• The thorax lies between the neck and the abdomen and lies within a cage formed by the vertebrae, the ribs, the sternum, the costal cartilages, and their attached muscles. The thoracic cage protects the contents of the thorax, whereas the muscles assist in breathing. • It is important to identify and count ribs because they form key landmarks to the positions of the internal organs. • In a fit, muscular person one can identify a number of landmarks • Jugular (suprasternal) notch: at level of inferior border of T2 vertebra • Sternal angle (manubriosternal join): at level of T4/5 intervertebral disc and where second costal cartilages articulate with sternum • Manubrium: left brachiocephalic vein runs beneath manubrium from upper left to lower right, where it joins right brachiocephalic vein to form superior vena cava. • Body of sternum: anterior to T5 through T9 vertebrae and right border of heart • Nipple: anterior to 4th intercostal space in males and dome of right hemidiaphragm; sits on pectoralis major muscle • Xiphoid process: at level of T10 vertebra • The costal margins: comprises 7th through 10th costal cartilages • On yourself, palpate the following: • The sternoclavicular joints, lateral to jugular notch • The sternum and its parts: manubrium, body, and xiphoid process • The manubriosternal joint (sternal angle) • The second pair of ribs on either side of sternal angle—the surface landmark for rib counting • Surface lines can be drawn to identify regions of the thorax. • Imaginary perpendicular lines passing through midpoint of each clavicle are called midclavicular lines. • Midaxillary lines are perpendicular lines through apex of axilla on both sides. • Cephalic vein can be seen in some subjects; it lies in deltopectoral groove between deltoid and pectoralis major muscles. • The sternum can be divided to gain access to the thoracic cavity for surgical operations. This is called a median sternotomy. • The middle ribs are most commonly fractured, and multiple rib fractures can manifest as a “flail chest,” where the injured region of the chest wall moves paradoxically, that is, in on inspiration and out on expiration. • Consists of glandular tissue in which the majority is embedded within the tela subcutanea (superficial fascia) of the anterior chest wall overlying the pectoral muscles • The glands are rudimentary in males and immature females. • Size and shape of the adult female breast varies; size is determined by amount of fat surrounding glandular tissue. • The base of the breast is fairly consistent, extending from lateral border of sternum to midaxillary line and from 2nd to 6th ribs. • The majority of the breast overlies deep pectoral fascia of pectoralis major muscle, with remainder overlying fascia of serratus anterior. • The breast is separated from pectoralis major muscle by retromammary space, a potential space filled with loose connective tissue. • The breast is firmly attached to overlying skin by condensation of connective tissue called suspensory ligaments (of Cooper), which help to support lobules of the breast. • A small part of the mammary gland may extend toward the axilla, called the axillary tail (of Spence). • For descriptive purposes, the breast is divided into four quadrants: upper and lower lateral, and upper and lower medial. • The most prominent feature of the breast is the nipple. • The nipple is surrounded by the areola, a circular pigmented area of skin. • The areola is pink in Caucasians and brown in African and Asian people. • The pigmentation of the areola increases during pregnancy. • The areola contains sebaceous glands; following a pregnancy these secrete an oily substance to protect the mother’s nipple from irritation during nursing. • The breast is composed of 15 to 20 lobules of glandular tissue, formed by septa of suspensory ligaments. • The mammary glands are modified sweat glands that are formed from development of milk-secreting alveoli, arranged in clusters. • Each lobule is drained by a lactiferous duct. • Blood supply of the breast arises from the perforating branches and anterior intercostal branches of the internal thoracic artery. • The breast is also supplied by the branches of the thoraco-acromial and lateral thoracic arteries (from the axillary artery). • Venous drainage parallels the arterial supply and is mainly to the axillary artery and internal thoracic vein. • Lymph from the nipple, areola, and lobules of the mammary glands drains to a subareolar lymphatic plexus. • From there, a system of interconnecting lymphatic channels drains lymph to various lymph nodes. • The majority of the lymph, especially from the lateral quadrants of the breast, drains to the pectoral nodes, and from there to the axillary nodes. • The remaining amount of lymph, especially from the medial quadrants of the breast, drains into the parasternal lymph nodes along the internal thoracic vessels. • Some lymph from the lower quadrants of the breast passes to the inferior phrenic nodes. • Lymph from the medial quadrants can cross to the opposite breast. • Secondary metastases of breast carcinoma can spread to the opposite breast in this way. Clinically the breast is divided into quadrants: The breast is palpated in a circular fashion, beginning with the nipple and moving outward. The palpation should extend into the axilla to palpate the axillary tails. After palpation of one breast, the other should be palpated in the same way. Examine the skin of the breast for a change in texture or dimpling (peau d’orange sign) and the nipple for retraction, since these signs may indicate underlying disease. • Fibroadenoma: benign tumor, usually a solid and solitary mass that moves easily under the skin. Often painless, although sometimes tender on palpation. More common in young women but can occur at any age. • Intraductal carcinoma, or breast cancer: the commonest type of malignancy in women but can also occur in men. Approximately 50% of cancers develop in the upper quadrant of the breast; metastases from these cancers often spread to the axillary lymph nodes. This malignancy presents as a palpable mass that is hard, immobile, and sometimes painful. Additional signs can include bloody or watery nipple discharge if the larger ducts are involved. • Gynecomastia: enlargement of the breasts in males because of aging, drug treatment, and changes in the metabolism of sex hormones by the liver. These muscles are arranged in three layers • External intercostal muscles • Have fibers that slope down and medially • Extend from posterior tubercle of rib to junction of rib and its costal cartilage anteriorly • Anteriorly, are replaced by external intercostal membranes that extend from costochondral junctions to sternum • Internal intercostal muscles: • Lie internal to external intercostal muscles • Their fibers lie at right angles to those of external intercostal muscles and run inferiorly and laterally. • Anteriorly extend to lateral border of sternum • Posteriorly extend only to angles of ribs; medial to angles, are replaced by internal intercostal membranes • Innermost intercostal muscles • Lie deep to internal intercostal muscles • Separated from internal intercostals by intercostal vessels and nerves • Connect inner surfaces of adjacent ribs • All intercostal muscles are supplied by intercostal nerves corresponding in number to their intercostal space. • Main action of intercostals is to maintain space between ribs during inspiration and expiration. • Subcostal muscles—internal to internal intercostals, cross from angle of one rib to internal surface of rib 1 to 2 spaces below • Transversus thoracis—4 to 5 slips of muscle that attach to xiphoid process and inferior sternum and pass superiorly and laterally to attach to 2nd through 6th costal cartilages • Intercostal nerves arise from the ventral rami of the upper eleven thoracic spinal nerves. • Each intercostal nerve divides to give a lateral cutaneous branch near the midaxillary line. • Anterior cutaneous branches innervate skin on anterior abdomen and thorax and divide into medial and lateral branches. • Muscular branches supply intercostal, levatores costarum, transversus thoracis, and serratus posterior muscles. • The lower five intercostal nerves supply skin and muscles of abdominal wall. • Contain general somatic afferent and efferent fibers, as well as general visceral efferent fibers from sympathetic trunk via white and gray rami communicantes and general visceral afferent fibers. • All ribs contain bone marrow. • Ribs 1 through 7 are vertebrocostal because they attach to sternum via a costal cartilage. • Ribs 8 through 10 are vertebrochondral because their cartilages are joined to cartilage of rib above and via that connection to sternum. • Ribs 11 and 12 are free or floating ribs that do not connect even indirectly with sternum but that have a costal cartilage on their tips. • First rib is broad and sharply curved and has a tubercle of attachment of scalene muscles. • Sternal angle (of Louis); level of bifurcation of trachea, arch of aorta: T4/T5 • Aortic hiatus of diaphragm; also transmits thoracic duct: T12 • Esophageal hiatus of diaphragm; also transmits right and left vagal trunks, esophageal branches of left gastric vessels, and lymphatics: T10 • Caval opening of diaphragm; also terminal branches of right phrenic nerve: T8 • Second intercostal space at the midclavicular line: insertion of tube for an apical pneumothorax (thoracostomy) • 4th to 6th intercostal space at the midaxillary line: insertion of chest drains for a hemothorax (thoracostomy) • Left 5th intercostal space: apex beat of the heart and this is shifted in heart enlargement • Bone marrow biopsy: The removal of bone and marrow for examination under the microscope. The sternum is a site of red marrow, even in adulthood, and is a good site for a bone marrow biopsy. Another common site is the posterior iliac crest. A biopsy is usually conducted before performing a bone marrow aspiration. • Bone marrow aspiration: The removal of a small amount of bone marrow fluid through a needle inserted into the bone. Fluid is examined to determine if there are any problems with the blood cells made in the bone marrow • Two lateral pleural cavities containing the lungs and pleurae • Central compartment, the mediastinum, containing all other thoracic structures • Each lung is surrounded by, and covered with, a continuous membrane, which is defined as • The visceral and parietal pleura are continuous at hilum of the lung where structures enter and leave the lung (bronchus, pulmonary vessels, bronchial vessels, lymphatics). • The parietal pleura has four named parts. • Costal pleura lining internal surface of thoracic wall • Mediastinal pleura covering sides of mediastinum • Diaphragmatic pleura covering superior surface of dome of each hemidiaphragm • Cervical pleura, dome of pleura extending superiorly into superior thoracic aperture • Visceral pleura does not have any general sensory innervation and is insensitive to pain. • The parietal pleura is very sensitive to pain because of its sensory supply by branches of intercostal and phrenic nerves. • The pleural cavity is potential space between parietal and visceral pleura. • Lines of pleural reflection are lines along which parietal pleura changes directions from one wall to another. • Sternal line of pleural reflection is sharp line along which costal pleura becomes mediastinal pleura. • Costal line of pleural reflection is sharp line along which costal pleura becomes diaphragmatic pleura. • Vertebral line of pleural reflection is a smooth reflection of costal pleura onto vertebrae posteriorly. • The lines of pleural reflection on the left side can be remembered as 4-6-8-10-12. • The line of pleural reflection on left descends in midline of sternum to 4th costal cartilage, where it deviates to left margin of sternum at 6th costal cartilage to accommodate pericardium and heart (cardiac notch). • This line then deviates to cross 8th rib at midclavicular line. • It crosses 10th rib at midaxillary line. • On the right side, line of pleural reflection descends at midline of sternum to xiphoid process, and then deviates 8-10-12. • The lungs do not fully occupy pleural cavities during expiration. • There are peripheral areas where diaphragmatic and costal pleura come in contact, referred to as the costodiaphragmatic recesses. • There are areas posterior to sternum where costal and mediastinal pleura come in contact with each other, and these are called costomediastinal recesses. • The costomediastinal recess is larger on the left because of the cardiac notch. • During expiration, the lower limit of the lungs is two costal spaces above line of pleural reflection.
Thorax Study Guide
3.1 Topographic Anatomy
Guide
Clinical Points
3.2 Mammary Gland
Guide
Structure of the Breast
Vasculature of the Breast
Lymphatic Drainage of the Breast
Clinical Points
Examination of the Breast
Pathology of the Breast
3.3 Body Wall
Guide
Layers
Intercostal Muscles
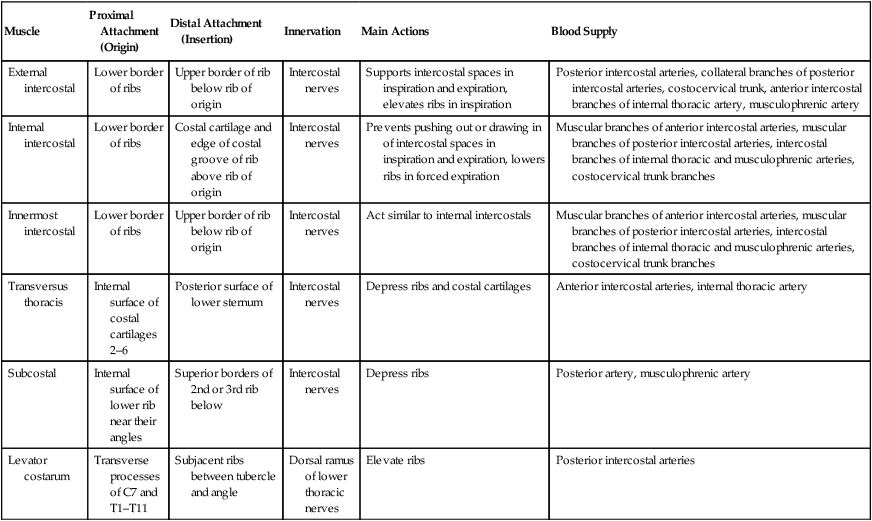
Muscle
Proximal Attachment (Origin)
Distal Attachment (Insertion)
Innervation
Main Actions
Blood Supply
External intercostal
Lower border of ribs
Upper border of rib below rib of origin
Intercostal nerves
Supports intercostal spaces in inspiration and expiration, elevates ribs in inspiration
Posterior intercostal arteries, collateral branches of posterior intercostal arteries, costocervical trunk, anterior intercostal branches of internal thoracic artery, musculophrenic artery
Internal intercostal
Lower border of ribs
Costal cartilage and edge of costal groove of rib above rib of origin
Intercostal nerves
Prevents pushing out or drawing in of intercostal spaces in inspiration and expiration, lowers ribs in forced expiration
Muscular branches of anterior intercostal arteries, muscular branches of posterior intercostal arteries, intercostal branches of internal thoracic and musculophrenic arteries, costocervical trunk branches
Innermost intercostal
Lower border of ribs
Upper border of rib below rib of origin
Intercostal nerves
Act similar to internal intercostals
Muscular branches of anterior intercostal arteries, muscular branches of posterior intercostal arteries, intercostal branches of internal thoracic and musculophrenic arteries, costocervical trunk branches
Transversus thoracis
Internal surface of costal cartilages 2–6
Posterior surface of lower sternum
Intercostal nerves
Depress ribs and costal cartilages
Anterior intercostal arteries, internal thoracic artery
Subcostal
Internal surface of lower rib near their angles
Superior borders of 2nd or 3rd rib below
Intercostal nerves
Depress ribs
Posterior artery, musculophrenic artery
Levator costarum
Transverse processes of C7 and T1–T11
Subjacent ribs between tubercle and angle
Dorsal ramus of lower thoracic nerves
Elevate ribs
Posterior intercostal arteries
Intercostal Nerves
Ribs
Anatomical and Clinical Points
Important Vertebral Landmarks
Importance of Certain Intercostal Spaces
Bone Marrow Biopsy and Aspiration
3.4 Lungs
Guides
Thoracic Cavity, Pleurae, and Pleural Cavity
Lines of Pleural Reflection



