Thoracic Trauma
J. Wayne Meredith
J. Jason Hoth
Introduction
Trauma continues to be a significant source of patient morbidity and mortality, accounting for 140,000 deaths annually and is the leading cause of death in patients younger than 40 years. Although rarely isolated, thoracic injuries are a primary or contributing cause of death in up to 75% of all trauma-related deaths. Fortunately, the majority of thoracic injuries can be treated effectively, and often definitively, by relatively simple maneuvers at the bedside such as tube thoracostomy. However, 10% to 15% of patients presenting with thoracic trauma have severe, life-threatening injuries that require definitive operative repair. In these patients, the timing of intervention and utilization of the appropriate surgical approach are crucial and should be based on a comprehensive knowledge of the location and nature of the injury. These extremes in injury severity are unique to the chest and require a correspondingly broad range of knowledge and skills on the part of the treating surgeon.
Initial Evaluation
Initial evaluation and treatment of patients with thoracic injuries are guided by the same principles and priorities as initial evaluation and treatment of patients with other injuries. The first priority is to ensure an adequate airway and ventilation. Patients with severe chest trauma commonly require nasotracheal or orotracheal intubation. It is frequently during this stage of evaluation that tube thoracostomy is required for life-threatening pneumothorax. The next priority is control of external hemorrhage and restoration of circulation. External hemorrhage is best controlled by direct pressure. Inadequate perfusion generally results from either hypovolemia or pump (i.e., cardiac) problems. Hypovolemia from hemorrhage, by far the most common cause of inadequate perfusion in the traumatic setting, often must be treated operatively as part of the resuscitative effort. Pump problems are signaled by distended neck veins and are caused by one of four conditions: (a) tension pneumothorax, (b) pericardial tamponade, (c) coronary air embolism, or (d) cardiac contusion or myocardial infarction (MI). In most blunt trauma patients, urgent treatment of thoracic injury is accomplished during the primary survey because the most common blunt chest injuries can be controlled with endotracheal intubation or tube thoracostomy.
Ed Thoracotomy
Emergency room thoracotomy is a drastic procedure with limited utility. The therapeutic goals of ED thoracotomy (EDT) include control of hemorrhage, effective cardiac compression, cross-clamping the pulmonary hilum in the case of air embolism or massive bronchopleural fistula, relief of cardiac tamponade, and crossclamping of the descending aorta for lower torso hemorrhage control.
Indications
When making a decision to perform an EDT, three factors must be taken into consideration: mechanism of injury, location of major injury, and signs of life. Better outcomes are seen when performed for penetrating (8% to 10%) injuries rather than blunt injuries (∼1%). Patients with isolated penetrating chest injuries have the greatest chance of survival, and the absence of signs of life (palpable pulse, pupillary or gag reflex, and demonstrable blood pressure) must be considered. In general, the patients most likely to respond favorably to EDT include victims of penetrating trauma with signs of life either upon presentation to the emergency room or that lose signs of life within 10 minutes of arrival.
Surgical Technique
Once the decision has been made to intervene, the standard incision is a left anterolateral thoracotomy. After evacuating blood
from the chest, attention is directed to the injury. If a great vessel is injured and bleeding, pressure is utilized to staunch hemorrhage. If air embolism is encountered, the pulmonary hilum is clamped or the affected lung may be twisted 180 degree and air in the aorta evacuated. When hemopericardium is present, the pericardium may be divided longitudinally, and once the hemopericardium is evacuated, the heart is delivered from the pericardial sac and a temporary repair is then performed using suture or staples. After the cause of arrest has been addressed, a crossclamp may be applied to the descending thoracic aorta. Intravascular volume is restored and if the patient responds, transported to the operating room for definitive repair of injuries.
from the chest, attention is directed to the injury. If a great vessel is injured and bleeding, pressure is utilized to staunch hemorrhage. If air embolism is encountered, the pulmonary hilum is clamped or the affected lung may be twisted 180 degree and air in the aorta evacuated. When hemopericardium is present, the pericardium may be divided longitudinally, and once the hemopericardium is evacuated, the heart is delivered from the pericardial sac and a temporary repair is then performed using suture or staples. After the cause of arrest has been addressed, a crossclamp may be applied to the descending thoracic aorta. Intravascular volume is restored and if the patient responds, transported to the operating room for definitive repair of injuries.
The secondary survey should focus on more subtle evidence of injury that may be detected on physical examination and chest X-ray. Simple rib fractures, flail chest segments, pneumothorax, and hemothorax often go undetected during the primary survey, but are common findings later in the workup. Because of continuing improvements in CT scanning technology, this modality is increasingly being used in the evaluation of the thoracic trauma in stable patients. Indeed, chest CT angiography (CTA) is now routinely employed for definitive diagnosis of aortic and great vessel injuries, rendering standard angiography unnecessary in most cases. Additionally, chest CT scanning is also useful in the diagnosis of pulmonary contusion, tracheobronchial, and esophageal injuries. Furthermore, echocardiography can be an important adjunct for assessing proximity wounds to the heart or evaluating a new murmur.
Indications for urgent operative treatment of thoracic injuries fall into five broad categories: (a) hemorrhage, (b) major airway disruption, (c) cardiac and vascular injuries, (d) esophageal disruption, and (e) diaphragmatic disruption. The extent and location of hemorrhage can sometimes be determined from open wounds, but is more often established after chest tube insertion. It is important to understand that the pulmonary circulation is a low pressure system and complete reexpansion of the lung will tamponade parenchymal bleeding. In general, if 1,500 mL of blood or more is obtained initially or ongoing bleeding at a rate of 300 mL/h or higher for 3 hours is noted, thoracotomy is generally indicated. Caveats to the use of chest tube drainage as an indicator of chest explorations are chest trauma with a delayed presentation and the presence of a coagulopathy. Massive air leakage and the presence of gastric or esophageal contents in the chest tube effluent also necessitate surgical intervention. A continuous air leak seen in conjunction with inability to expand the lung completely or with inadequate tidal volumes is considered a massive air leak. These findings suggest major tracheobronchial injuries. The presence of cardiac tamponade, demonstrated using a combination of findings on physical examination (Beck’s triad: muffled heart tones, distended neck veins, and hypotension) and more recently, by the presence of a pericardial effusion on FAST examination, demands further evaluation with pericardial window or median sternotomy. Lastly, air embolism, a rare entity associated with penetrating injury, occurs when a fistula develops between a bronchus and pulmonary vein and also requires urgent thoracotomy. Typically, the patient is stable until intubated and placed on positive pressure ventilation when sudden cardiovascular collapse and/or the onset of lateralizing neurologic symptoms occur.
Choice of Incision
Given the indications for chest exploration, selecting the appropriate chest incision is critically important. What makes this decision difficult is that four different compartments must be considered: the right chest, left chest, mediastinum, and in the case of concomitant abdominal injury, the peritoneal cavity. Several factors should be carefully measured before making a decision. Information regarding missile or injury trajectory, a thorough working knowledge of thoracic/mediastinal anatomy, and the exposures offered by each different incision are vital for choosing the appropriate incision. For example, a left parasternal gunshot wound may injure both the anterior and the posterior walls of the left ventricle. Of these two injuries, while the anterior injury is easily exposed and repaired through a median sternotomy or anterior thoracotomy, the posterior injury is more difficult to repair and is best approached with a left posterolateral thoracotomy. A summary of surgical approaches for common traumatic injuries to thoracic viscera are summarized in Table 1.
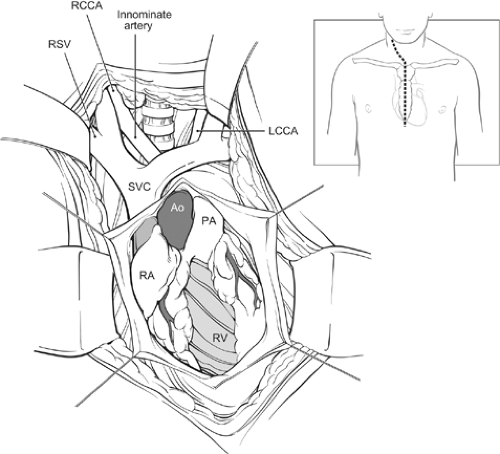
Median sternotomy (Fig. 1) offers adequate exposure for the majority of parasternal stab wound as these injuries do not typically penetrate deeply and primarily involve the anterior mediastinum. Likewise, in the instance of right parasternal GSW, a median sternotomy provides good exposure of structures that are likely to be injured, including the right atrium and ventricle, the superior vena cava, the atrial appendage, the right pulmonary artery, and the lung. Furthermore, the incision for a sternotomy may be extended into the neck or supraclavicular fossa to enhance exposure of the great vessels (Fig. 1, inset). As previously stated, posterolateral thoracotomy provides superior exposure of the posterior heart and should be used in instances of left parasternal GSW. Additionally, for lateral wounds, depending on the side involved, a right or left posterolateral thoracotomy provides the best exposure as these injuries are more likely to be posterior. In cases of massive hemothorax, a posterolateral thoracotomy on the affected side will offer excellent visualization of the great vessels such as the subclavian artery or aorta. A left posterolateral thoracotomy (Fig. 2) is the incision of choice in instances of air embolism and massive air leak.
Right thoracotomy is an excellent approach for right lung, tracheal and proximal left mainstem bronchial injuries (a point that is often forgotten). Most upper and midesophageal injuries are best approached through a right thoracotomy except in cases of distal esophageal injuries that are best accessed through the left chest. Right heart structures such as the right atrium, right ventricle, atrial appendage, as well as the left atrium are also easily exposed with a right thoracotomy. Left thoracotomy provides adequate exposure of the left lung, the left pulmonary hilum, the aorta, the proximal left subclavian artery, the left heart chambers, the distal esophagus, and the distal left mainstem bronchus. A “clam shell” incision, formed by extending a thoracotomy incision transversely across the sternum using either the Lebsche knife, a pair of trauma shears or a saw, provides excellent access, but suboptimal exposure of every intrathoracic or mediastinal structure except the right ventricle and the right atrium. When using this approach, the internal mammary arteries are divided and often do not bleed in the poorly perfused patient. However, once blood pressure is restored, significant hemorrhage from these vessels may result. A more stable closure of the transverse sternotomy may be achieved with sternal plates rather than wires.
Chest Wall Injuries
Rib Fractures
Clinical Presentation and Diagnosis
Rib fractures are the most common chest wall injuries resulting from blunt trauma. The main pathophysiologic consequences of rib fractures are pain, splinting, and prevention of adequate cough. The diagnosis should be suspected if pain or splinting occurs on deep inspiration, and it is confirmed by careful physical examination, consisting of anterior–posterior and lateral–lateral manual compression. If an alert patient feels no pain when these maneuvers are done, clinically significant rib fractures can be excluded. Although rib fractures are often identified on routine chest radiographs, they are more likely to be undetectable on plain radiographs; however, chest CT identifies rib fractures with high sensitivity and specificity.
Treatment
Pain control for isolated rib fractures can usually be adequately accomplished with oral analgesics, encouraging good pulmonary toilet, and use of thoracic epidural anesthesia in select patients. Increasingly, reports have demonstrated the feasibility of rib fracture repair using a variety of different methods. Potential indications for operative repair of rib fractures include flail chest, painful moveable rib fractures, which are refractory to conventional management, chest wall deformity/defect, rib fracture nonunion, and during thoracotomy for other indications. In isolated reports, clinical outcomes have been excellent when repair is undertaken and most trauma surgeons feel as though there is a role for rib repair; however, there is a need for clinical trials documenting the superiority of rib fracture repair versus conventional management in select patient populations.
Sternal Fractures
Clinical Presentation and Diagnosis
The vast majority of sternal fractures results from motor vehicle crashes and may be associated with significant underlying thoracic and abdominal injuries. The diagnosis of sternal fracture is based on the presence of severe pain, often associated with instability, on sternal palpation. Sternal fractures are almost invariably transverse, with the majority occurring near the sternomanubrial joint.
Table 1 Surgical Approaches for Traumatic Injuries to Thoracic Viscera | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Initial management of a sternal fracture is directed toward resuscitation and identification or exclusion of other life-threatening injuries. In patients with isolated sternal fractures, a normal electrocardiogram and chest radiograph suggest that associated serious injuries are unlikely. If the pain is controlled with oral analgesics, these fractures can usually be managed on an outpatient basis. The vast majority of sternal fractures heal with nonoperative management. Those that are unstable or are displaced by more than 1 cm of overlap are more likely to exhibit malunion or nonunion and subsequent chronic pain; they may require treatment with open reduction and internal fixation.
Flail Chest
Clinical Presentation and Diagnosis
Flail chest is the most serious of the blunt chest wall injuries. It is common after any form of blunt thoracic trauma, and though it may occur as an isolated finding, it is usually associated with other significant injuries. It involves fractures of adjacent ribs, each of which is fractured in two or more places, so that a panel of chest wall moves independently of, and in the opposite direction to, the remainder of the chest (i.e., paradoxical motion) with spontaneous respiration. A flail segment may be overlooked in a patient on positive pressure ventilation because there may be no paradoxical motion without inspiratory effort. The pathophysiology of flail chest consists of three components: alteration of chest wall mechanics impairing adequate ventilation; pulmonary contusion resulting in shunting to produce hypoxemia; and pain with associated splinting and inadequate pulmonary toilet, setting the stage for subsequent infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree