.g., increased myocardial contraction).
Thyrogen is a recombinant DNA source of human TSH useful in the management and treatment of thyroid cancer patients.
Treatment Principles
Cardinal Points of Treatment
How to Monitor
See Tables 52-2 and 52-3.
TABLE 52-2
Laboratory Evaluation of Thyroid Disorders
| Test | Hormone Evaluated | Interpretation of Test Results |
| TRH (thyrotropin) | Thyrotropin-releasing hormone | Assesses the function of the hypothalamic-pituitary-thyroid axis. Most useful when other tests are inconclusive |
| TSH | Thyroid-stimulating hormone | Assesses the function of the hypothalamic-pituitary-thyroid axis |
| TBG (thyroglobulin) | Thyroxine-binding globulin | As the primary protein for hormone binding, it is most useful for evaluating discrepancies in clinical findings and other serum hormone levels |
| T4 (T4 RIA, thyroxine) | Tetraiodothyronine, thyroxine | Concentration of bound and unbound thyroid hormone (T4) in the serum |
| FT4 | Free thyroxine, free T4 | Concentration of unbound thyroid hormone (T4) in the serum. It is most helpful for diagnosis when TBG level is abnormal. |
| T3 (T3 RIA) | Triiodothyronine | Concentration of bound and unbound thyroid hormone (T3) in the serum |
| FT3 | Free triiodothyronine, free T3 | Concentration of unbound, active T3 in the serum |
| T3-U (T3 RU) | Resin T3 uptake | Indirectly measures the concentration of thyroglobulin (TBG) by measuring the empty TBG binding sites in serum. Direct measurement of TBG may be more useful. |
| rT3 | Reverse T3 | A T3 antagonist, rT3 can be increased in euthyroid sick syndrome. |
| FTI (F T4-I, T7, T12) | Free T4 index | Derived by multiplying T4 and T3-U, it reflects the free (unbound) T4 in serum. This test essentially has been replaced by direct FT3 and FT4 measurements. |
| LATS | Long-acting thyroid stimulator | A positive test supports the diagnosis of Graves’ disease. |
| Antithyroid antibodies | Antithyroglobulin antibodies and/or antithyroid peroxidase antibodies Anti-TSH receptor antibodies | High titers in individuals with Hashimoto’s thyroiditis and Graves’ disease High titers in individuals with Graves’ disease |
TABLE 52-3
Normal Range for Thyroid Function Laboratory Tests
| Name of Test | Normal Range for Values |
| TRH (thyrotropin-releasing hormone) | Males: 14-24 mcg/ml Females: 16-26 mcg/ml |
| TSH (thyroid-stimulating hormone) | Newborn: <20 mcg/ml Adult: 0.30-5.5 mcg/ml |
| TBG (thyroglobulin) | 16-34 micro units/ml |
| T4 (thyroxine) | Newborn: 6.4-23.2 mcg/ml Child (1-10 yr): 6.4-15 mcg/ml Adult: 5-12 mcg/ml |
| FT4 (free thyroxine) | 0.9-1.7 ng/dl |
| T3 (triiodothyronine) | Newborn: 32-250 ng/ml Child (1-10 yr): 94-269 ng/ml Adult: 95-190 ng/ml |
| FT3 (free triiodothyronine) | 0.2-0.52 ng/dl |
| T3-U (resin T3 uptake) | 25%-35% |
| FTI (free thyroxine index) | 1.3-4.2 |
| Antithyroid antibodies: Anti-TBG antimicrosomal | Negative or titer <1:100 |
| LATS (long-acting thyroid stimulator) | Negative |
The test for T4 measures total thyroxine, both bound and unbound in the serum. Free thyroxine (FT4) measures only unbound T4. Normally, only T4 must be measured; thyroid-binding globulin (TBG) is the protein to which thyroid hormones are bound. It can be measured directly by the TBG test. Resin T3 uptake (T3 RU) is an indirect measure that is no longer used. If the patient has an abnormal TBG, free T4 may have to be evaluated.
Usually, measuring the TSH within 4 to 6 weeks is sufficient. Full therapeutic effectiveness may not be achieved for 3 to 6 weeks. TSH and symptom review usually are monitored monthly until normal and stable. Annual evaluation is recommended once maintenance therapy has been achieved. Levels also should be evaluated whenever patients experience signs and/or symptoms that could be related to underdosage/overdosage.
Children younger than 3 years of age should be maintained on the upper end of the T4 therapeutic range with a normal serum TSH. It is recommended that children undergo laboratory assessment of medication effectiveness every 1 to 2 months for the first year, every 2 to 3 months from 1 to 3 years old, and every 3 to 12 months thereafter.
Patients with a history of thyroid cancer who have had partial or total removal of their thyroid gland must take thyroid hormone supplements to suppress endogenous levels of TSH and to regulate their metabolism. However, a high level of TSH in a patient’s bloodstream is necessary for radioiodine imaging to detect remnant thyroid tissue or metastatic disease, and for optimal sensitivity of serum thyroglobulin testing to be achieved. In the past, patients had to stop taking their hormone supplements for 2 to 6 weeks prior to testing, causing them to experience symptoms of thyroid deficiency. Thyrogen, which is a recombinant form of TSH, allows the patients to avoid hormone withdrawal and its debilitating effects while they are undergoing diagnostic testing. Specifically, thyrogen is a new diagnostic agent for adjunctive use in serum thyroglobulin testing with or without radioiodine imaging in the follow-up of patients with well-differentiated thyroid cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Top 100 drug. Thyroid supplements will be discussed separately from thyroid suppressants.
Top 100 drug. Thyroid supplements will be discussed separately from thyroid suppressants.