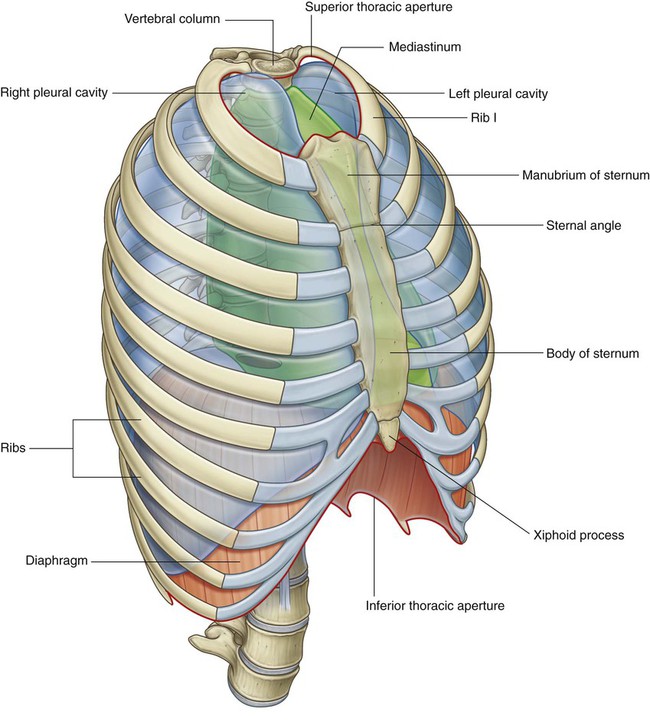
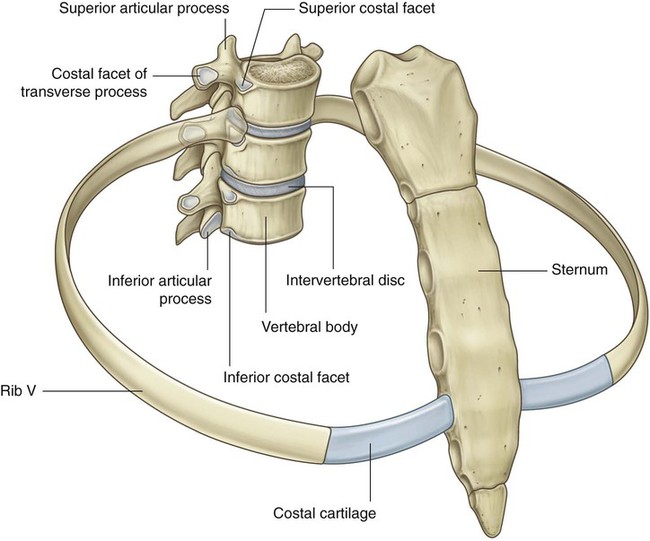
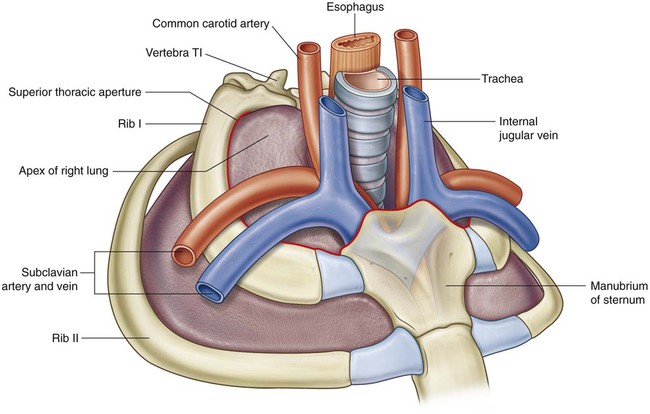
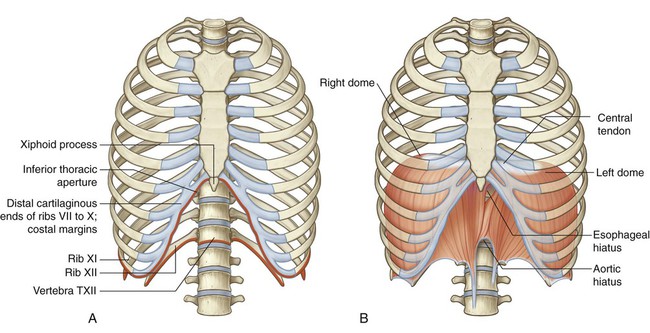
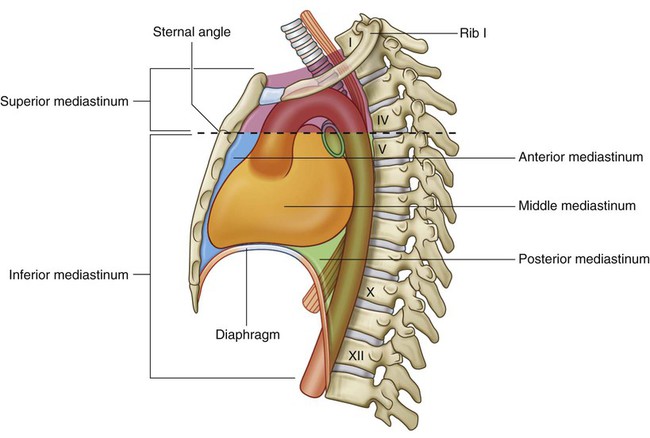
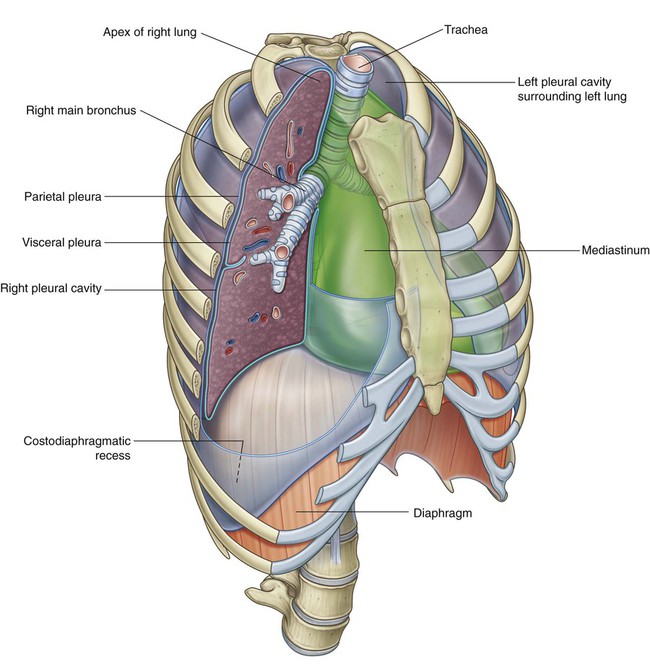
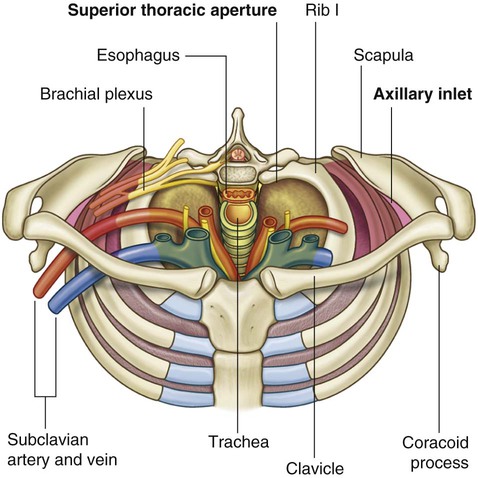
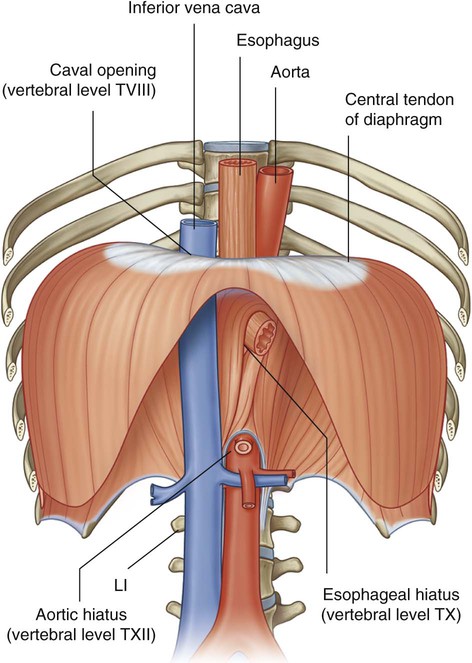
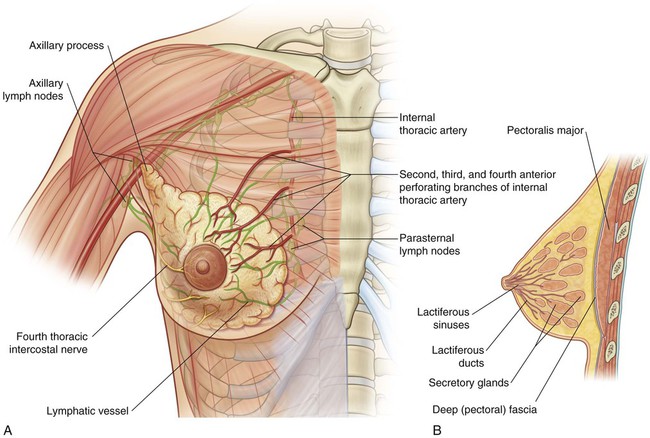
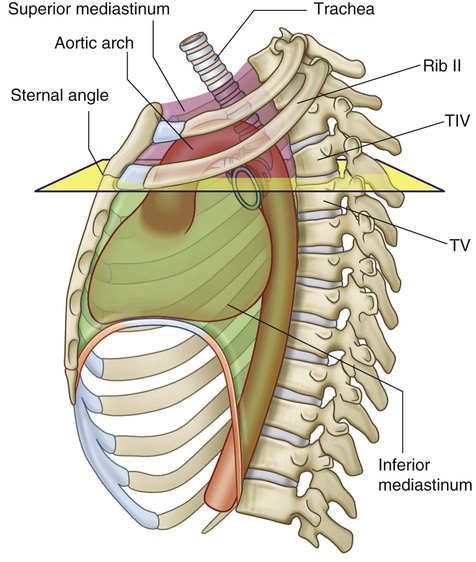
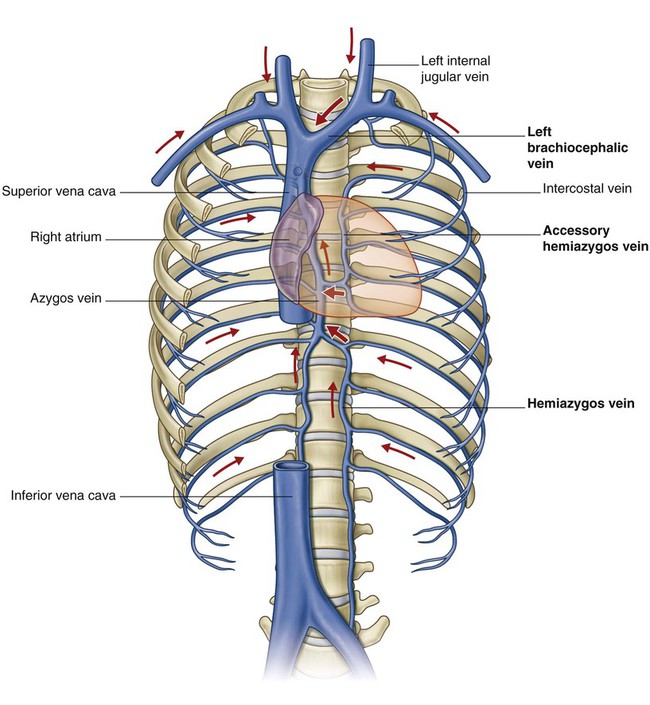
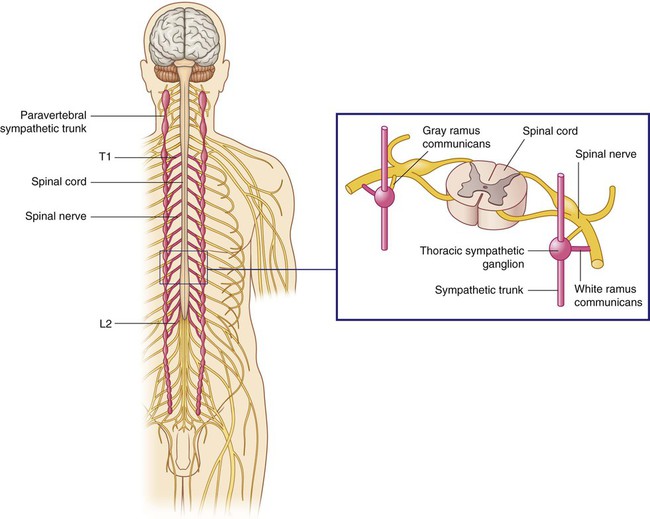
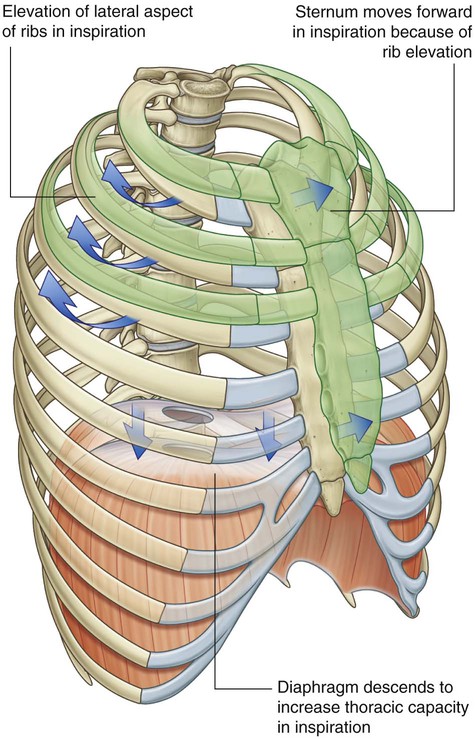
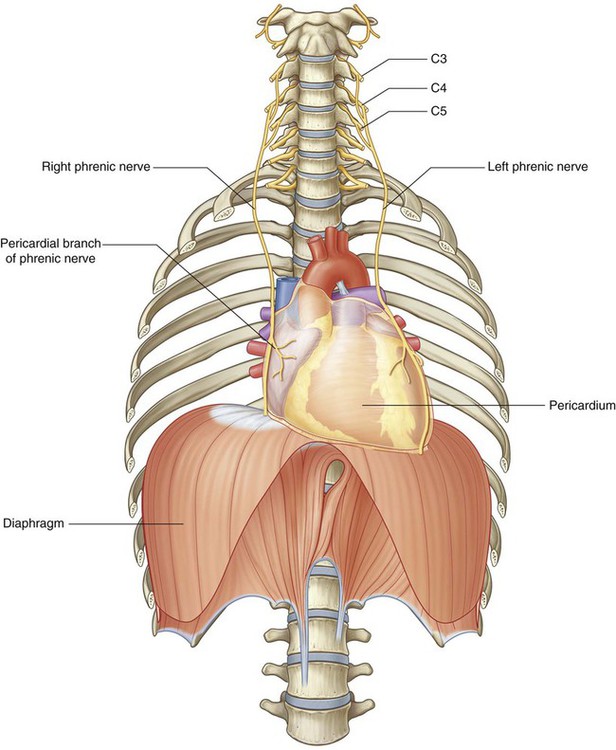
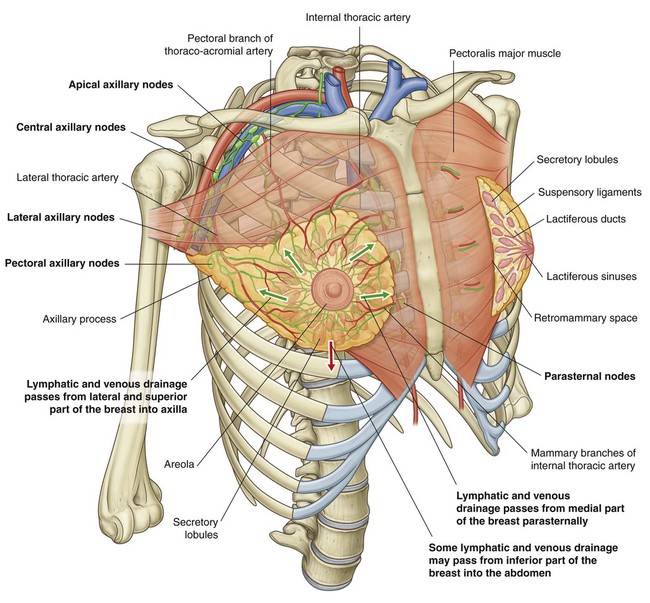
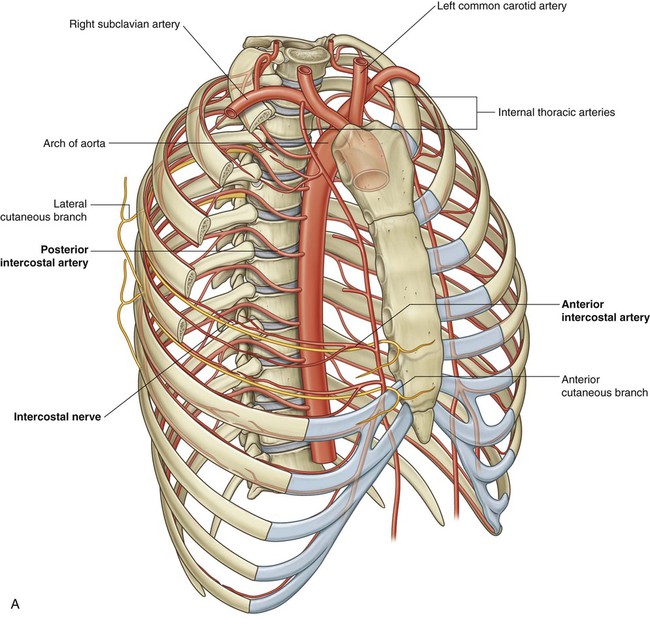
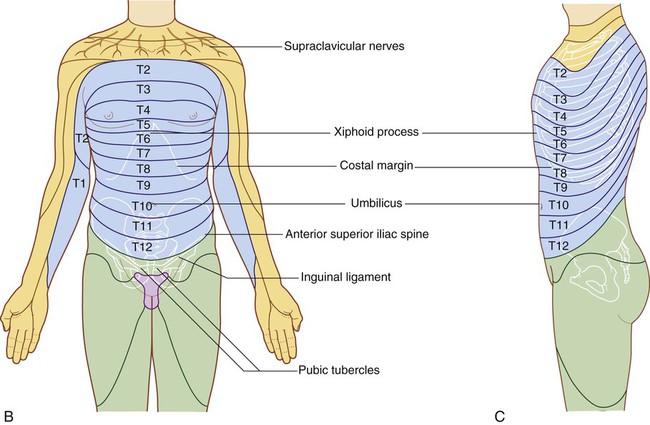
The thorax is an irregularly shaped cylinder with a narrow opening (superior thoracic aperture) superiorly and a relatively large opening (inferior thoracic aperture) inferiorly (Fig. 3.1). The superior thoracic aperture is open, allowing continuity with the neck; the inferior thoracic aperture is closed by the diaphragm. The thoracic wall consists of skeletal elements and muscles (Fig. 3.1): All ribs articulate with thoracic vertebrae posteriorly. Most ribs (from rib II to IX) have three articulations with the vertebral column. The head of each rib articulates with the body of its own vertebra and with the body of the vertebra above (Fig. 3.2). As these ribs curve posteriorly, each also articulates with the transverse process of its vertebra. Anteriorly, the costal cartilages of ribs I to VII articulate with the sternum. The inferior thoracic aperture is large and expandable. Bone, cartilage, and ligaments form its margin (Fig. 3.4A). Skeletal elements of the inferior thoracic aperture are: When viewed anteriorly, the inferior thoracic aperture is tilted superiorly. A horizontal plane passing through the sternal angle and the intervertebral disc between vertebrae TIV and TV separates the mediastinum into superior and inferior parts (Fig. 3.5). The inferior part is further subdivided by the pericardium, which encloses the pericardial cavity surrounding the heart. The pericardium and heart constitute the middle mediastinum. The superior thoracic aperture opens directly into the root of the neck (Fig. 3.7). An axillary inlet, or gateway to the upper limb, lies on each side of the superior thoracic aperture. These two axillary inlets and the superior thoracic aperture communicate superiorly with the root of the neck (Fig. 3.7). Each axillary inlet is formed by: The base of the axillary inlet’s triangular opening is the lateral margin of rib I. The diaphragm separates the thorax from the abdomen. Structures that pass between the thorax and abdomen either penetrate the diaphragm or pass posteriorly to it (Fig. 3.8): The breasts, consisting of secretory glands, superficial fascia, and overlying skin, are in the pectoral region on each side of the anterior thoracic wall (Fig. 3.9). Vessels, lymphatics, and nerves associated with the breast are as follows: The horizontal plane passing through the disc that separates thoracic vertebrae TIV and TV is one of the most significant planes in the body (Fig. 3.10) because it: The right atrium is the chamber of the heart that receives deoxygenated blood returning from the body. It lies on the right side of the midline, and the two major veins, the superior and inferior venae cavae, that drain into it are also located on the right side of the body. This means that, to get to the right side of the body, all blood coming from the left side has to cross the midline. This left-to-right shunting is carried out by a number of important and, in some cases, very large veins, several of which are in the thorax (Fig. 3.11). Posterior and anterior intercostal vessels branch segmentally from these arteries and pass laterally around the wall, mainly along the inferior margin of each rib (Fig. 3.12A). Running with these vessels are intercostal nerves (the anterior rami of thoracic spinal nerves), which innervate the wall, related parietal pleura, and associated skin. The position of these nerves and vessels relative to the ribs must be considered when passing objects, such as chest tubes, through the thoracic wall. Dermatomes of the thorax generally reflect the segmental organization of the thoracic spinal nerves (Fig. 3.12B). The exception occurs, anteriorly and superiorly, with the first thoracic dermatome, which is located mostly in the upper limb, and not on the trunk. Dermatomes of T7 to T12 follow the contour of the ribs onto the anterior abdominal wall (Fig. 3.12C). All preganglionic nerve fibers of the sympathetic system are carried out of the spinal cord in spinal nerves T1 to L2 (Fig. 3.13). This means that sympathetic fibers found anywhere in the body ultimately emerge from the spinal cord as components of these spinal nerves. Preganglionic sympathetic fibers destined for the head are carried out of the spinal cord in spinal nerve T1. The cylindrical thorax consists of: The breasts consist of mammary glands and associated skin and connective tissues. The mammary glands are modified sweat glands in the superficial fascia anterior to the pectoral muscles and the anterior thoracic wall (Fig. 3.16). Lymphatic drainage of the breast is as follows: Each pectoral region contains the pectoralis major, pectoralis minor, and subclavius muscles (Fig. 3.17 and Table 3.1). All originate from the anterior thoracic wall and insert into bones of the upper limb. Table 3.1 Muscles of the pectoral region
Thorax
Conceptual overview
General description
Component parts
Thoracic wall
 Posteriorly, it is made up of twelve thoracic vertebrae and their intervening intervertebral discs;
Posteriorly, it is made up of twelve thoracic vertebrae and their intervening intervertebral discs;
 Laterally, the wall is formed by ribs (twelve on each side) and three layers of flat muscles, which span the intercostal spaces between adjacent ribs, move the ribs, and provide support for the intercostal spaces;
Laterally, the wall is formed by ribs (twelve on each side) and three layers of flat muscles, which span the intercostal spaces between adjacent ribs, move the ribs, and provide support for the intercostal spaces;
 Anteriorly, the wall is made up of the sternum, which consists of the manubrium of sternum, body of sternum, and xiphoid process.
Anteriorly, the wall is made up of the sternum, which consists of the manubrium of sternum, body of sternum, and xiphoid process.
Inferior thoracic aperture
 the body of vertebra TXII posteriorly,
the body of vertebra TXII posteriorly,
 rib XII and the distal end of rib XI posterolaterally,
rib XII and the distal end of rib XI posterolaterally,
 the distal cartilaginous ends of ribs VII to X, which unite to form the costal margin anterolaterally, and
the distal cartilaginous ends of ribs VII to X, which unite to form the costal margin anterolaterally, and
Mediastinum
Relationship to other regions
Neck
Upper limb
Abdomen
 The inferior vena cava pierces the central tendon of the diaphragm to enter the right side of the mediastinum near vertebral level TVIII.
The inferior vena cava pierces the central tendon of the diaphragm to enter the right side of the mediastinum near vertebral level TVIII.
 The esophagus penetrates the muscular part of the diaphragm to leave the mediastinum and enter the abdomen just to the left of the midline at vertebral level TX.
The esophagus penetrates the muscular part of the diaphragm to leave the mediastinum and enter the abdomen just to the left of the midline at vertebral level TX.
 The aorta passes posteriorly to the diaphragm at the midline at vertebral level TXII.
The aorta passes posteriorly to the diaphragm at the midline at vertebral level TXII.
 Numerous other structures that pass between the thorax and abdomen pass through or posterior to the diaphragm.
Numerous other structures that pass between the thorax and abdomen pass through or posterior to the diaphragm.
Breast
 Branches from the internal thoracic arteries and veins perforate the anterior chest wall on each side of the sternum to supply anterior aspects of the thoracic wall. Those branches associated mainly with the second to fourth intercostal spaces also supply the anteromedial parts of each breast.
Branches from the internal thoracic arteries and veins perforate the anterior chest wall on each side of the sternum to supply anterior aspects of the thoracic wall. Those branches associated mainly with the second to fourth intercostal spaces also supply the anteromedial parts of each breast.
 Lymphatic vessels from the medial part of the breast accompany the perforating arteries and drain into the parasternal nodes on the deep surface of the thoracic wall.
Lymphatic vessels from the medial part of the breast accompany the perforating arteries and drain into the parasternal nodes on the deep surface of the thoracic wall.
 Vessels and lymphatics associated with lateral parts of the breast emerge from or drain into the axillary region of the upper limb.
Vessels and lymphatics associated with lateral parts of the breast emerge from or drain into the axillary region of the upper limb.
 Lateral and anterior branches of the fourth to sixth intercostal nerves carry general sensation from the skin of the breast.
Lateral and anterior branches of the fourth to sixth intercostal nerves carry general sensation from the skin of the breast.
Key features
Vertebral level TIV/V
 passes through the sternal angle anteriorly, marking the position of the anterior articulation of the costal cartilage of rib II with the sternum. The sternal angle is used to find the position of rib II as a reference for counting ribs (because of the overlying clavicle, rib I is not palpable);
passes through the sternal angle anteriorly, marking the position of the anterior articulation of the costal cartilage of rib II with the sternum. The sternal angle is used to find the position of rib II as a reference for counting ribs (because of the overlying clavicle, rib I is not palpable);
 separates the superior mediastinum from the inferior mediastinum and marks the position of the superior limit of the pericardium;
separates the superior mediastinum from the inferior mediastinum and marks the position of the superior limit of the pericardium;
 marks where the arch of the aorta begins and ends;
marks where the arch of the aorta begins and ends;
 passes through the site where the superior vena cava penetrates the pericardium to enter the heart;
passes through the site where the superior vena cava penetrates the pericardium to enter the heart;
 is the level at which the trachea bifurcates into right and left main bronchi; and
is the level at which the trachea bifurcates into right and left main bronchi; and
Venous shunts from left to right
Segmental neurovascular supply of thoracic wall
 the thoracic aorta, which is in the posterior mediastinum, and
the thoracic aorta, which is in the posterior mediastinum, and
 a pair of vessels, the internal thoracic arteries, which run along the deep aspect of the anterior thoracic wall on either side of the sternum.
a pair of vessels, the internal thoracic arteries, which run along the deep aspect of the anterior thoracic wall on either side of the sternum.
Sympathetic system
Regional anatomy
Pectoral region
 a superficial compartment containing skin, superficial fascia, and breasts; and
a superficial compartment containing skin, superficial fascia, and breasts; and
 a deep compartment containing muscles and associated structures.
a deep compartment containing muscles and associated structures.
Breast
Lymphatic drainage
 Approximately 75% is via lymphatic vessels that drain laterally and superiorly into axillary nodes (Fig. 3.16).
Approximately 75% is via lymphatic vessels that drain laterally and superiorly into axillary nodes (Fig. 3.16).
 Most of the remaining drainage is into parasternal nodes deep to the anterior thoracic wall and associated with the internal thoracic artery.
Most of the remaining drainage is into parasternal nodes deep to the anterior thoracic wall and associated with the internal thoracic artery.
 Some drainage may occur via lymphatic vessels that follow the lateral branches of posterior intercostal arteries and connect with intercostal nodes situated near the heads and necks of ribs.
Some drainage may occur via lymphatic vessels that follow the lateral branches of posterior intercostal arteries and connect with intercostal nodes situated near the heads and necks of ribs.
Muscles of the pectoral region
Muscle
Origin
Insertion
Innervation
Function
Pectoralis major
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access