http://evolve.elsevier.com/Edmunds/NP/
This chapter discusses the angiotensin receptor blockers (ACEIs) and the angiotensin receptor blockers (ARBs) as a unit because these drugs are quite similar in terms of their therapeutic uses, mechanisms of action, and adverse effects. Key distinctions are noted.
ACEIs and ARBs are commonly used in the treatment of patients with hypertension. In addition, these drugs have been shown to prolong survival in patients with heart failure, coronary heart disease, and acute MI. They slow the rate of progression of chronic renal failure and, particularly, diabetic nephropathy.
Therapeutic Overview
For an overview of the disorders indicative of treatment with ACEIs and ARBs, see the respective chapters (Table 22-1).
Mechanism of Action
Two types of angiotensin receptors have been identified: AT1 and AT2. Most of the biologic effects of angiotensin II are mediated by the AT1 receptor. AT2 receptors may exert antiproliferative and vasodilatory effects. ACEIs block angiotensin-converting enzyme (ACE), which is responsible for the conversion of angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor and is a stimulus for aldosterone release from the adrenal glands (Figure 22-1). Reduction in aldosterone secretion results in less water absorption and sodium/potassium exchange in the distal renal tubule, causing a slight increase in serum potassium.
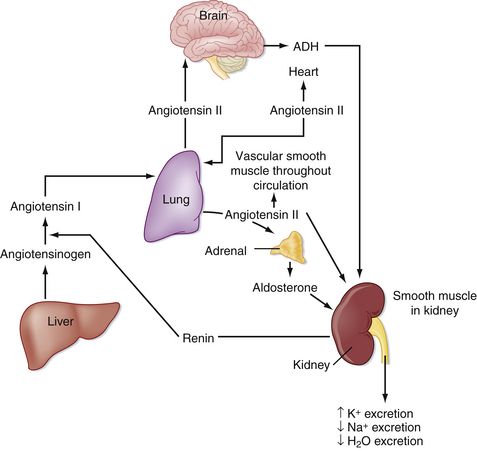
FIGURE 22-1 Essential components of the renin-angiotensin-aldosterone system. (Modified from Koeppen BM, Stanton BA: Physiology, ed 6, St Louis, 2008, Mosby.)
ACEIs inhibit the breakdown of bradykinin, a potent and naturally occurring vasodilator, by blocking the enzyme kininase II. This is thought to be the cause of the cough commonly experienced by patients who take this class of drugs.
ARBs block the effects of angiotensin II by blocking the binding of angiotensin II to its receptors. They do not affect bradykinin (Figure 22-2). Receptor affinity is highest by candesartan > irbesartan > eprosartan > telmisartan> valsartan > losartan.
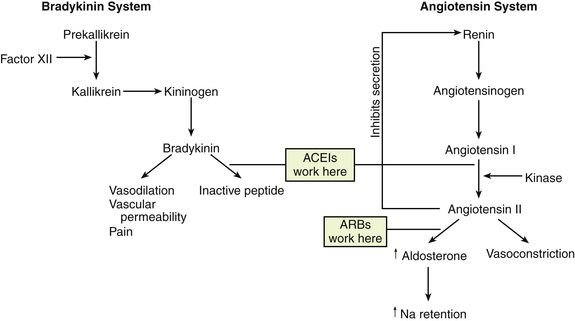
FIGURE 22-2 Sites of action of angiotensin-converting enzyme inhibitors (ACEIs) and receptor antagonists. (Modified from McCance KL, Huether SE: Pathophysiology, ed 5, St Louis, 2005, Mosby.)
ARBs differ from ACEIs in the following four respects:
Whether these differences translate to significant clinical outcomes is unknown.
The pharmacologic effects of ACE inhibition produce a reduction in systemic vascular resistance, with no effect or a moderate increase in cardiac output. Blood pressure is lowered through decreased systemic vascular resistance. Blood pressure reduction is not accompanied by changes in heart rate. Renal perfusion is increased and renal vascular resistance is decreased, but the glomerular filtration rate is usually unchanged. In patients with heart failure syndrome, ACEIs significantly decrease preload by reducing sodium and water retention (through reduction of aldosterone secretion) and reduce afterload through their effects on angiotensin II (decreasing systemic vascular resistance). This causes a modest increase in ejection fraction and a decrease in ventricular end-diastolic pressure and volume. These in turn improve myocardial energy metabolism. ACEIs also act on the renal vasculature to reduce arteriolar resistance, which improves renal hemodynamics. This may improve the course of patients with diabetic nephropathy and other renal diseases with glomerular hypertension. The ACE escape phenomenon may be seen in some patients when alternate enzyme pathways are used for formation of angiotensin II, thus increasing the benefit of ARBs.
Treatment Principles
For information on standardized treatment guidelines, for evidence supporting these guidelines, and for information on nonpharmacologic treatment for patients with hypertension, MI, chronic heart failure, and diabetic nephropathy, see the related chapters: Chapters 17, 18, 19, and 53. In this chapter, only pharmacologic treatment with ACEIs and ARBs is discussed.
ACEIs have similar therapeutic and adverse reactions. They differ basically in terms of pharmacokinetics (Table 22-2). Some are provided as prodrugs that must be metabolized by the liver to the active drug. The duration of hypotensive effects is critical. Many products claim that they provide 24-hour protection, but their effects may wear off within 24 hours. Blood pressure (BP) should be checked shortly before the time of administration to ensure 24-hour BP control. These agents differ in terms of tissue distribution, and this may result in differences in the renin-angiotensin systems affected. Except for fosinopril, these agents are cleared predominantly by the kidney. ACEIs generally are considered safe and effective in patients with mild to moderate renal impairment; however, dosage reduction is required in patients whose renal clearance is diminished. Fosinopril, lisinopril, and ramipril are eliminated by both hepatic and renal mechanisms, and they have the ability to compensate for renal dysfunction by shifting to hepatic elimination. Dehydration and renal insufficiency increase the risk of elevated K when an ACEI is started.
An advantage of ACEIs and ARBs is their relative lack of serious adverse reactions compared with other drugs for hypertension and angina. The most common and often treatment-limiting side effect of the ACEIs is cough. This cough is persistent, dry, and hacking and is seen in up to 20% of patients taking ACEIs. The ARBs were developed, in part, to eliminate this side effect, and clinical trials have demonstrated this benefit. The most serious and potentially life-threatening adverse reaction is angioedema, which occurs in approximately 0.1% to 0.7% of patients. However, because ACEIs are used so often, current clinical practice guidelines suggest that the use of an ACEI should be ruled out for anyone who comes into an emergency department with angioedema. The main distinguishing clinical features of ACEI-induced angioedema were older age and absence of an allergic history. ARBs are often reserved as alternatives to ACEIs for patients who cannot tolerate an ACEI; in addition, overall costs are reduced because of the availability of generic ACEIs.
Other serious adverse effects of the ACEIs and the ARBs include hyperkalemia, hypotension, and acute renal failure. Abrupt withdrawal of these agents has not resulted in rebound hypertension.
Hypertension
The antihypertensive effects of the ARBs have proved comparable with those of the ACEIs. ACEIs and ARBs are of particular value for the treatment of hypertensive patients who have concomitant illnesses such as diabetes, renal insufficiency, left ventricular dysfunction, and CHF. Fifty to 60 percent of white patients will have a good response to an ACEI; this is comparable with results reported with other first-line antihypertensive drugs. Some African American patients do not appear to respond as well as whites in terms of BP reduction, but cardioprotective or nephroprotective effects can still be seen. The addition of a low-dose thiazide diuretic often allows for efficacy in blood pressure lowering that is comparable with that seen in whites. BP reduction may be progressive, with maximal effects achieved in 2 to 4 weeks.
An additional advantage of ACEIs is regression of left ventricular hypertrophy. However, in ALLHAT (the Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial), an ACEI was shown to be less cardioprotective than a thiazide diuretic. ACEIs have been shown to increase insulin sensitivity and to modestly lower plasma glucose levels. They also minimize or prevent diuretic-induced elevations in cholesterol and uric acid levels.
Another possible benefit of ACEIs (although not yet substantiated with robust clinical research) may be their ability to reduce the incidence of new-onset diabetes. Multiple clinical trials, such as CHARM (Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity), LIFE (Losartan Intervention For Endpoint reduction), HOPE (Heart Outcomes Prevention Evaluation study), ANBP2 (Second Australian National Blood Pressure trial), ALLHAT, and VALUE (Valsartan Antihypertensive Long-term Use Evaluation), suggest that ACEIs are more likely to prevent diabetes than are other antihypertensive agents. Three major trials are currently under way to determine whether ACEIs and ARBs or combination therapy is more effective than are other antihypertensives in preventing the onset of diabetes. Their action may be complicated by the use of statins, which may increase the risk of diabetes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Top 100 drug;
Top 100 drug;  key drug.
key drug.