Chest wall65
Introduction
10.1. Chest wall
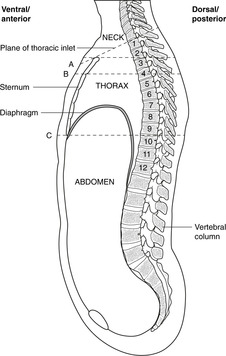
Vertebral levels and surface markings (Fig. 10.1)
Bones and joints of the chest wall (Fig. 10.2)
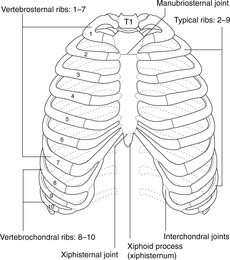
Fig. 10.2
Vertebrae
Ribs
First rib
Sternum
Joints between vertebrae and ribs
Ligaments
Joints between ribs, sternum and vertebral column
Rib
Posterior articulation
Anterior articulation
1
Vertebra T1 only
Sternum (primary cartilaginous joint, so first rib and sternum move as one)
2–7
Vertebra of same number and one above
Small synovial cavity between sternum and costal cartilage
8–9
As above
Costal cartilage articulates with cartilage immediately above
10
Vertebra of same number only
Costal cartilage articulates with cartilage immediately above
11, 12
Vertebra of same number only
None
Muscles of chest wall
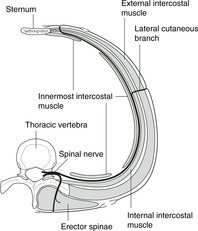
Intercostal muscles and spaces (Fig. 10.4)
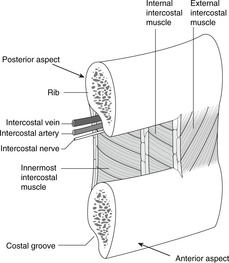
Fig. 10.4
Neurovascular bundle, costal groove
Muscles of the pectoral girdle
Insertion of chest drains (Fig. 10.5)
Blood supply of chest wall
Arteries: branches of the aorta and the subclavian/axillary artery
Veins
Intercostal nerves (Fig. 10.8)
Intercostal nerves contain both motor and sensory fibres
Intercostal nerves also convey sympathetic fibres (see later)
Segmentation, dermatomes
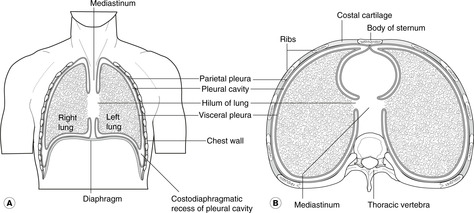
10.2. Pleural cavities, tracheobronchial tree, lungs (Figs 10.9, 10.10)
Pleural cavities, mediastinum
Pneumothorax, haemothorax
Tracheobronchial tree (Fig. 10.12)
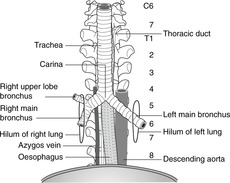
Fig. 10.12
Trachea
Palpating the trachea
Tracheal bifurcation and main bronchi
Lobar bronchi
Lungs
Lobes and fissures
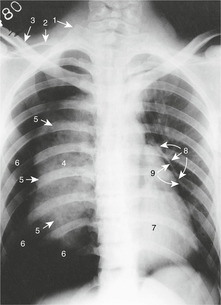
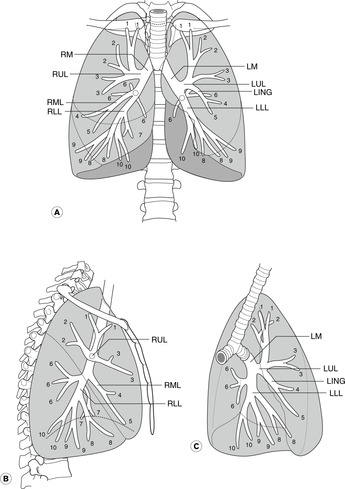
Bronchopulmonary segments (Fig. 10.13)
Right lung
Left lung
Pulmonary hila
Relations of lungs to other organs
Sensory nerve supply of pleura and lungs
Parietal pleura
Lungs and visceral pleura
Movements of breathing
Lymphatics of the thorax
Chest wall
Lungs and trachea
Tracheobronchial nodes
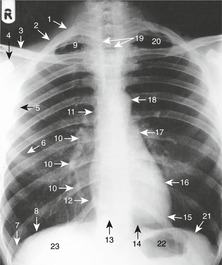
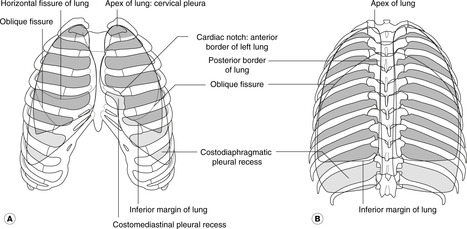
Surface markings of lungs (Fig. 10.14)
Pleural cavities and reflections
Costodiaphragmatic recess
Pleura below the ribs
Lungs
Variations in position depending upon posture and breathing
Structure
In forced expiration
In forced inspiration
Bifurcation of trachea
T4
T5/6 or lower
Hilum of lung
T5
T6 or lower
Lower border of lung
T8 (med.) to T9 (lat.)
T9 (med.) to T12 (lat.)
Listening to (auscultating) the lungs
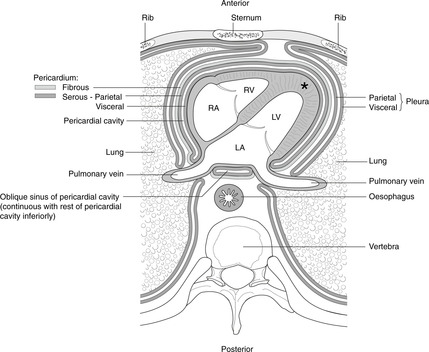
10.3. Heart and pericardial cavity
Pericardium
Fibrous pericardium (Fig. 10.15)
Pericardial cavity and sinuses
Cardiac tamponade
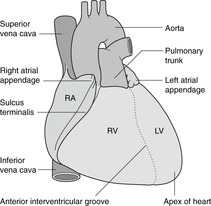
Heart
Surfaces and borders
Surfaces of the heart
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Thorax
10.2 Pleural cavities, tracheobronchial tree, lungs71
10.3 Heart and pericardial cavity77
10.4 Mediastinum85
10.5 Breast94
The thorax consists of:
• the chest wall
• the two pleural cavities surrounding the lungs
• the area between these cavities, the mediastinum, in which are found the heart, great vessels, trachea and oesophagus, vagus and phrenic nerves, thymus gland and the thoracic duct.
On the external surface of the anterolateral chest wall are the breasts (mammary glands), also considered in this chapter.
Below, the thorax is separated from the abdomen by the diaphragm; above, it is continuous with the neck at the thoracic inlet (between sternum and vertebra T1) through which structures pass between thorax and neck (Fig. 10.1).
The chest wall consists of the ribs and sternum laterally and anteriorly, and the vertebral column posteriorly, which provides most of the structural support. Ribs articulate with the vertebral column behind and the sternum in front, these articulations permitting the movements of breathing. Intercostal (between the ribs) spaces are occupied by muscle and a neurovascular bundle that supplies the muscles, the skin over them and the lining of the pleural cavity deep to them. The repeating pattern of vertebrae, ribs and the intercostal neurovascular bundle is an illustration of segmentation.
You should:
• describe the orientation of the ribs
• list the vertebral levels of the suprasternal notch, angle of Louis, and xiphisternum
• describe how ribs articulate with vertebrae and sternum
• describe the structure and contents of an intercostal space
• describe the formation and function of intercostal nerves and the dermatomes of the chest wall
• describe where and how to insert a chest drain.
Remind yourself of the significance of vertebral levels and surface markings.
• The suprasternal notch (in which you can palpate the trachea) is at vertebral level T2.
• The sternal angle (of Louis) is at vertebral level T4.
• The xiphisternum (xiphoid process) is at vertebral level T9 (about).
• Note the downwards orientation of the ribs when you consider an anterior view of the rib cage: the second rib articulates with vertebra T2 posteriorly, but with the sternal angle at vertebral level T4 anteriorly. Therefore, a transverse (horizontal) section of the thorax, such as a scan, intersects several ribs.
The chest wall is made up of the 12 pairs of ribs, the sternum and the intercostal muscles. Ribs are numbered 1–12 from above down and articulate with the vertebral column posteriorly and (mostly) the sternum anteriorly. The ribs are angled with respect to the horizontal plane – the sternal end is lower than the vertebral – and so in horizontal section, or a transverse computerised tomography (CT) or magnetic resonance imaging scan, several ribs will be seen sectioned obliquely. Ribs are united at their anterior end to cartilage: the costal cartilages.
The main features of a typical vertebra are described in Chapter 5. A thoracic vertebra is identifiable because of its facets for articulation with the ribs. Vertebrae T2–9 have two demifacets on each side, other vertebrae having only one.
Each rib has a head, neck, tubercle and shaft. Figure 10.3 shows the main features of a typical rib (ribs 2–10). Of the atypical ribs (1, 11, 12), you need only bother with the first.
• Scalene tubercle on the upper surface, to which is attached scalenus anterior muscle.
• Groove for subclavian vein, anterior to the tubercle.
• Groove for subclavian artery, posterior to the tubercle.
There are three parts, from superior to inferior: manubrium, body and xiphoid process (or xiphisternum). There may be a hole in the centre of the body, since it is formed by a number of individual sternebrae that should fuse together, but may fail to do so.
Typical ribs have three synovial articulations with the vertebrae.
• The head has upper and lower articular facets set almost at a right angle to one another, the lower articulating with the vertebra corresponding in number to the rib, and the upper with the vertebra above. Ribs 1, 10, 11 and 12 have only one facet and articulate only with the numerically corresponding vertebra.
These joints allow the ribs to move in breathing.
These ligaments are not of great importance. They include:
• triradiate ligament: from the head of the rib to the vertebra above, the intervertebral disc, and the vertebra below
• costotransverse ligaments between the vertebral transverse process and the tubercle of the rib.
• The first costal cartilage is continuous with the manubrium (primary cartilaginous joint) and remains so throughout life, unless it ossifies completely.
• Costal cartilages 2–7 have synovial articulations with the sternum. The second costal cartilage articulates at the sternal angle with the manubrium and the body of the sternum. The sternal angle (of Louis) is easily palpable and when you are counting ribs as part of a physical examination, it is best to start at the sternal angle with the second rib. In any case, the first rib is difficult to find because it is underneath the clavicle.
• Costal cartilages 8–10 have synovial articulations with the costal cartilage immediately above.
• Costal cartilages 11 and 12 are free of any anterior articulations, but provide attachments for muscles.
Articulations are summarised in Table 10.1.
• Ribs 1–7 are vertebrosternal, or true ribs.
• Ribs 8–10 are vertebrochondral or false ribs.
• Ribs 11 and 12 are floating ribs.
There are three layers of tissue between ribs, partly muscle and partly membrane: external, internal and innermost intercostals, with the intercostal neurovascular bundle running between the internal and innermost. The area between ribs, occupied by these intercostal muscles, is the intercostal space.
• External intercostal muscle. Muscle at the back and sides, membrane anteriorly. Fibres pass from the upper rib downwards and forwards to the upper border of the rib below.
• Internal intercostal muscle. Muscle at the front and sides, membrane posteriorly.
Fibres pass upwards and forwards, more or less at right angles to those of the external intercostal.
• Innermost intercostal muscle: as internal intercostal.
• Inside the chest wall there are (usually) muscle fibres that fan out from the sternum to the internal aspect of ribs 3–6. This is transversus thoracis, and it is equivalent to the transversus abdominis in the abdomen. It is not important.
These muscles are supplied by the segmental intercostal nerve corresponding in number to the intercostal space. The rib has a groove underneath most of its length on the internal aspect. This costal groove provides some shelter for the intercostal neurovascular bundle. Within the groove the neurovascular bundle is arranged, from top to bottom, vein, artery, nerve (VAN). In each intercostal space, there are also smaller branches of the intercostal nerve and artery (collateral branches) which run on top of the rib below.
Overlying the ribs and intercostal muscles externally are muscles which attach the upper limb (humerus, clavicle and scapula) to the trunk: pectoralis major, pectoralis minor, latissimus dorsi, levator scapulae, rhomboids, and trapezius. These are considered in Chapter 12.
It is occasionally necessary to insert a chest drain (a hollow tube) through the chest wall into the pleural cavity. This procedure, properly termed thoracocentesis (also thoracentesis, pleurocentesis), is performed to remove either fluid (excess pleural fluid, blood) or air that had collected in the pleural cavity (see Pneumothorax, p. 72). The position of various structures which should be avoided (heart, liver, spleen, etc.) means that there are two places on either side where this may most safely be done:
• second intercostal space in the midclavicular line
• fourth or fifth space in the midaxillary line.
To avoid any risk of damage to the main intercostal neurovascular bundle, it is better to insert the chest drain in the lower half of an intercostal space.
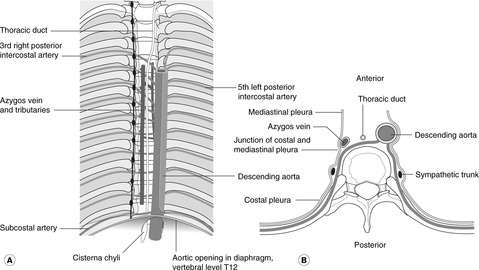
• Posterior intercostal arteries (Fig. 10.6). These are branches of the aorta (so-called segmental arteries), except for the first and second which come from the costocervical trunk, a branch of the subclavian artery (not from the aorta because it does not pass high enough in the thorax).
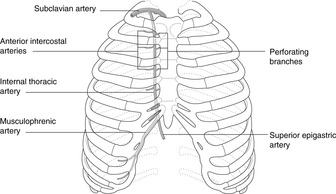
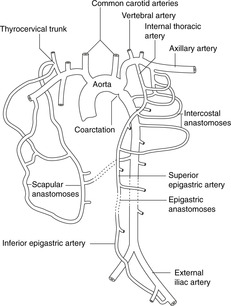
• Anterior intercostal arteries (Fig. 10.7). These arise from the right and left internal thoracic arteries, branches of the subclavian which run internally down the chest wall 1 or 2cm lateral to the sternal border. They are important in supplying the breast. Anterior and posterior intercostal arteries anastomose with each other in the intercostal space, and this potential route between the internal thoracic artery and the aorta is important in congenital aortic coarctation (narrowing) as a bypass for the narrowing (see later and Fig. 10.25, p. 88).
• Lateral thoracic artery. Again, this is important for the breast.
• Other branches of the subclavian/axillary arteries: thoracoacromial (acromiothoracic), superior (or supreme or highest) thoracic (don’t bother with these).
• Anterior intercostal veins drain to the internal thoracic veins, thence to the subclavian – brachiocephalic – superior vena cava (SVC).
• Posterior intercostal veins drain to the azygos system and the SVC. As the first one or two posterior intercostal arteries arise differently from the rest, so the posterior intercostal veins of the first few spaces drain differently: to the brachiocephalic veins (see later).
Intercostal nerves are ventral rami of the thoracic segmental nerves (see Ch. 6). Having been formed in the region of the intervertebral foramen, they run in the costal groove of each rib and supply the intercostal muscles, a strip of skin overlying the intercostal muscles and a similar strip of parietal pleura on the internal aspect of the chest wall. Anteriorly, when the ribs turn upwards, the neurovascular bundle parts company with the ribs and continues in the direction already established. Lower intercostal nerves therefore also supply skin of most of the anterior abdominal wall and the parietal peritoneum deep to it (the abdominal equivalent of parietal pleura).
• Cell bodies of motor fibres to skeletal muscle (voluntary motor fibres) are in the ventral horn of grey matter of the correspondingly numbered spinal cord segment.
• Cell bodies of sensory fibres in an intercostal nerve are in the dorsal root ganglion of the parent segmental nerve.
This arrangement gives rise to the concept of segmental innervation, and allows automatic reflex action within one segment – a physiological phenomenon particularly important clinically in the limbs.
Segmentation is most obvious in the thorax: segmental bones (ribs), segmental nerves, dermatomes, segmental vessels, and, in a way, the vertebrae. Study Fig. 6.6 (p. 36) again, which shows the dermatome pattern for the whole body, and memorise these dermatomes in the chest:
• skin over the second intercostal space (landmark: sternal angle of Louis): spinal nerve
• T2; and similarly down the chest to skin over the xiphoid process: T7 or 8.
The right and left pleural cavities surround the right and left lungs. The tissue between them that contains heart and great vessels, etc. is the mediastinum.
The pleural cavities are, like the pericardial and peritoneal cavities, serous cavities derived from the embryonic coelom. Serous cavities, which also include synovial cavities, are lined by mesothelium, a simple squamous lining which, with associated connective tissue and basement membrane, makes up the serous membranes (pleura, pericardium, peritoneum, synovium).
They are, strictly speaking, only potential cavities. Each lung invaginates each pleural cavity as it forms in such a way that the serous lining of the cavities, the pleura, is found:
• on the inside of the chest wall – the parietal pleura
• covering the lung – the visceral pleura.
Parietal pleura on the inside of the chest wall is sometimes called the costal pleura, that on the medial side of the pleural cavity the mediastinal pleura, and that on the superior aspect of the diaphragm the diaphragmatic pleura.
The two layers of pleura glide on one another (for movement in breathing), but since there is normally nothing between the visceral and parietal pleura other than a minute amount of lubricating pleural fluid, the two layers do not separate. The surface tension of pleural fluid ensures that the two layers remain adherent. A simple analogy is two sheets of glass with water between them: the two sheets may move on one another but can not easily be separated because of the film of fluid between them.
If air finds its way between the visceral and parietal pleura (e.g. a lung alveolus bursts, or a person is stabbed), then the two ‘plates of glass’ separate, the lung does not move with the chest wall and the elastic tissue in the lungs causes them to collapse, thus preventing normal breathing. This is a pneumothorax (Fig. 10.11). If a blood vessel bleeds into the pleural cavity, a haemothorax develops. These conditions are treated by the insertion of a chest drain (Fig. 10.5, see p. 68).
The trachea begins at the level of the cricoid cartilage (vertebral level C6) and descends to its bifurcation (vertebral level about T4 in the supine position and T5 or 6 in the erect position). Its walls are made up of incomplete rings of hyaline cartilage closed posteriorly by connective tissue and trachealis muscle (involuntary muscle). Behind it is the oesophagus and between the two in the neck are the recurrent laryngeal nerves (see later).
The trachea should be central in the suprasternal notch (vertebral level T2), and palpation of this is a routine part of a thorough clinical examination. If the trachea is deviated to one side or the other, this implies that it has been displaced by disease (e.g. a tumour or a pneumothorax pushing it to the other side).
At the bifurcation of the trachea, the two main bronchi arise and these pass into the lungs at the hila with the pulmonary (Latin: pulmo = lung) arteries and veins. At the bifurcation, the internal ridge that separates the two main bronchi is the carina (Latin: keel) and this should be fairly sharp. The area immediately beneath the bifurcation is occupied by tracheobronchial lymph nodes, which are often involved in malignant disease. If, at bronchoscopy, the carina is less than sharp, it is likely that tracheobronchial lymph nodes are enlarged.
The right main bronchus is slightly larger in calibre than the left, and this is one reason why inhaled foreign bodies more often pass into the right main bronchus. Both bronchi pass inferolaterally from the tracheal bifurcation, but the angulation of the bronchi is by no means constant. In some people the arrangement is more or less symmetrical, whereas in others the right main bronchus is more in line with the trachea than the left. The right main bronchus passes directly to the hilum of the right lung. The left main bronchus passes anterior to the oesophagus, which it indents (vertebral level T4/5, see later) and thence to the hilum of the left lung.
The right and left main bronchi each give lobar bronchi to the lobes of the lungs, and these divide into segmental bronchi, each serving its own bronchopulmonary segment (see later). The incomplete cartilaginous rings, like those in the trachea, persist into the lobar bronchi. Structural support to smaller bronchi is provided by randomly arranged plates of cartilage in the wall.
The lungs are divided by fissures into lobes. The right lung has three lobes: upper, middle and lower; the left lung has two: upper and lower. The left-sided equivalent of the right middle lobe is the lingula – part of the left upper lobe. The lobes are demarcated by fissures: oblique and horizontal on the right, and oblique only on the left. The horizontal fissure is sometimes incomplete.
Occasionally on the right, the developing azygos vein may invaginate its way into the apical portion of the right upper lobe, thus creating a ‘peninsula’ of lung tissue. This azygos fissure and lobe may be mistaken on a chest radiograph for a pathological condition.
Each lung is made up of a number of bronchopulmonary segments, each with its own bronchus, its own branch of the pulmonary artery, and its own tributary of the pulmonary vein. These discrete units enable surgeons to excise one or more bronchopulmonary segments when disease is confined to them without compromising the function of other segments. You need to know them.
• Upper lobe: apical, posterior and anterior bronchopulmonary segments.
• Middle lobe: lateral and medial bronchopulmonary segments.
• Lower lobe: apical, medial, anterior, lateral and posterior bronchopulmonary segments.
Conventionally, the segments are numbered 1–10 in the order given. To avoid confusion between upper and lower lobes, the lower lobe segments are often called apical basal, medial basal, and so on.
The pattern is modified somewhat:
• The middle lobe is replaced by the superior and inferior segments of the lingula (parts of the upper lobe).
• There is no medial basal segmental bronchus and the left medial basal segment may be much reduced in size or even absent as a result of the presence of the heart.
• There may be a common origin from the left upper lobe bronchus for the left upper lobe apical and posterior segmental bronchi, although the segments themselves are separate, as on the right.
You should bear in mind that there is, as usual, some variation in this pattern from person to person. It is interesting, but of no relevance, to know that in pigs, sheep, llamas and tigers one of the right lobar bronchi arises from the trachea itself.
These are the regions where arteries, veins, the bronchial tree, nerves and lymphatics pass between mediastinum and lungs. You need not bother with the precise arrangement of structures at the hilum except to know that the bronchi are posterior and the pulmonary arteries superior. The pulmonary ligament is the narrow inferior extension of the hilum, containing nothing of importance.
A number of important mediastinal structures are intimately related to the lungs and create impressions on the medial aspect of both lungs. On the right lung, those formed by the superior vena cava, the azygos vein and the oesophagus are noteworthy. On the left side, the impressions of the heart, the aortic arch and descending aorta are obvious.
• Costal: local intercostal nerves
• Diaphragmatic: local intercostal nerves (peripherally), phrenic nerve (centrally)
• Mediastinal: phrenic (mainly).
Parietal pleural sensation is somatic sensation, and pain from irritation of parietal pleura will be sharp and well localised by the patient.
The lungs and visceral pleura, like all internal organs, are supplied by visceral sensory nerves that travel back to the central nervous system in nerves also conveying sympathetic and/or parasympathetic fibres. Visceral pain is much more vague and poorly localised by the patient. Inflammation of the pleura is called pleurisy and the sharp pain commonly associated with it arises not from irritation of the visceral pleura but from irritation of parietal pleura to which the disease has spread.
Normal breathing is the result of movement of the diaphragm. The diaphragm descends, the diaphragmatic parietal pleura descends and, since the two layers of pleura can not separate, this pulls the visceral pleura down so that the lung alveoli and airways expand and air is sucked in. In expiration, the diaphragm relaxes and the elastic tissue in the lung recoils, thus expelling air in the airways. In forced inspiration other muscles are used and these include any muscles that will enlarge the rib cage in any way. Neck muscles (sternocleidomastoid) will pull it up, abdominal muscles (quadratus lumborum) will pull it down, and by fixing the upper limbs, pectoral girdle muscles (pectoralis major, latissimus dorsi) will pull it out. These are accessory muscles of respiration and you will see them in action in any patient suffering a bronchitic or asthmatic attack. The function of the intercostal muscles is not fully understood, despite what anyone may tell you, but obviously they afford a degree of flexibility between the more rigid ribs.
The shape of the costotransverse joints allows the lateral aspect of the lower ribs to swivel up and out, thus increasing the lateral diameter of the chest. The anterior ends of all ribs can swing up and out, thereby increasing the anteroposterior diameter of the chest. Disease resulting in limitation of movement at these joints can be a cause of respiratory distress.
Both these lymphatic channels communicate with those of the breast and may be involved in the spread of breast disease.
There are communicating lymph plexuses immediately under the visceral pleura and around the bronchial tree. From here lymph passes to the hilum where hilar nodes are found and thence to the mediastinal nodes and the thoracic duct.
These are the mediastinal lymph nodes immediately beneath the carina. They constitute the largest collection of lymph nodes in the body and receive lymph from heart, lungs and mediastinal structures such as the oesophagus. Enlargement of these nodes will cause a widening of the carina when viewed at bronchoscopy (see above).
These are important. The pleura extends above the clavicle into the neck where it is vulnerable to stab wounds, so do not be surprised if a patient who has been stabbed above the clavicle is breathless: there may be a pneumothorax. In this region the superior limit of the pleural cavity is formed by the suprapleural membrane, a half-tent of membrane suspended from the transverse process of vertebra C7 to attach to the inner aspect of the first rib.
Remember 2, 4, 6, 8, 10, 12. From about 2cm above the clavicle, the line of pleural reflection passes behind the sternoclavicular joint and almost meets its fellow of the other side behind the sternal angle (level of second costal cartilage), then down to the level of the fourth costal cartilage where the left line passes laterally but the right continues down to the sixth. The lines then pass obliquely laterally across the sixth cartilage, crossing the eighth rib in the midclavicular line, the tenth rib in the midaxillary line and the twelfth rib (behind now) in the midscapular line, or even lower.
Note that at the back the costodiaphragmatic recesses of the pleural cavities are behind the upper poles of the kidneys.
The three sites where the pleural reflection is below the costal margin are:
• right costosternal region (not the left, because of the heart)
• between the twelfth rib and the vertebral column on the right
• between the twelfth rib and the vertebral column on the left.
In these places abdominal incisions may enter the pleural cavity.
These are similar to the pleura except that lung tissue does not normally extend much below vertebral level T10, and of course the extent of the lungs varies during breathing with inspiration and expiration.
• Oblique fissure (both sides): spine of vertebra T2 or T3 – sixth costal cartilage.
• Horizontal fissure (right lung only): level of fourth costal cartilage, sternal edge – line of oblique fissure.
You should bear in mind that structures move during breathing. Vertebral levels are given in Table 10.2.
Finally, it should be obvious that everything will be lower when you are standing erect than when you are lying down. For these reasons, surface markings and vertebral levels are only approximate.
From a clinical point of view you should note the following:
• When you place your stethoscope on a patient’s back, you are listening mainly to the lower lobe. There is a small area of upper lobe, but no middle lobe at all.
• When you place your stethoscope on a patient’s anterior chest wall, you are listening mainly to the upper and middle lobes.
• You will listen to the middle lobe best by placing the stethoscope at the side and in the axilla.
• You can not listen to individual bronchopulmonary segments, or even to individual lobes.
• When a patient is lying in bed on his back, the most dependent bronchopulmonary segments are the apical and posterior segments of the lower lobe. These segments are most often affected by lung infections in ill, bedridden patients.
• In normal breathing, lung tissue does not occupy the lower extremities of the costodiaphragmatic recesses, but it may in deep inspiration. This means that in this region the surface markings of the extent of the lungs is different from the surface markings for the extent of the pleural cavities.
The heart is surrounded by visceral and parietal layers of serous pericardium (equivalent to the pleura), and external to these the fibrous pericardium. The heart and pericardial cavity are in the anterior mediastinum, behind the sternum slightly to the left of the midline. The heart is oriented such that the right chambers of the heart are more anterior, and the left chambers more posterior. The outflow from each chamber is guarded by a valve: right atrium–tricuspid; right ventricle–pulmonary; left atrium–mitral; left ventricle–aortic. The cardiac conducting system is the means by which contraction is coordinated. Right and left coronary arteries from the ascending aorta supply heart muscle with freshly oxygenated blood. The inherent rhythmicity of cardiac muscle is modulated by the autonomic innervation of the heart, amongst other things.
You should:
• describe the arrangement of the pericardium around the heart, and the importance of cardiac tamponade
• list the surface markings of the heart and its borders as seen on a posteroanterior chest radiograph
• describe the route taken by blood as it passes through the chambers and valves of the heart, and know how to perform external cardiac massage
• list the position, surface anatomy and importance of the cardiac valves
• describe the disposition and importance of the conducting system
• describe the anatomy of the right, left, circumflex, anterior interventricular and posterior interventricular coronary arteries
• describe where to place your stethoscope in order to listen to the various elements of cardiac function.
The serous pericardium, and the heart inside it, are then enclosed in a sac of tough fibrous tissue, the fibrous pericardium. It is simply like a plastic bag closed round the ‘neck’ of the heart (the great vessels) and is firmly attached to the underlying parietal layer of serous pericardium.
So, there are two types of pericardium, fibrous and serous, and there are two layers of serous pericardium. Note that it is the serous pericardium that is equivalent to the pleura. As in the pleural cavity, the pericardial cavity is only a potential cavity: it contains a minute amount of pericardial fluid and is there to facilitate gliding movements such as occur during the beating of the heart, but it does not allow separation of the two layers of serous pericardium.
The cardiac equivalent of the hilum of the lung, that is the place where structures pass between the heart and the rest of the mediastinum, is not as ‘tidy’ as the pulmonary hilum. The embryology of the great arteries (aorta, pulmonary) and veins (inferior vena cava, superior vena cava and pulmonary veins) results in the area posterior to the heart being complex.
• That part of the pericardial cavity behind the heart is the oblique sinus separating the left atrium (the original left side of the heart is now at the back) from the oesophagus.
• The transverse sinus is the potential communication between the right and left sides of the pericardial cavity found behind the great arteries (ascending aorta, pulmonary artery) and in front of the superior vena cava.
It is important to realise that the fibrous pericardium is indeed fibrous and not elastic. If fluid were to collect in the pericardial cavity, the pericardial covering would not be able to expand to accommodate it and the beating of the heart would become increasingly compromised. This is cardiac tamponade – a potentially fatal emergency. It may arise from pericarditis (inflammatory fluid in the pericardial cavity) or from rupture of one of the coronary vessels or even of the heart wall itself, resulting in blood in the pericardial cavity (haemopericardium).
The heart develops as a midline structure. It subsequently shifts so that the left side becomes posterior and the right side anterior. Despite this, the terms left and right are used and you might bear in mind that right can often, but not always, be translated as anterior, and left as posterior.