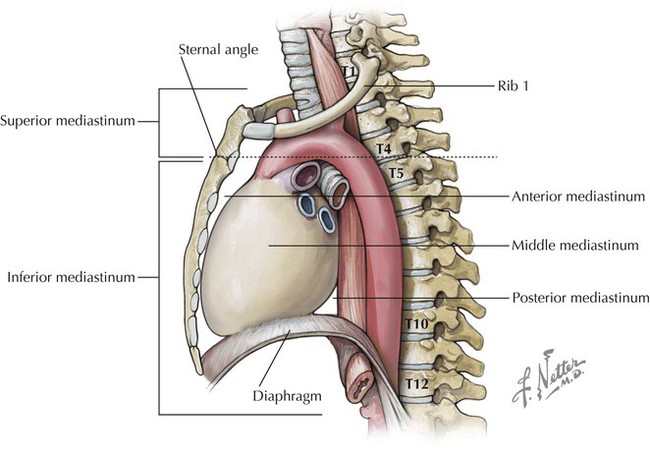
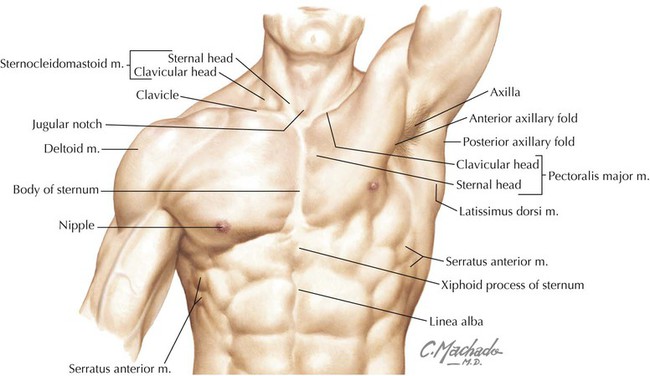
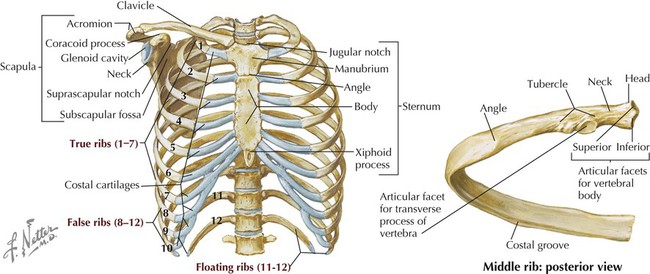
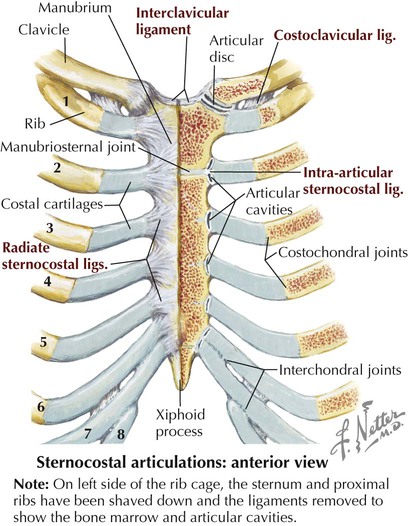
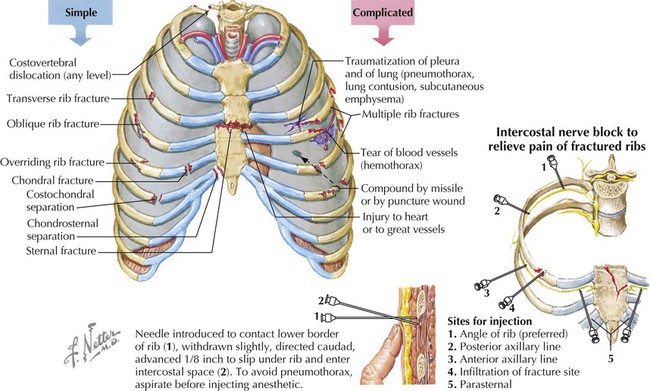
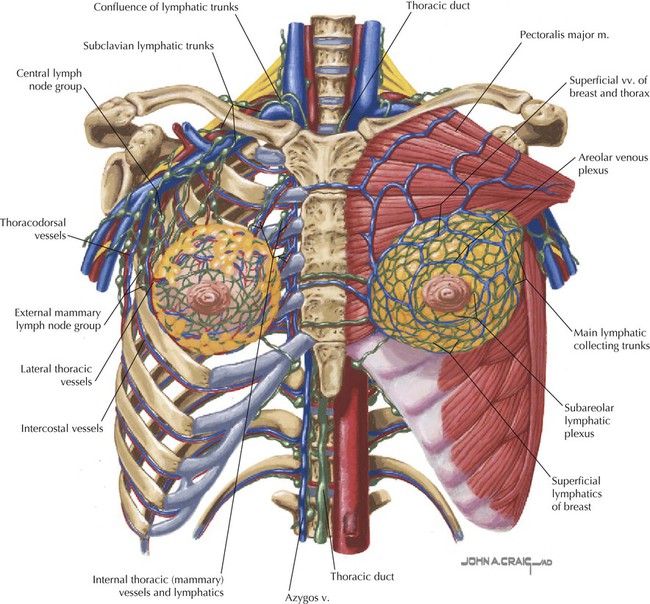
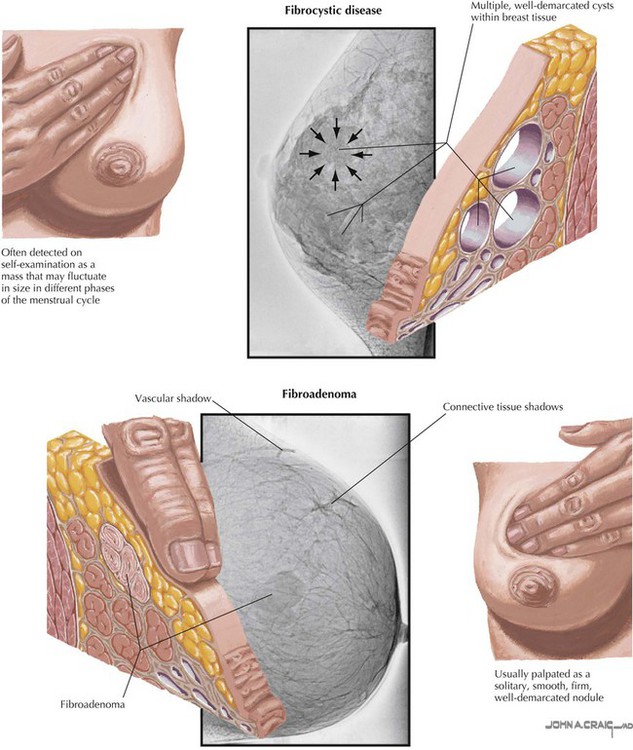
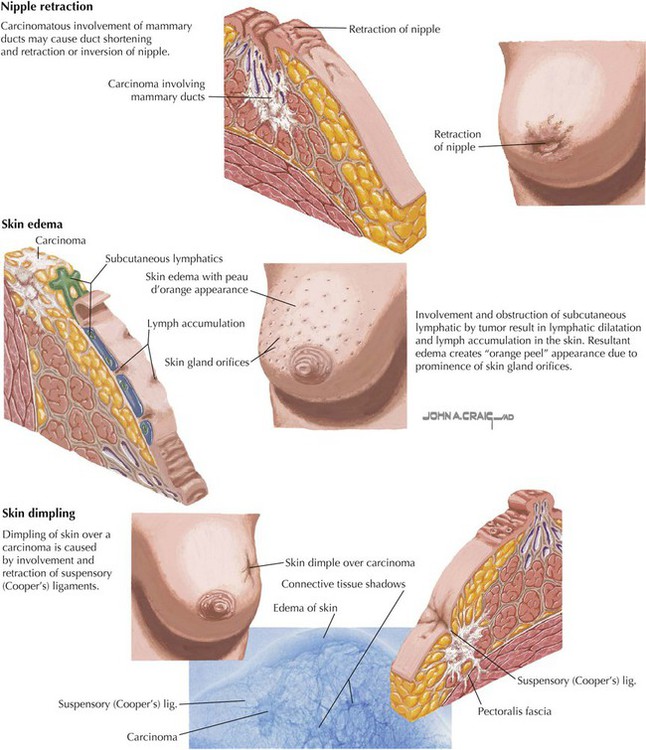
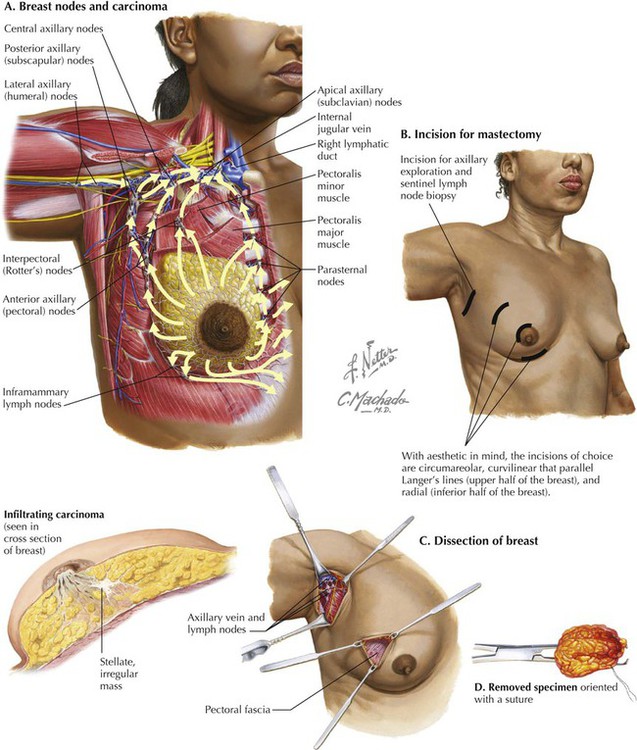
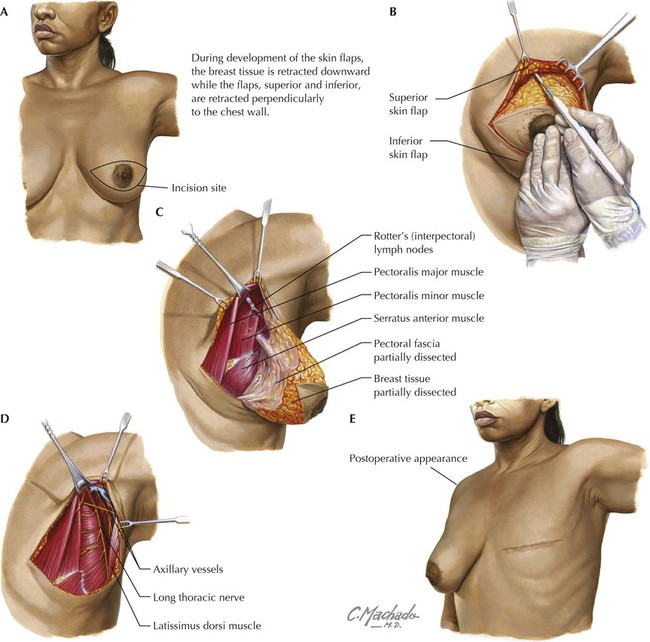
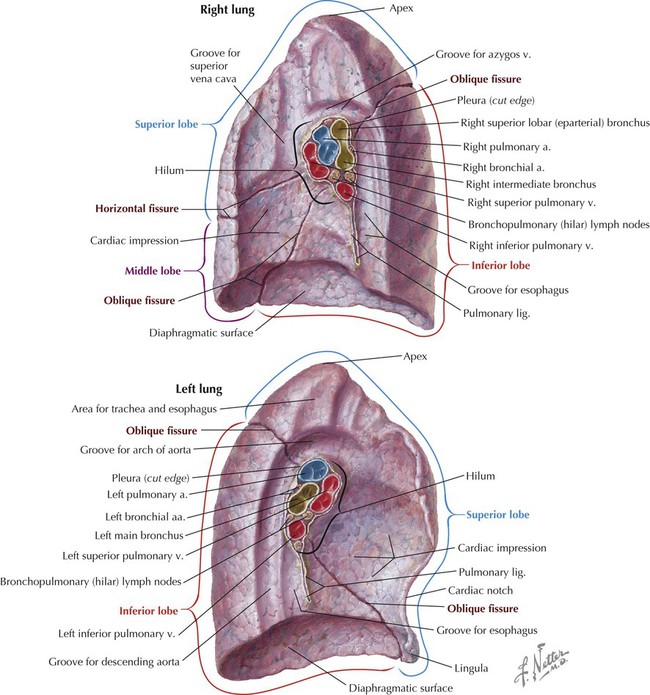
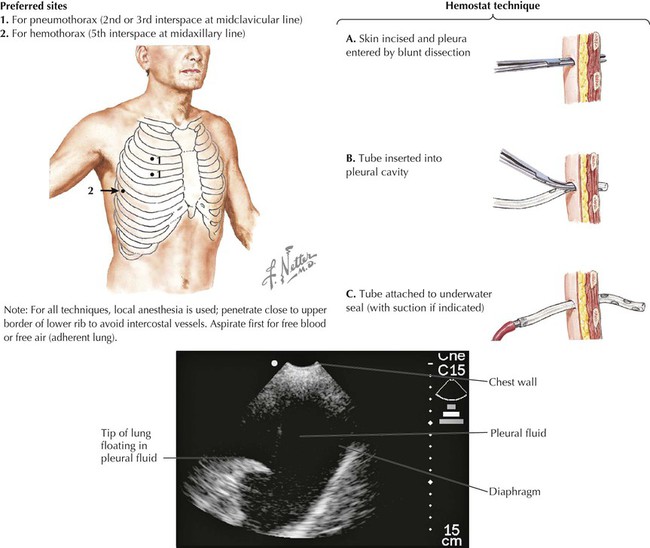
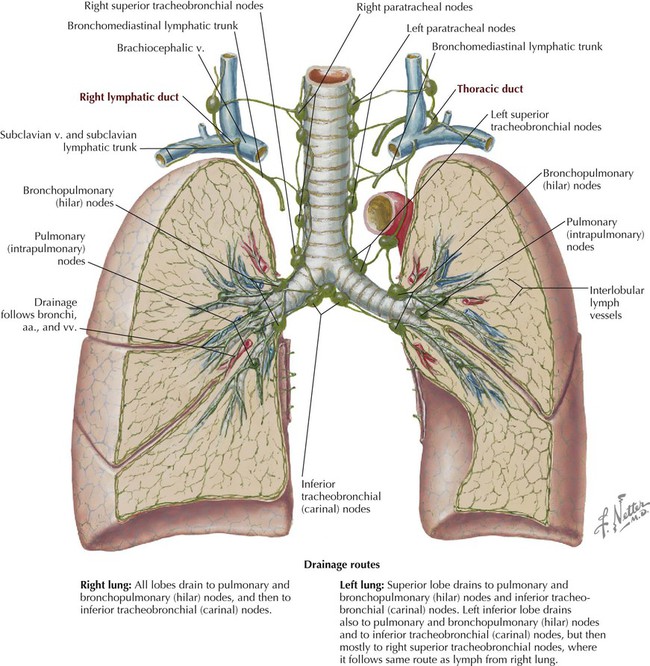
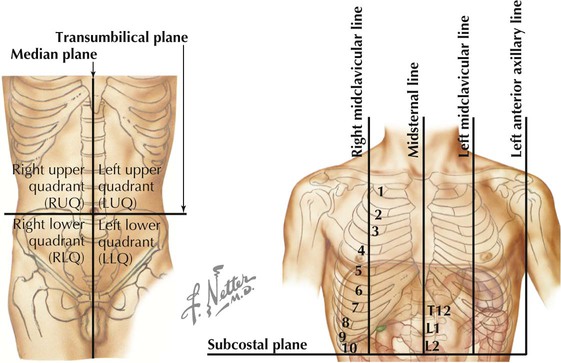
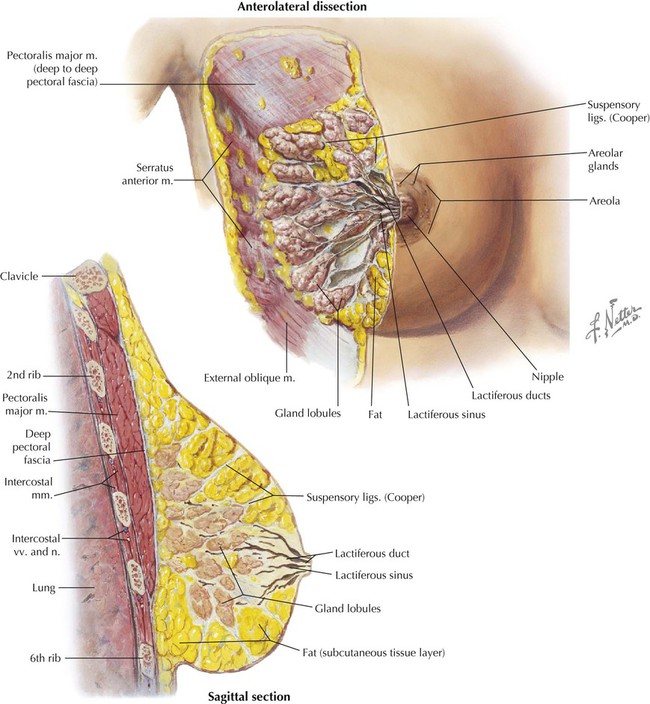
• Protection: the thoracic cage and its muscles protect the vital structures in the thorax. • Support: the thoracic cage provides muscular support for the upper limb. • Conduit: the thorax provides for a superior and an inferior thoracic aperture and a central mediastinum. • Segmentation: the thorax provides an excellent example of segmentation, a hallmark of the vertebrate body plan. • Breathing: movements of the diaphragm and intercostal muscles are essential for expanding the thoracic cavity to facilitate the entry of air into the lungs in the process of breathing. • Pumping blood: the thorax contains the heart, which pumps blood through the pulmonary and systemic circulations. The superior thoracic aperture (the anatomical thoracic inlet) conveys large vessels, important nerves, the thoracic lymphatic duct, the trachea, and the esophagus between the neck and thorax. Clinicians often refer to “thoracic outlet syndrome,” which describes symptoms associated with compression of the brachial plexus as it passes over the first rib (specifically, the T1 ventral ramus). Technically, this is a misnomer because these nerves are not exiting the superior thoracic aperture (thoracic inlet). The inferior thoracic aperture (the anatomical thoracic outlet) conveys the inferior vena cava (IVC), aorta, esophagus, nerves, and thoracic lymphatic duct between the thorax and the abdominal cavity. Additionally, the thorax contains two pleural cavities laterally and a central “middle space” called the mediastinum, which is divided as follows (Fig. 3-1): • Superior mediastinum: a midline compartment that lies above an imaginary horizontal plane that passes through the manubrium of the sternum (sternal angle of Louis) and the intervertebral disc between the T4 and T5 vertebrae • Inferior mediastinum: the midline compartment below this same horizontal plane, which is further subdivided into an anterior, middle (contains the heart), and posterior mediastinum Key surface landmarks for thoracic structures include the following (Fig. 3-2): • Jugular (suprasternal) notch: a notch marking the level of the second thoracic vertebra, the top of the manubrium, and the midpoint between the articulation of the two clavicles. The trachea is palpable in the suprasternal notch. • Sternal angle (of Louis): marks the articulation between the manubrium and body of the sternum, the dividing line between the superior and the inferior mediastinum, and the site of articulation of the second ribs (useful for counting ribs and intercostal spaces). • Nipple: marks the T4 dermatome and approximate level of the dome of the diaphragm on the right side. • Xiphoid process: marks the inferior extent of the sternum and the anterior attachment point of the diaphragm. In addition to the sternal angle of Louis, physicians often use other imaginary planes of reference to assist in locating underlying visceral structures of clinical importance. Important vertical planes of reference include the following (Fig. 3-3): • Anterior axillary line: inferolateral margin of the pectoralis major muscle; demarcates the anterior axillary fold. • Posterior axillary line: margin of the latissimus dorsi and teres major muscles; demarcates the posterior axillary fold. • Scapular line: intersects the inferior angles of the scapula. • Midvertebral line: also called the “posterior median” line. The thoracic cage, which is part of the axial skeleton, includes the thoracic vertebrae, the midline sternum, the 12 pairs of ribs (each with a head, neck, tubercle, and body; floating ribs 11 and 12 are short and do not have a neck or tubercle), and the costal cartilages (Fig. 3-4). This bony framework provides the scaffolding for attachment of the chest wall muscles and the pectoral girdle, which includes the clavicle and scapula and forms the attachment of the upper limb to the thoracic cage at the shoulder joint (Table 3-1). TABLE 3-1 Joints of the thoracic cage include articulations between the ribs and the sternum and thoracic vertebrae and between the sternum and the clavicle and are summarized in Figure 3-5 and Table 3-2. TABLE 3-2 The musculature of the anterior thoracic wall include several muscles that attach to the thoracic cage but that actually are muscles that act on the upper limb (Fig. 3-6). These muscles are as follows (for a review, see Chapter 7): The true anterior thoracic wall muscles fill the intercostal spaces or support the ribs, act on the ribs (elevate or depress the ribs), and keep the intercostal spaces rigid, thereby preventing them from bulging out during expiration and being drawn in during inspiration (Fig. 3-6 and Table 3-3). Note that the external intercostal muscles are replaced by the anterior intercostal membrane at the costochondral junction anteriorly, and that the internal intercostal muscles extend posteriorly to the angle and then are replaced by the posterior intercostal membrane. The innermost intercostal muscles lie deep to the internal intercostals and extend from the midclavicular line to about the angles of the ribs posteriorly. TABLE 3-3 Muscles of the Anterior Thoracic Wall The intercostal neurovascular bundles (vein, artery, and nerve) lie inferior to each rib, running in the costal groove deep to the internal intercostal muscles (Fig. 3-7 and Table 3-4). The veins largely correspond to the arteries and drain into the azygos system of veins or the internal thoracic veins. The intercostal arteries form an anastomotic loop between the internal thoracic artery (branches of anterior intercostal arteries arise here) and the thoracic aorta posteriorly. Posterior intercostal arteries arise from the aorta, except for the first two, which arise from the supreme intercostal artery, a branch of the costocervical trunk of the subclavian artery. TABLE 3-4 Arteries of the Internal Thoracic Wall The intercostal nerves are the ventral rami of the first 11 thoracic spinal nerves. The 12th thoracic nerve gives rise to the subcostal nerve, which courses inferior to the 12th rib. The nerves give rise to lateral and anterior cutaneous branches and branches innervating the intercostal muscles (Fig. 3-7). The female breast extends from approximately the second to the sixth ribs and from the sternum medially to the midaxillary line laterally. Mammary tissue is composed of compound tubuloacinar glands organized into about 15 to 20 lobes, which are supported and separated from each other by fibrous connective tissue septae (the suspensory ligaments of Cooper) and fat. Each lobe is divided in lobules of secretory acini and their ducts. Features of the breast include the following (Fig. 3-8): • Breast: fatty tissue containing glands that produce milk; lies in the superficial fascia above the retromammary space, which lies above the deep pectoral fascia enveloping the pectoralis major muscle. • Areola: circular pigmented skin surrounding the nipple; it contains modified sebaceous and sweat glands (glands of Montgomery) that lubricate the nipple and keep it supple. • Nipple: site of opening for the lactiferous ducts; usually lies at about the level of the fourth intercostal space. • Axillary tail (of Spence): extension of mammary tissue superolaterally toward the axilla. • Lymphatic system: lymph is drained from breast tissues; about 75% of lymphatic drainage is to the axillary lymph nodes (Fig. 3-9; see also Fig. 7-11), and the remainder drains to infraclavicular, pectoral, or parasternal nodes. The primary arterial supply to the breast includes the following: • Anterior intercostal branches of the internal thoracic (mammary) arteries (from the subclavian artery) • Lateral mammary branches of the lateral thoracic artery (a branch of the axillary artery) The venous drainage (Fig. 3-9) largely parallels the arterial supply, finally draining into the internal thoracic, axillary, and adjacent intercostal veins. The thorax is divided into the following three compartments: The lungs lie within the pleural cavity (right and left) (Fig. 3-10). This “potential space” is between the investing visceral pleura, which closely envelops each lung, and the parietal pleura, which reflects off each lung and lines the inner aspect of the thoracic wall, the superior surface of the diaphragm, and the sides of the pericardial sac (Table 3-5). Normally, the pleural cavity contains a small amount of serous fluid, which lubricates the surfaces and reduces friction during respiration. The parietal pleura is richly innervated with afferent fibers that course in the somatic intercostal nerves and, over the surface of the diaphragm, the phrenic nerve (C3-C5); the visceral pleura has few, if any, pain fibers. TABLE 3-5 Clinically, it is important for physicians to be able to “visualize” the extent of the lungs and pleural cavities topographically on the surface of their patients (Fig. 3-10). The lungs lie adjacent to the parietal pleura inferiorly to the sixth costal cartilage. (Note the presence of the cardiac notch on the left side.) Beyond this point, the lungs do not occupy the full extent of the pleural cavity during quiet respiration. These points are important to know if one needs access to the pleural cavity without injuring the lungs (Table 3-6), such as to drain inflammatory exudate (pleural effusion), hemorrhage into the cavity (hemothorax), or air (pneumothorax). In quiet respiration, the lung margins reside two ribs above the extent of the pleural cavity at the midclavicular, midaxillary, and midscapular lines. TABLE 3-6 Surface Landmarks of the Pleura and Lungs • Apex: superior part of the upper lobe that extends into the root of the neck (above the clavicles). • Hilum: area located on the medial aspect through which structures enter and leave the lung. • Costal: anterior, lateral, and posterior aspects of the lung in contact with the costal elements of the internal thoracic cage. • Diaphragmatic: inferior part of the lung in contact with the underlying diaphragm. The right lung has three lobes and is slightly larger than the left lung, which has two lobes. Both lungs are composed of spongy and elastic tissue, which readily expands and contracts to conform to the internal contours of the thoracic cage (Fig. 3-11 and Table 3-7). TABLE 3-7 External Features of the Lungs The lung’s parenchyma is supplied by several small bronchial arteries that arise from the proximal portion of the descending thoracic aorta. Usually, one small right bronchial artery and a pair of left bronchial arteries (superior and inferior) can be found on the posterior aspect of the main bronchi. Although much of this blood returns to the heart via the pulmonary veins, some also collects into small bronchial veins that drain into the azygos system of veins (see Fig. 3-25). The lymphatic drainage of both lungs is to pulmonary (intrapulmonary) and bronchopulmonary (hilar) nodes (i.e., from distal sites to the proximal hilum). Lymph then drains into tracheobronchial nodes at the tracheal bifurcation and into right and left paratracheal nodes (Fig. 3-12).
Thorax
1 Introduction
2 Surface Anatomy
Key Landmarks
Planes of Reference
3 Thoracic Wall
Thoracic Cage
STRUCTURE
CHARACTERISTICS
Sternum
Long, flat bone composed of the manubrium, body, and xiphoid process
True ribs
Ribs 1-7: articulate with the sternum directly
False ribs
Ribs 8-12: articulate to costal cartilages of the ribs above
Floating ribs
Ribs 11 and 12: articulate with vertebrae only
Joints of Thoracic Cage
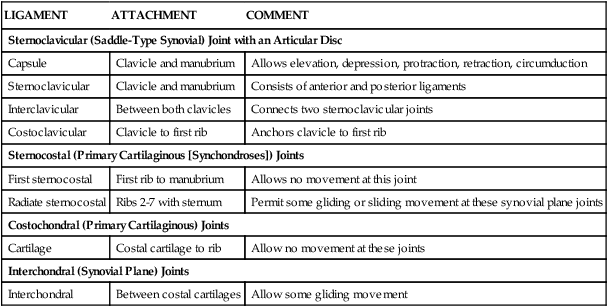
LIGAMENT
ATTACHMENT
COMMENT
Sternoclavicular (Saddle-Type Synovial) Joint with an Articular Disc
Capsule
Clavicle and manubrium
Allows elevation, depression, protraction, retraction, circumduction
Sternoclavicular
Clavicle and manubrium
Consists of anterior and posterior ligaments
Interclavicular
Between both clavicles
Connects two sternoclavicular joints
Costoclavicular
Clavicle to first rib
Anchors clavicle to first rib
Sternocostal (Primary Cartilaginous [Synchondroses]) Joints
First sternocostal
First rib to manubrium
Allows no movement at this joint
Radiate sternocostal
Ribs 2-7 with sternum
Permit some gliding or sliding movement at these synovial plane joints
Costochondral (Primary Cartilaginous) Joints
Cartilage
Costal cartilage to rib
Allow no movement at these joints
Interchondral (Synovial Plane) Joints
Interchondral
Between costal cartilages
Allow some gliding movement
Muscles of Anterior Thoracic Wall
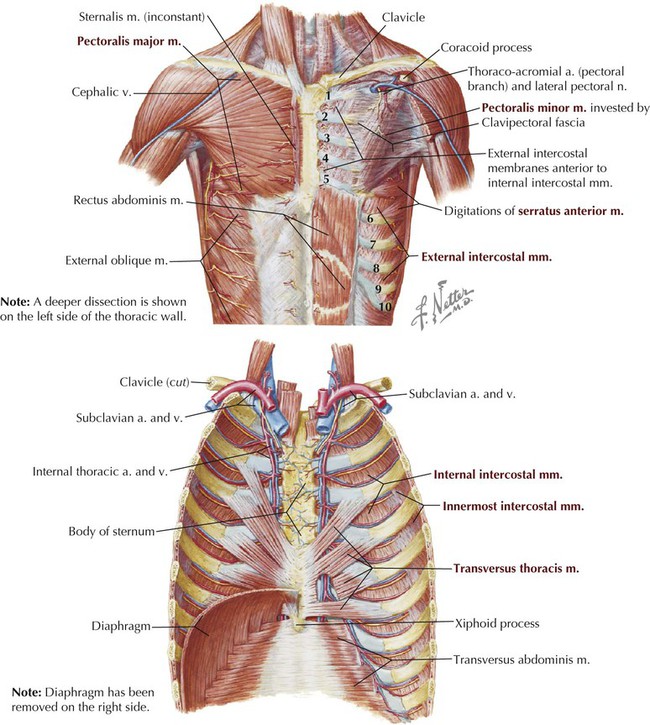
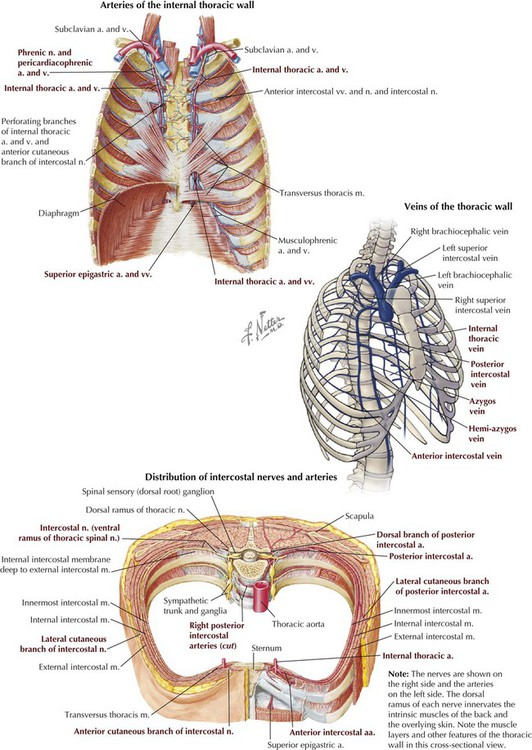
MUSCLE
SUPERIOR ATTACHMENT (ORIGIN)
INFERIOR ATTACHMENT (INSERTION)
INNERVATION
MAIN ACTIONS
External intercostal
Inferior border of rib above
Superior border of rib below
Intercostal nerves
Elevate ribs, supports intercostal space
Internal intercostal
Inferior border of rib above
Superior border of rib below
Intercostal nerves
Elevate ribs (upper four and five); others depress ribs
Innermost intercostal
Inferior border of rib above
Superior border of rib below
Intercostal nerves
Acts with internal intercostals
Transversus thoracis
Posterior surface of lower sternum
Internal surface of costal cartilages 2-6
Intercostal nerves
Depress ribs
Subcostal
Internal surface of lower rib near their angles
Superior borders of second or third ribs below
Intercostal nerves
Depress ribs
Levator costarum
Transverse processes of C7 and T1-T11
Subjacent ribs between tubercle and angle
Dorsal primary rami of C8-T11
Depress ribs and costal cartilages
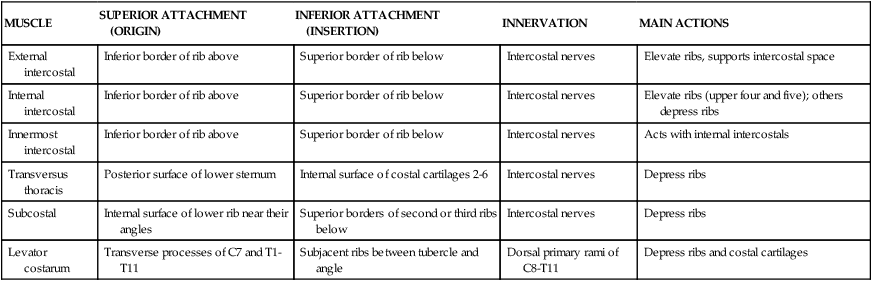
Intercostal Vessels and Nerves
ARTERY
COURSE
Internal thoracic
Arises from subclavian and terminates by dividing into superior epigastric and musculophrenic arteries.
Intercostals
First two posterior branches derived from superior intercostal branch of costocervical trunk and lower nine from thoracic aorta; these anastomose with anterior branches derived from internal thoracic artery (1st-6th spaces) or its musculophrenic branch (7th-9th spaces); the lowest two spaces only have posterior branches.
Subcostal
From aorta, courses inferior to the 12th rib.
Pericardiacophrenic
From internal thoracic and accompanies phrenic nerve.
Female Breast
4 Pleura and Lungs
Pleural Spaces (Cavities)
STRUCTURE
DEFINITION
Cupula
Dome of cervical parietal pleura extending above the first rib
Parietal pleura
Membrane that in descriptive terms includes costal, mediastinal, diaphragmatic, and cervical (cupula) pleura
Pleural reflections
Points at which parietal pleurae reflect off one surface and extend onto another (e.g., costal to diaphragmatic)
Pleural recesses
Reflection points at which lung does not fully extend into the pleural space (e.g., costodiaphragmatic, costomediastinal)
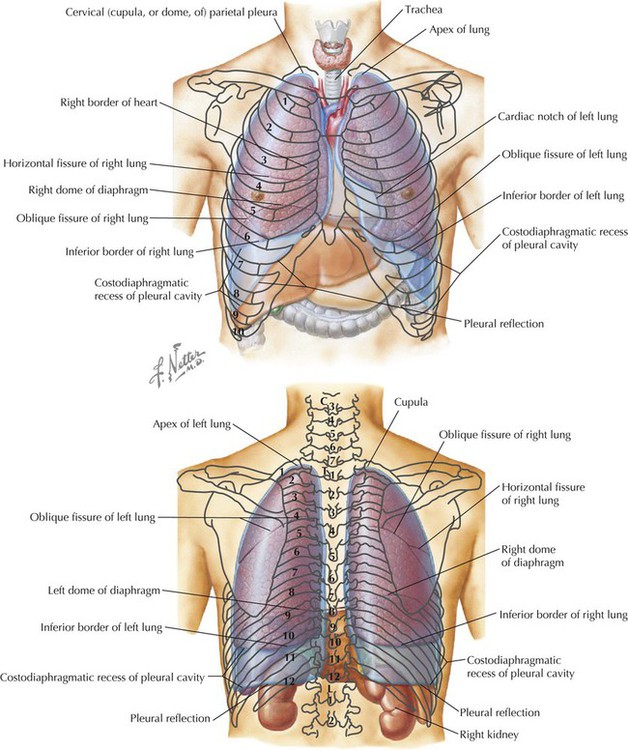
LANDMARK
MARGIN OF LUNG
MARGIN OF PLEURA
Midclavicular line
6th rib
8th rib
Midaxillary line
8th rib
10th rib
Midscapular line
10th rib
12th rib
The Lungs
STRUCTURE
CHARACTERISTICS
Lobes
Three lobes (superior, middle, inferior) in right lung; two in left lung
Horizontal fissure
Only on right lung, extends along line of fourth rib
Oblique fissure
On both lungs, extends from T2 vertebra to sixth costal cartilage
Impressions
Made by adjacent structures, in fixed lungs
Hilum
Points at which structures (bronchus, vessels, nerves, lymphatics) enter or leave lungs
Lingula
Tongue-shaped feature of left lung
Cardiac notch
Indentation for the heart, in left lung
Pulmonary ligament
Double layer of parietal pleura hanging from the hilum that marks reflection of visceral pleura to parietal pleura
Bronchopulmonary segment
10 functional segments in each lung supplied by a segmental bronchus and a segmental artery from the pulmonary artery
Thorax