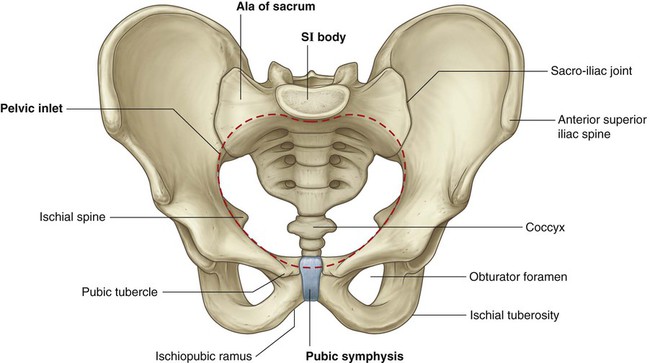
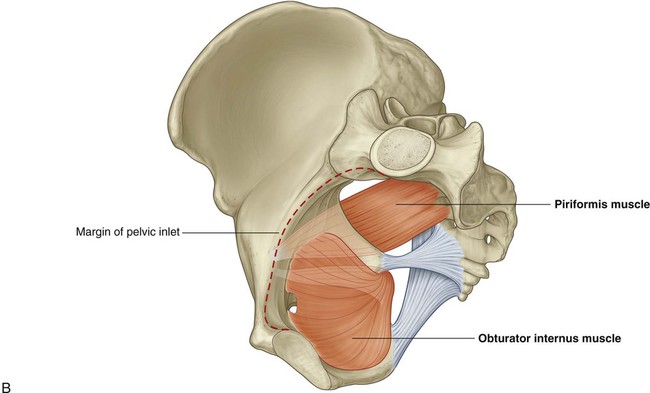
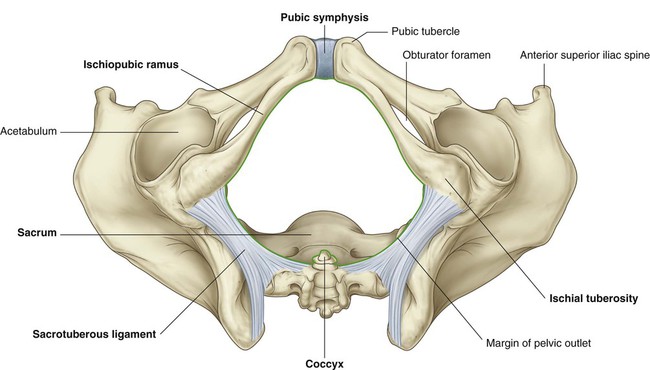
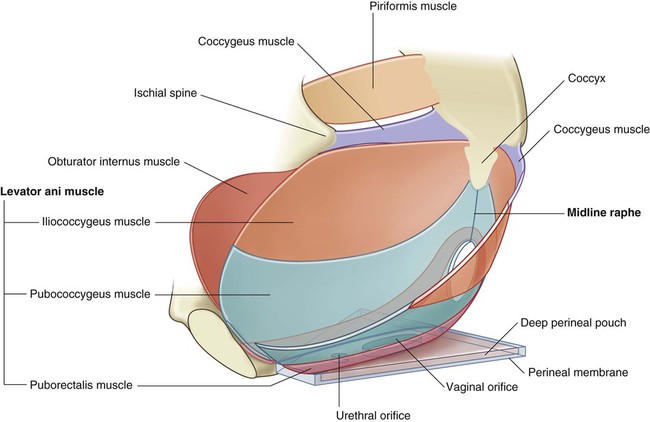
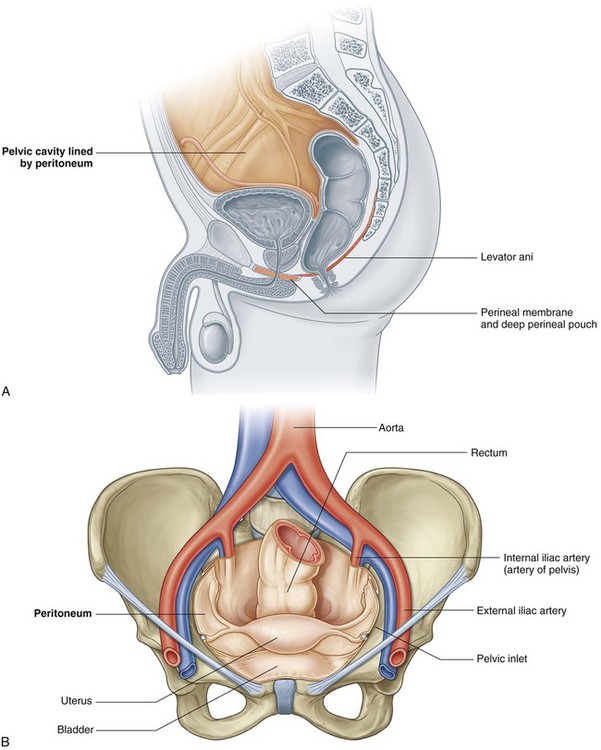
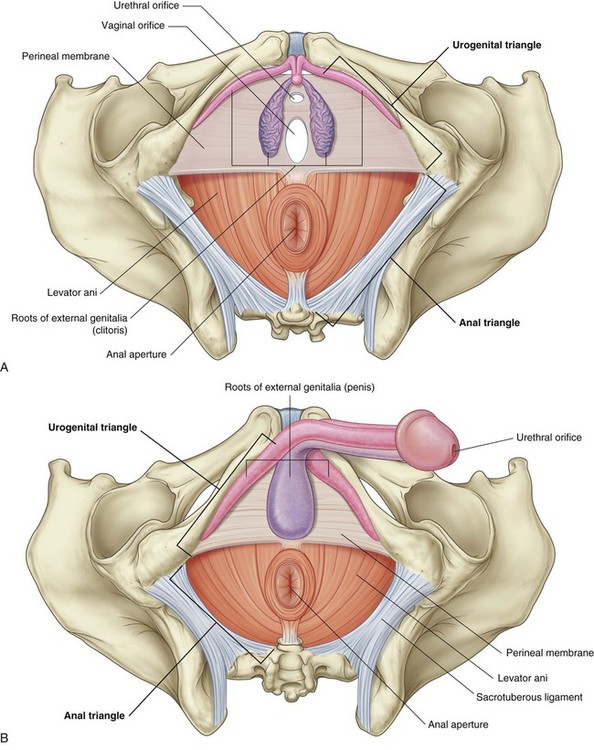
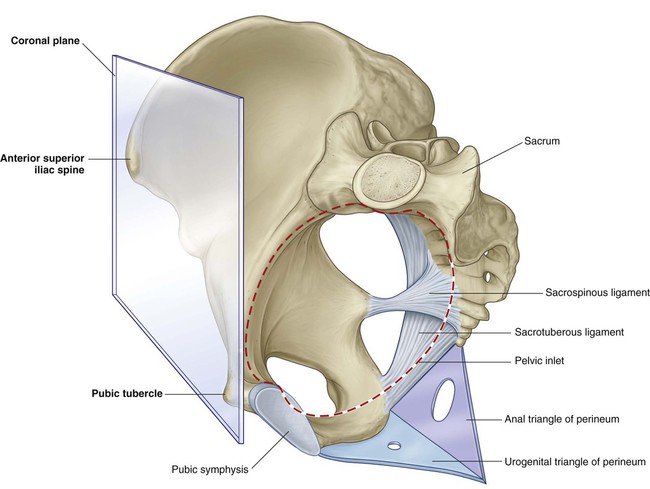
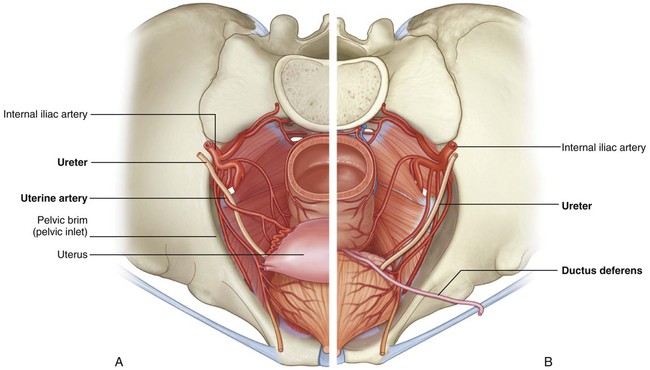
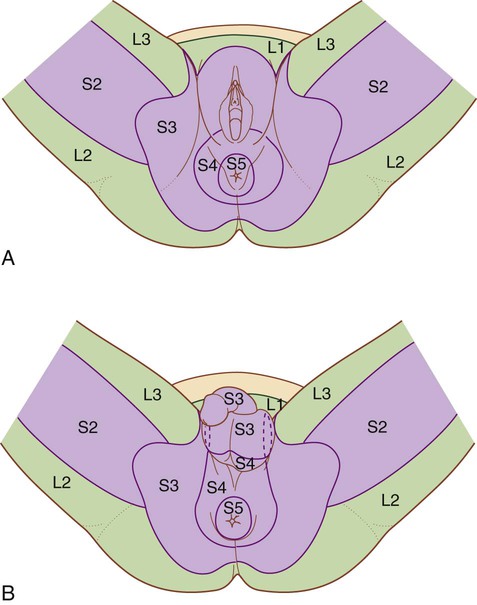
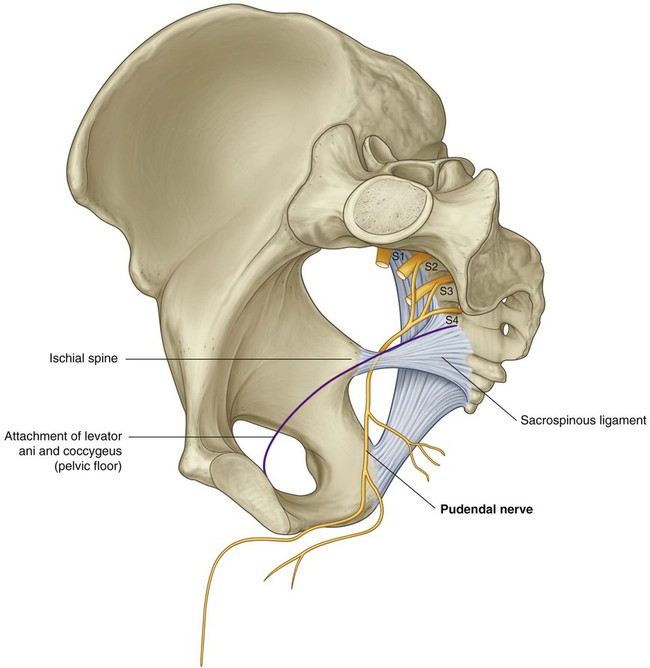
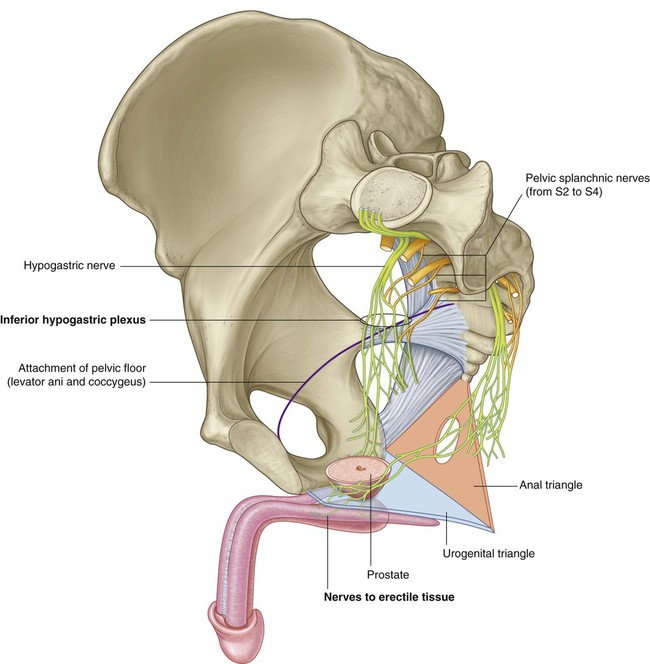
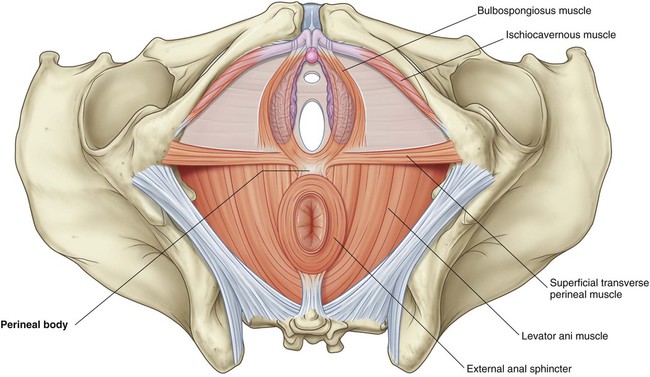
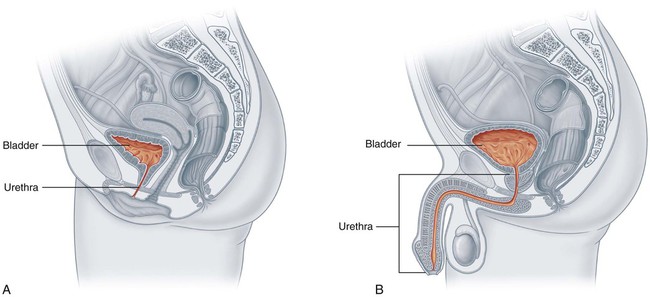
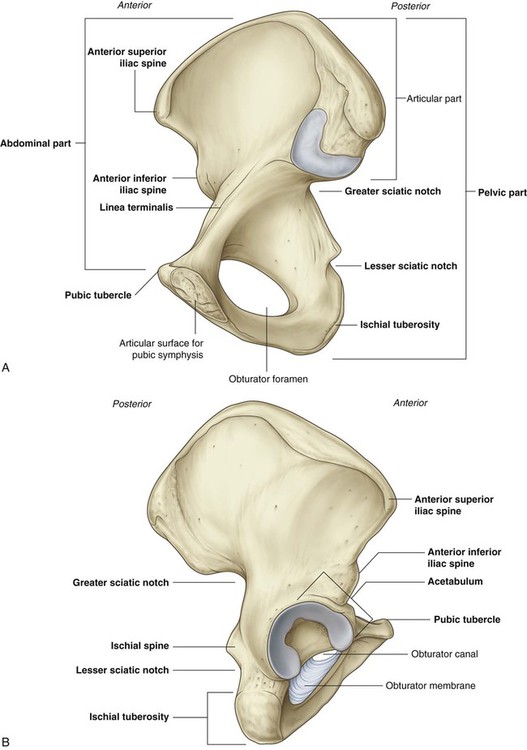
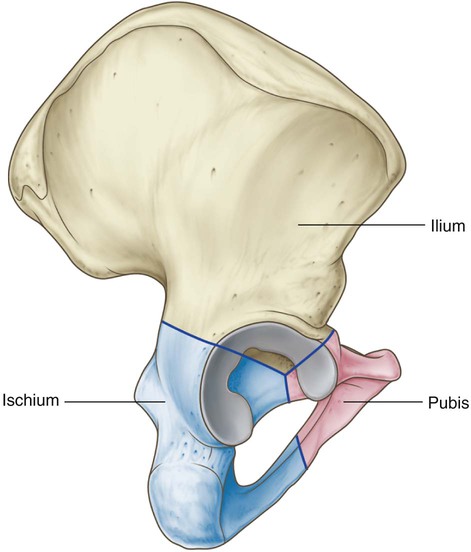
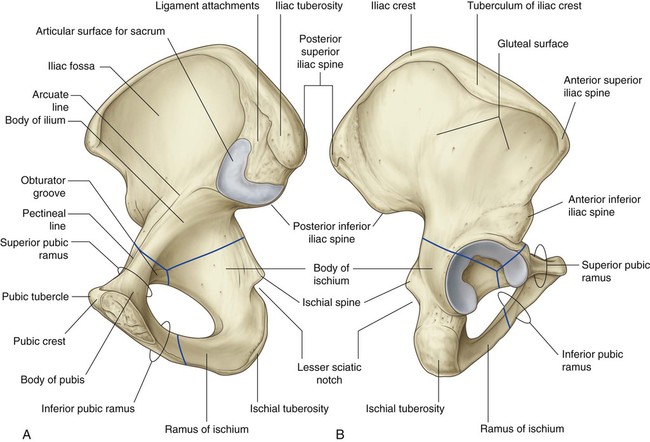
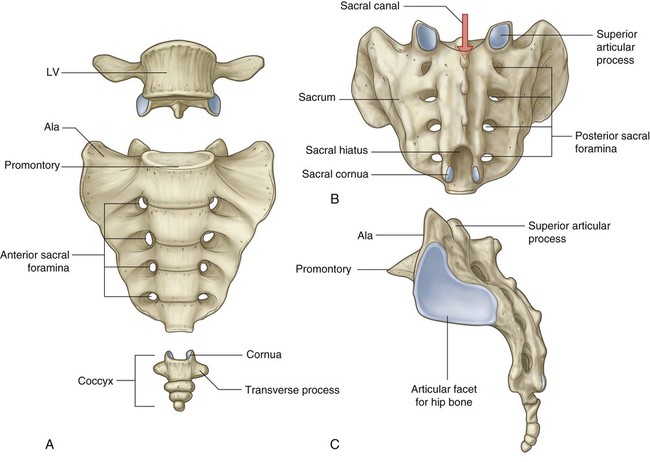
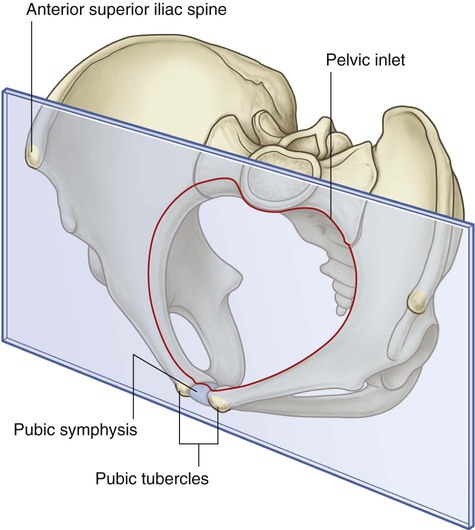
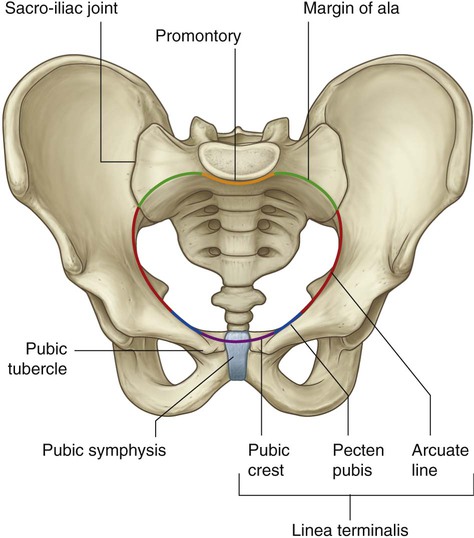
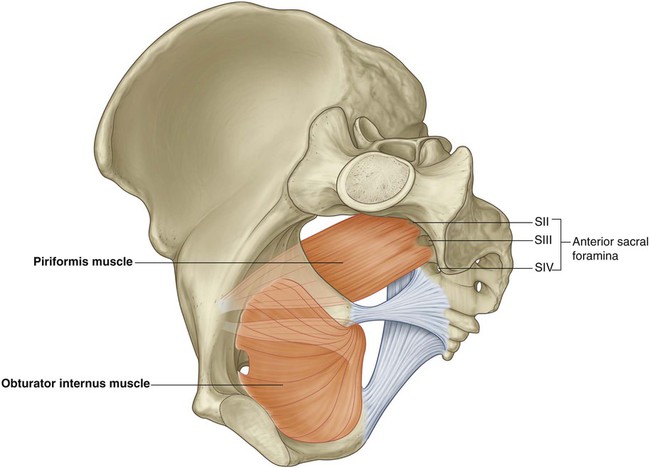
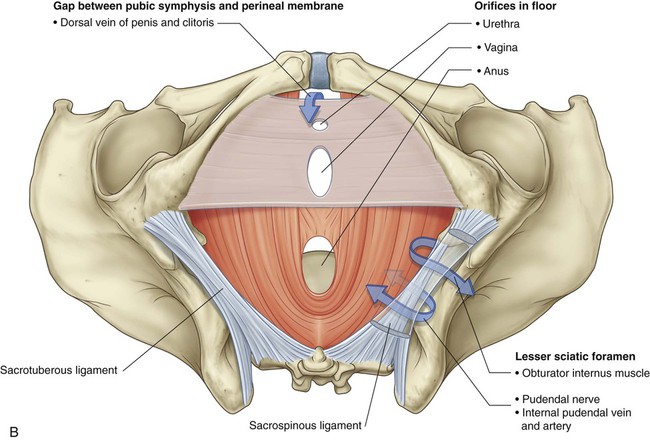
5 ADDITIONAL LEARNING RESOURCES for Chapter 5, Pelvis and Perineum, on STUDENT CONSULT (www.studentconsult.com): The perineum (Fig. 5.1) is inferior to the floor of the pelvic cavity; its boundaries form the pelvic outlet. The perineum contains the external genitalia and external openings of the genitourinary and gastrointestinal systems. As it fills, the bladder expands superiorly into the abdomen. It is supported by adjacent elements of the pelvic bone and by the pelvic floor. The urethra passes through the pelvic floor to the perineum, where, in women, it opens externally (Fig. 5.2A) and in men it enters the base of the penis (Fig. 5.2B). The pelvic inlet is somewhat heart shaped and completely ringed by bone (Fig. 5.4). Posteriorly, the inlet is bordered by the body of vertebra SI, which projects into the inlet as the sacral promontory. On each side of this vertebra, wing-like transverse processes called the alae (wings) contribute to the margin of the pelvic inlet. Laterally, a prominent rim on the pelvic bone continues the boundary of the inlet forward to the pubic symphysis, where the two pelvic bones are joined in the midline. Structures pass between the pelvic cavity and the abdomen through the pelvic inlet. Two ligaments—the sacrospinous and the sacrotuberous ligaments—are important architectural elements of the walls because they link each pelvic bone to the sacrum and coccyx (Fig. 5.5A). These ligaments also convert two notches on the pelvic bones—the greater and lesser sciatic notches—into foramina on the lateral pelvic walls. Completing the walls are the obturator internus and piriformis muscles (Fig. 5.5B), which arise in the pelvis and exit through the sciatic foramina to act on the hip joint. The pelvic floor, which separates the pelvic cavity from the perineum, is formed by muscles and fascia (Fig. 5.7). The pelvic floor is supported anteriorly by: The perineal membrane is a thick, triangular fascial sheet that fills the space between the arms of the pubic arch, and has a free posterior border (Fig. 5.7). The deep perineal pouch is a narrow region superior to the perineal membrane. The pelvic cavity is lined by peritoneum continuous with the peritoneum of the abdominal cavity that drapes over the superior aspects of the pelvic viscera, but in most regions, does not reach the pelvic floor (Fig. 5.8A). The pelvic viscera are located in the midline of the pelvic cavity. The bladder is anterior and the rectum is posterior. In women, the uterus lies between the bladder and rectum (Fig. 5.8B). Other structures, such as vessels and nerves, lie deep to the peritoneum in association with the pelvic walls and on either side of the pelvic viscera. The perineum lies inferior to the pelvic floor between the lower limbs (Fig. 5.9). Its margin is formed by the pelvic outlet. An imaginary line between the ischial tuberosities divides the perineum into two triangular regions. The cavity of the true pelvis is continuous with the abdominal cavity at the pelvic inlet (Fig. 5.10A). All structures passing between the pelvic cavity and abdomen, including major vessels, nerves, and lymphatics, as well as the sigmoid colon and ureters, pass via the inlet. In men, the ductus deferens on each side passes through the anterior abdominal wall and over the inlet to enter the pelvic cavity. In women, ovarian vessels, nerves, and lymphatics pass through the inlet to reach the ovaries, which lie on each side just inferior to the pelvic inlet. Three apertures in the pelvic wall communicate with the lower limb (Fig. 5.10A): The lesser sciatic foramen, which lies inferior to the pelvic floor, provides communication between the gluteal region and the perineum (Fig. 5.10B). The pelvic cavity also communicates directly with the perineum through a small gap between the pubic symphysis and the perineal membrane (Fig. 5.10B). In the anatomical position, the anterior superior iliac spines and the superior edge of the pubic symphysis lie in the same vertical plane (Fig. 5.11). Consequently, the pelvic inlet is angled 50°–60° forward relative to the horizontal plane, and the pelvic cavity projects posteriorly from the abdominal cavity. An important structure crosses the ureters in the pelvic cavity in both men and women—in women, the uterine artery crosses the ureter lateral to the cervix of the uterus (Fig. 5.12A), and in men, the ductus deferens crosses over the ureter just posterior to the bladder (Fig. 5.12B). Dermatomes of the perineum in both men and women are from spinal cord levels S3 to S5, except for the anterior regions, which tend to be innervated by spinal cord level L1 by nerves associated with the abdominal wall (Fig. 5.14). Dermatomes of L2 to S2 are predominantly in the lower limb. The pudendal nerve is the major nerve of the perineum and is directly associated with the ischial spine of the pelvis (Fig. 5.15). On each side of the body, these spines and the attached sacrospinous ligaments separate the greater sciatic foramina from the lesser sciatic foramina on the lateral pelvic wall. The pudendal nerve leaves the pelvic cavity through the greater sciatic foramen and then immediately enters the perineum inferiorly to the pelvic floor by passing around the ischial spine and through the lesser sciatic foramen (Fig. 5.15). The ischial spine can be palpated transvaginally in women and is the landmark for administering a pudendal nerve block. The parasympathetic innervation from spinal cord levels S2 to S4 controls genital erection in both women and men (Fig. 5.16). On each side, preganglionic parasympathetic nerves leave the anterior rami of the sacral spinal nerves and enter the inferior hypogastric plexus (pelvic plexus) on the lateral pelvic wall. Structures of the pelvic floor intersect with structures in the perineum at the perineal body (Fig. 5.17). This poorly defined fibromuscular node lies at the center of the perineum, approximately midway between the two ischial tuberosities. Converging at the perineal body are: In women, the urethra is short and passes inferiorly from the bladder through the pelvic floor and opens directly into the perineum (Fig. 5.18A). In men the urethra passes through the prostate before coursing through the deep perineal pouch and perineal membrane and then becomes enclosed within the erectile tissues of the penis before opening at the end of the penis (Fig. 5.18B). The penile part of the male urethra has two angles: The pelvic bone is irregular in shape and has two major parts separated by an oblique line on the medial surface of the bone (Fig. 5.19A): The lateral surface of the pelvic bone has a large articular socket, the acetabulum, which, together with the head of the femur, forms the hip joint (Fig. 5.19B). The posterior margin of the bone is marked by two notches separated by the ischial spine: The posterior margin terminates inferiorly as the large ischial tuberosity. Each pelvic bone is formed by three elements: the ilium, pubis, and ischium. At birth, these bones are connected by cartilage in the area of the acetabulum; later, at between 16 and 18 years of age, they fuse into a single bone (Fig. 5.20). Of the three components of the pelvic bone, the ilium is the most superior in position. The ilium is separated into upper and lower parts by a ridge on the medial surface (Fig. 5.21A). The arcuate line forms part of the linea terminalis and the pelvic brim. The upper part of the ilium expands to form a flat, fan-shaped “wing,” which provides bony support for the lower abdomen, or false pelvis. This part of the ilium provides attachment for muscles functionally associated with the lower limb. The anteromedial surface of the wing is concave and forms the iliac fossa. The external (gluteal) surface of the wing is marked by lines and roughenings and is related to the gluteal region of the lower limb (Fig. 5.21B). The anterior and inferior part of the pelvic bone is the pubis (Fig. 5.21). It has a body and two arms (rami). The sacrum, which has the appearance of an inverted triangle, is formed by the fusion of the five sacral vertebrae (Fig. 5.22). The base of the sacrum articulates with vertebra LV, and its apex articulates with the coccyx. Each of the lateral surfaces of the bone bears a large L-shaped facet for articulation with the ilium of the pelvic bone. Posterior to the facet is a large roughened area for the attachment of ligaments that support the sacro-iliac joint. The superior surface of the sacrum is characterized by the superior aspect of the body of vertebra SI and is flanked on each side by an expanded wing-like transverse process termed the ala. The anterior edge of the vertebral body projects forward as the promontory. The anterior surface of the sacrum is concave; the posterior surface is convex. Because the transverse processes of adjacent sacral vertebrae fuse lateral to the position of the intervertebral foramina and lateral to the bifurcation of spinal nerves into posterior and anterior rami, the posterior and anterior rami of spinal nerves S1 to S4 emerge from the sacrum through separate foramina. There are four pairs of anterior sacral foramina on the anterior surface of the sacrum for anterior rami, and four pairs of posterior sacral foramina on the posterior surface for the posterior rami. The sacral canal is a continuation of the vertebral canal that terminates as the sacral hiatus. The small terminal part of the vertebral column is the coccyx, which consists of four fused coccygeal vertebrae (Fig. 5.22) and, like the sacrum, has the shape of an inverted triangle. The base of the coccyx is directed superiorly. The superior surface bears a facet for articulation with the sacrum and two horns, or cornua, one on each side, that project upward to articulate or fuse with similar downward-projecting cornua from the sacrum. These processes are modified superior and inferior articular processes that are present on other vertebrae. Each lateral surface of the coccyx has a small rudimentary transverse process, extending from the first coccygeal vertebra. Vertebral arches are absent from coccygeal vertebrae; therefore no bony vertebral canal is present in the coccyx. The lumbosacral joints are reinforced by strong iliolumbar and lumbosacral ligaments that extend from the expanded transverse processes of vertebra LV to the ilium and the sacrum, respectively (Fig. 5.23B). The sacro-iliac joints transmit forces from the lower limbs to the vertebral column. They are synovial joints between the L-shaped articular facets on the lateral surfaces of the sacrum and similar facets on the iliac parts of the pelvic bones (Fig. 5.24A). The joint surfaces have an irregular contour and interlock to resist movement. The joints often become fibrous with age and may become completely ossified. Each sacro-iliac joint is stabilized by three ligaments: The pubic symphysis lies anteriorly between the adjacent surfaces of the pubic bones (Fig. 5.25). Each of the joint’s surfaces is covered by hyaline cartilage and is linked across the midline to adjacent surfaces by fibrocartilage. The joint is surrounded by interwoven layers of collagen fibers and the two major ligaments associated with it are: In the anatomical position, the pelvis is oriented so that the front edge of the top of the pubic symphysis and the anterior superior iliac spines lie in the same vertical plane (Fig. 5.26). As a consequence, the pelvic inlet, which marks the entrance to the pelvic cavity, is tilted to face anteriorly, and the bodies of the pubic bones and the pubic arch are positioned in a nearly horizontal plane facing the ground. The pelvic inlet is the circular opening between the abdominal cavity and the pelvic cavity through which structures traverse between the abdomen and pelvic cavity. It is completely surrounded by bones and joints (Fig. 5.28). The promontory of the sacrum protrudes into the inlet, forming its posterior margin in the midline. On either side of the promontory, the margin is formed by the alae of the sacrum. The margin of the pelvic inlet then crosses the sacro-iliac joint and continues along the linea terminalis (i.e., the arcuate line, the pecten pubis or pectineal line, and the pubic crest) to the pubic symphysis. The sacrospinous and sacrotuberous ligaments (Fig. 5.29A) are major components of the lateral pelvic walls that help define the apertures between the pelvic cavity and adjacent regions through which structures pass. These ligaments stabilize the sacrum on the pelvic bones by resisting the upward tilting of the inferior aspect of the sacrum (Fig. 5.29B). They also convert the greater and lesser sciatic notches of the pelvic bone into foramina (Fig. 5.29A,B). The obturator internus is a flat, fan-shaped muscle that originates from the deep surface of the obturator membrane and from associated regions of the pelvic bone that surround the obturator foramen (Fig. 5.30 and Table 5.1). Table 5.1 The obturator internus forms a large part of the anterolateral wall of the pelvic cavity. The piriformis is triangular and originates in the bridges of bone between the four anterior sacral foramina. It passes laterally through the greater sciatic foramen, crosses the posterosuperior aspect of the hip joint, and inserts on the greater trochanter of the femur above the insertion of the obturator internus muscle (Fig. 5.30 and Table 5.1).
Pelvis and Perineum
Conceptual overview
General description
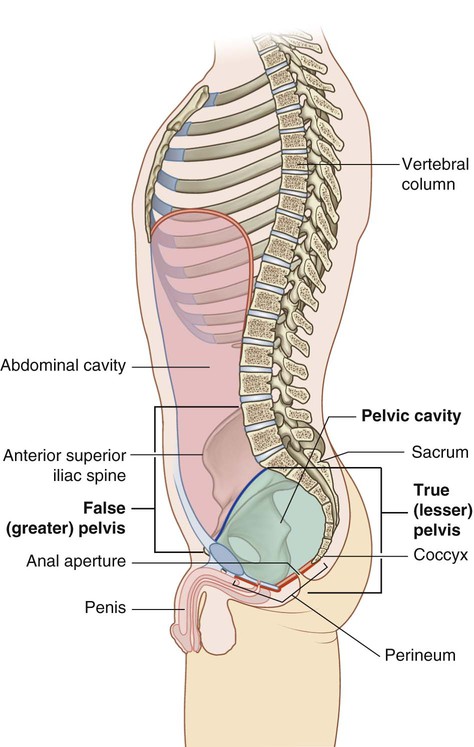
 The superior region related to upper parts of the pelvic bones and lower lumbar vertebrae is the false pelvis (greater pelvis) and is generally considered part of the abdomen (Fig. 5.1).
The superior region related to upper parts of the pelvic bones and lower lumbar vertebrae is the false pelvis (greater pelvis) and is generally considered part of the abdomen (Fig. 5.1).
 The true pelvis (lesser pelvis) is related to the inferior parts of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet.
The true pelvis (lesser pelvis) is related to the inferior parts of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet.
Functions
Contains and supports the bladder, rectum, anal canal, and reproductive tracts
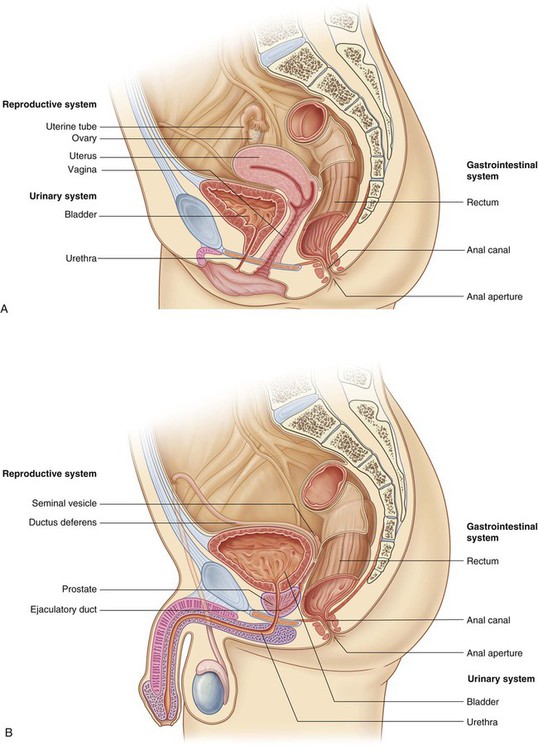
 In women, the vagina penetrates the pelvic floor and connects with the uterus in the pelvic cavity. The uterus is positioned between the rectum and the bladder. A uterine (fallopian) tube extends laterally on each side toward the pelvic wall to open near the ovary.
In women, the vagina penetrates the pelvic floor and connects with the uterus in the pelvic cavity. The uterus is positioned between the rectum and the bladder. A uterine (fallopian) tube extends laterally on each side toward the pelvic wall to open near the ovary.
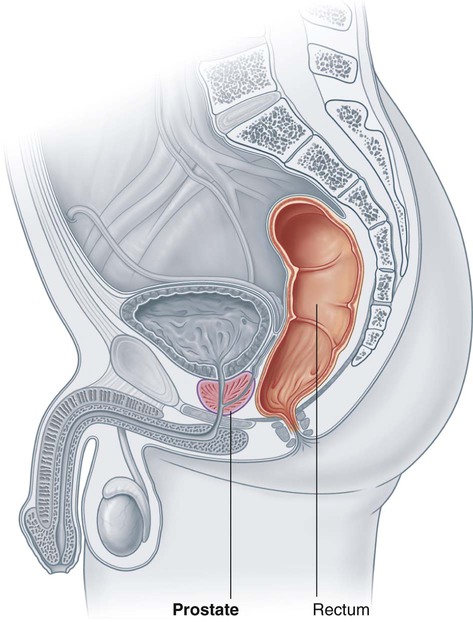
 In men, the pelvic cavity contains the site of connection between the urinary and reproductive tracts. It also contains major glands associated with the reproductive system—the prostate and two seminal vesicles.
In men, the pelvic cavity contains the site of connection between the urinary and reproductive tracts. It also contains major glands associated with the reproductive system—the prostate and two seminal vesicles.
Component parts
Pelvic inlet
Pelvic walls
Pelvic floor
Pelvic cavity
Perineum
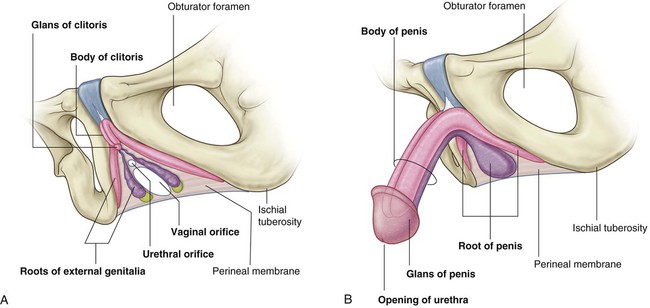
 Anteriorly, the urogenital triangle contains the roots of the external genitalia and, in women, the openings of the urethra and the vagina (Fig. 5.9A). In men, the distal part of the urethra is enclosed by erectile tissues and opens at the end of the penis (Fig. 5.9B).
Anteriorly, the urogenital triangle contains the roots of the external genitalia and, in women, the openings of the urethra and the vagina (Fig. 5.9A). In men, the distal part of the urethra is enclosed by erectile tissues and opens at the end of the penis (Fig. 5.9B).
Relationship to other regions
Abdomen
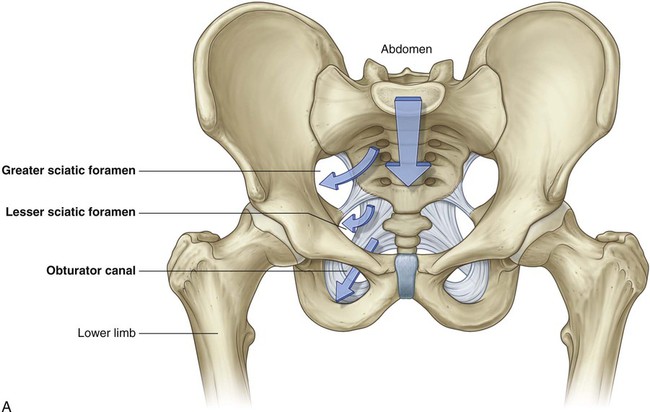
Lower limb
Key features
The pelvic cavity projects posteriorly
Important structures cross the ureters in the pelvic cavity
The perineum is innervated by sacral spinal cord segments
Nerves are related to bone
Parasympathetic innervation from spinal cord levels S2 to S4 controls erection
Muscles and fascia of the pelvic floor and perineum intersect at the perineal body
The course of the urethra is different in men and women
 The more important of these is a fixed angle where the urethra bends anteriorly in the root of the penis after passing through the perineal membrane.
The more important of these is a fixed angle where the urethra bends anteriorly in the root of the penis after passing through the perineal membrane.
 Another angle occurs distally where the unattached part of the penis curves inferiorly—when the penis is erect, this second angle disappears.
Another angle occurs distally where the unattached part of the penis curves inferiorly—when the penis is erect, this second angle disappears.
Regional anatomy
 the terminal openings of the gastrointestinal and urinary systems,
the terminal openings of the gastrointestinal and urinary systems,
 the external opening of the reproductive tract, and
the external opening of the reproductive tract, and
Pelvis
Bones
Pelvic bone
 The pelvic bone above this line represents the lateral wall of the false pelvis, which is part of the abdominal cavity.
The pelvic bone above this line represents the lateral wall of the false pelvis, which is part of the abdominal cavity.
 The pelvic bone below this line represents the lateral wall of the true pelvis, which contains the pelvic cavity.
The pelvic bone below this line represents the lateral wall of the true pelvis, which contains the pelvic cavity.
Components of the pelvic bone
 Posteriorly, the ridge is sharp and lies immediately superior to the surface of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened area for the attachment of the strong ligaments that support the sacro-iliac joint (Fig. 5.21).
Posteriorly, the ridge is sharp and lies immediately superior to the surface of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened area for the attachment of the strong ligaments that support the sacro-iliac joint (Fig. 5.21).
 Anteriorly, the ridge separating the upper and lower parts of the ilium is rounded and termed the arcuate line.
Anteriorly, the ridge separating the upper and lower parts of the ilium is rounded and termed the arcuate line.
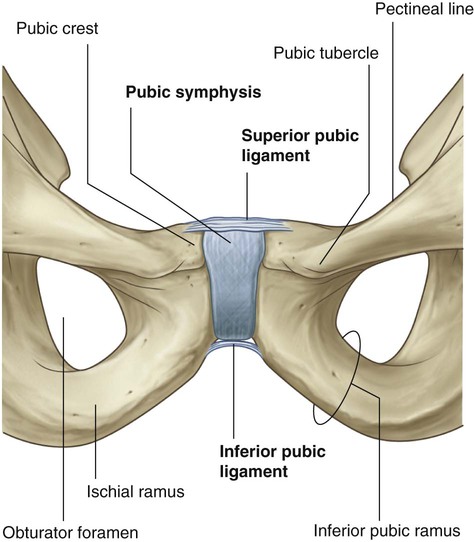
 The body is flattened dorsoventrally and articulates with the body of the pubic bone on the other side at the pubic symphysis. The body has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle.
The body is flattened dorsoventrally and articulates with the body of the pubic bone on the other side at the pubic symphysis. The body has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle.
 The superior pubic ramus projects posterolaterally from the body and joins with the ilium and ischium at its base, which is positioned toward the acetabulum. The sharp superior margin of this triangular surface is termed the pecten pubis (pectineal line), which forms part of the linea terminalis of the pelvic bone and the pelvic inlet. Anteriorly, this line is continuous with the pubic crest, which also is part of the linea terminalis and pelvic inlet. The superior pubic ramus is marked on its inferior surface by the obturator groove, which forms the upper margin of the obturator canal.
The superior pubic ramus projects posterolaterally from the body and joins with the ilium and ischium at its base, which is positioned toward the acetabulum. The sharp superior margin of this triangular surface is termed the pecten pubis (pectineal line), which forms part of the linea terminalis of the pelvic bone and the pelvic inlet. Anteriorly, this line is continuous with the pubic crest, which also is part of the linea terminalis and pelvic inlet. The superior pubic ramus is marked on its inferior surface by the obturator groove, which forms the upper margin of the obturator canal.
 The inferior ramus projects laterally and inferiorly to join with the ramus of the ischium.
The inferior ramus projects laterally and inferiorly to join with the ramus of the ischium.
Sacrum
Coccyx
Joints
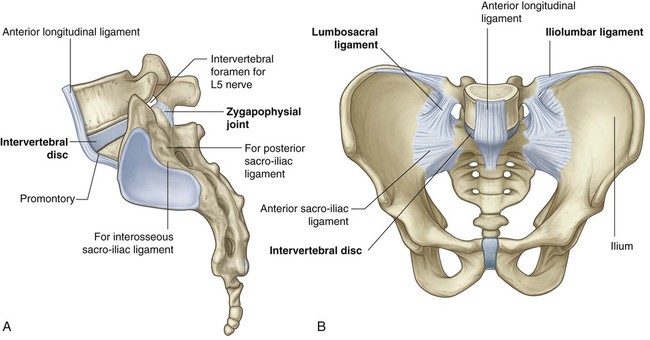
Lumbosacral joints
 the two zygapophysial joints, which occur between adjacent inferior and superior articular processes, and
the two zygapophysial joints, which occur between adjacent inferior and superior articular processes, and
 an intervertebral disc that joins the bodies of vertebrae LV and SI (Fig. 5.23A).
an intervertebral disc that joins the bodies of vertebrae LV and SI (Fig. 5.23A).
Sacro-iliac joints
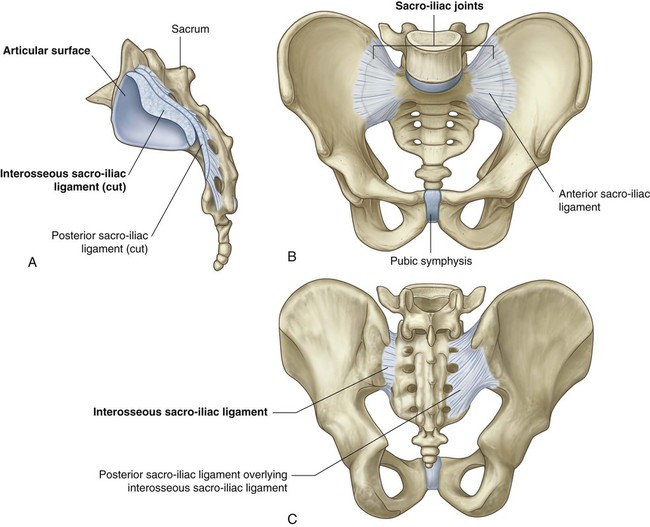
 the anterior sacro-iliac ligament, which is a thickening of the fibrous membrane of the joint capsule and runs anteriorly and inferiorly to the joint (Fig. 5.24B);
the anterior sacro-iliac ligament, which is a thickening of the fibrous membrane of the joint capsule and runs anteriorly and inferiorly to the joint (Fig. 5.24B);
 the interosseous sacro-iliac ligament, which is the largest, strongest ligament of the three, and is positioned immediately posterosuperior to the joint and attaches to adjacent expansive roughened areas on the ilium and sacrum, thereby filling the gap between the two bones (Fig. 5.24A,C); and
the interosseous sacro-iliac ligament, which is the largest, strongest ligament of the three, and is positioned immediately posterosuperior to the joint and attaches to adjacent expansive roughened areas on the ilium and sacrum, thereby filling the gap between the two bones (Fig. 5.24A,C); and
 the posterior sacro-iliac ligament, which covers the interosseous sacro-iliac ligament (Fig. 5.24C).
the posterior sacro-iliac ligament, which covers the interosseous sacro-iliac ligament (Fig. 5.24C).
Pubic symphysis joint
Orientation
Differences between men and women
 The pelvic inlet in women is circular (Fig. 5.27A) compared with the heart-shaped pelvic inlet (Fig. 5.27B) in men. The more circular shape is partly caused by the less distinct promontory and broader alae in women.
The pelvic inlet in women is circular (Fig. 5.27A) compared with the heart-shaped pelvic inlet (Fig. 5.27B) in men. The more circular shape is partly caused by the less distinct promontory and broader alae in women.
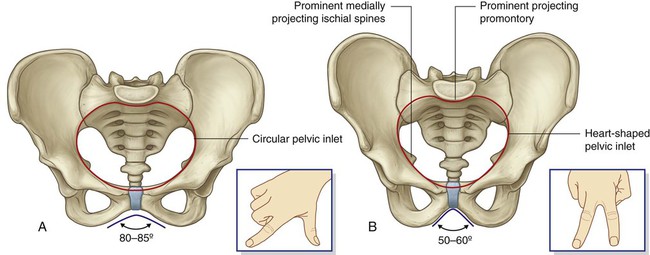
 The angle formed by the two arms of the pubic arch is larger in women (80°–85°) than it is in men (50°–60°).
The angle formed by the two arms of the pubic arch is larger in women (80°–85°) than it is in men (50°–60°).
 The ischial spines generally do not project as far medially into the pelvic cavity in women as they do in men.
The ischial spines generally do not project as far medially into the pelvic cavity in women as they do in men.
True pelvis
Pelvic inlet
Pelvic wall
Ligaments of the pelvic wall
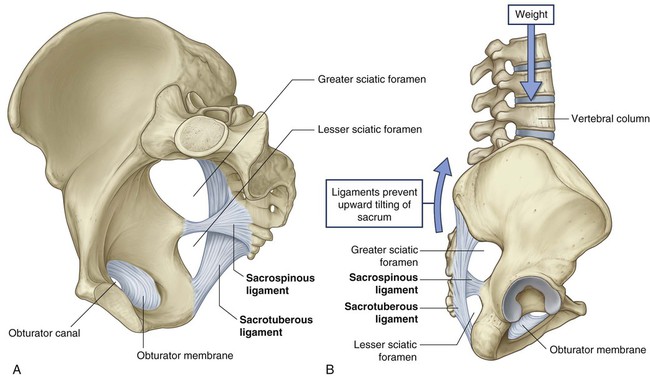
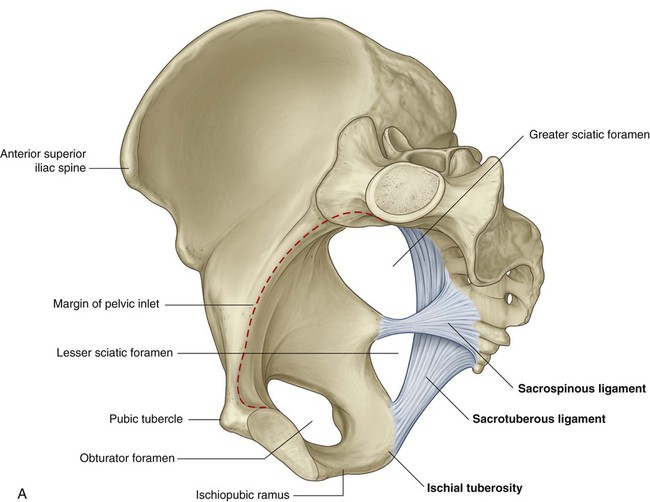
 The smaller of the two, the sacrospinous ligament, is triangular, with its apex attached to the ischial spine and its base attached to the related margins of the sacrum and the coccyx.
The smaller of the two, the sacrospinous ligament, is triangular, with its apex attached to the ischial spine and its base attached to the related margins of the sacrum and the coccyx.
 The sacrotuberous ligament is also triangular and is superficial to the sacrospinous ligament. Its base has a broad attachment that extends from the posterior superior iliac spine of the pelvic bone, along the dorsal aspect and the lateral margin of the sacrum, and onto the dorsolateral surface of the coccyx. Laterally, the apex of the ligament is attached to the medial margin of the ischial tuberosity.
The sacrotuberous ligament is also triangular and is superficial to the sacrospinous ligament. Its base has a broad attachment that extends from the posterior superior iliac spine of the pelvic bone, along the dorsal aspect and the lateral margin of the sacrum, and onto the dorsolateral surface of the coccyx. Laterally, the apex of the ligament is attached to the medial margin of the ischial tuberosity.
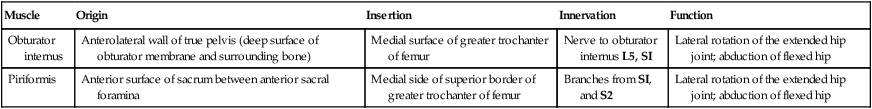
Muscles of the pelvic wall
Muscle
Origin
Insertion
Innervation
Function
Obturator internus
Anterolateral wall of true pelvis (deep surface of obturator membrane and surrounding bone)
Medial surface of greater trochanter of femur
Nerve to obturator internus L5, SI
Lateral rotation of the extended hip joint; abduction of flexed hip
Piriformis
Anterior surface of sacrum between anterior sacral foramina
Medial side of superior border of greater trochanter of femur
Branches from SI, and S2
Lateral rotation of the extended hip joint; abduction of flexed hip
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree