High-Yield Terms to Learn
Goiter Enlargement of the thyroid gland Graves’ disease Autoimmune disorder that results in hyperthyroidism during the early phase and can progress to hypothyroidism if there is destruction of the gland in later phases Thyroglobulin A protein synthesized in the thyroid gland; its tyrosine residues are used to synthesize thyroid hormones Thyroid-stimulating hormone (TSH) The anterior pituitary hormone that regulates thyroid gland growth, uptake of iodine and synthesis of thyroid hormone Thyroid storm Severe thyrotoxicosis Thyrotoxicosis Medical syndrome caused by an excess of thyroid hormone (Table 38-1) Thyroxine-binding globulin (TBG) Protein synthesized in the liver that transports thyroid hormone in the blood
Thyroid Hormones
Synthesis & Transport of Thyroid Hormones
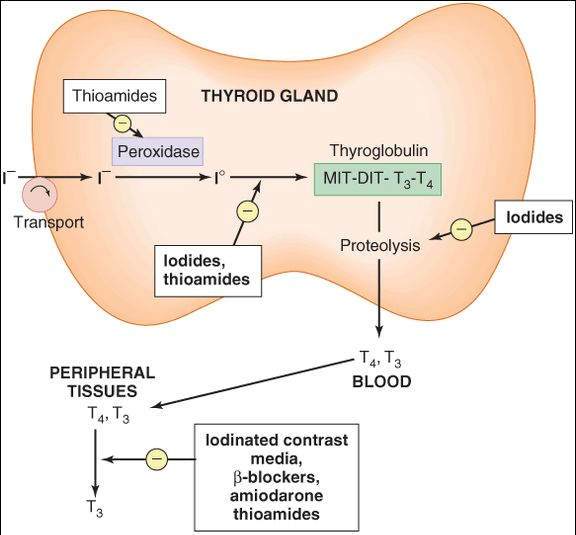
The thyroid secretes 2 iodine-containing hormones: thyroxine (T4 ) and triiodothyronine (T3). The iodine necessary for the synthesis of these molecules comes from food or iodide supplements. Iodide ion is actively taken up by and highly concentrated in the thyroid gland, where it is converted to elemental iodine by thyroidal peroxidase (Figure 38-1). The protein thyroglobulin serves as a scaffold for thyroid hormone synthesis. Tyrosine residues in thyroglobulin are iodinated to form monoiodotyrosine (MIT) or diiodotyrosine (DIT) in a process known as iodineorganification. Within thyroglobulin, 2 molecules of DIT combine to form T4, while 1 molecule each of MIT and DIT combine to form T3. Proteolysis of thyroglobulin liberates the T4 and T3, which are then released from the thyroid. After release from the gland, T4 and T3 are transported in the blood by thyroxine-binding globulin, a protein synthesized in the liver.
FIGURE 38-1
Sites of action of some antithyroid drugs. I-, iodide ion; I°, elemental iodine. Not shown: radioactive iodine (131I), which destroys the gland through radiation.
(Modified and reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 38-1.)
Thyroid function is controlled by the pituitary through the release of thyrotropin (thyroid-stimulating hormone [TSH]) (see Figure 37-1) and by the availability of iodide. Thyrotropin stimulates the uptake of iodide as well as synthesis and release of thyroid hormone. It also has a growth-promoting effect that causes thyroid cell hyperplasia and an enlarged gland (goiter). High levels of thyroid hormones inhibit the release of TSH, providing an effective negative feedback control mechanism. In Graves’ disease, an autoimmune disorder, B lymphocytes produce an antibody that activates the TSH receptor and can cause a syndrome of hyperthyroidism called thyrotoxicosis. Because these lymphocytes are not susceptible to negative feedback, patients with Graves’ disease can have very high blood concentrations of thyroid hormone at the same time that their blood concentrations of TSH are very low.
Mechanisms of Action of T4 and T3
T3 is about 10 times more potent than T4 . Because T4 is converted to T3 in target cells, the liver, and the kidneys, most of the effect of circulating T4 is probably due to T3. Thyroid hormones bind to intracellular receptors that control the expression of genes responsible for many metabolic processes. The proteins synthesized under T3 control differ depending on the tissue involved; these proteins include, for example, Na+/K+ ATPase, specific contractile proteins in smooth muscle and the heart, enzymes involved in lipid metabolism, and important developmental components in the brain. T3 may also have a separate membrane receptor-mediated effect in some tissues.
Effects of Thyroid Hormone
The organ-level actions of the thyroid hormones include normal growth and development of the nervous, skeletal, and reproductive systems and control of metabolism of fats, carbohydrates, proteins, and vitamins. The key features of excess thyroid activity (thyrotoxicosis) and hypothyroidism are listed in Table 38-1.
TABLE 38-1 Key features of thyrotoxicosis and hypothyroidism.
Thyrotoxicosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree