Fig. 41.1 The synthesis of thyroid hormones.
Iodide is oxidised to iodine by thyroid peroxidase and incorporated into tyrosine residues of thyroglobulin, the colloidal substance that fills the lumen of the thyroid follicles. Conjugation of mono-iodotyrosine (MIT) and di-iodotyrosine (DIT) residues into T3, or of two DIT residues to form T4, is followed by the release of T3 and T4 when thyroglobulin is proteolysed.
The synthesis and release of thyroid hormones are controlled by the anterior pituitary hormone thyrotropin (thyroid-stimulating hormone, TSH). This in turn is controlled by the hypothalamus, which secretes thyrotropin-releasing hormone (TRH). Circulating T3 and T4 exert negative feedback on both the hypothalamic and pituitary hormones (Fig. 41.2).
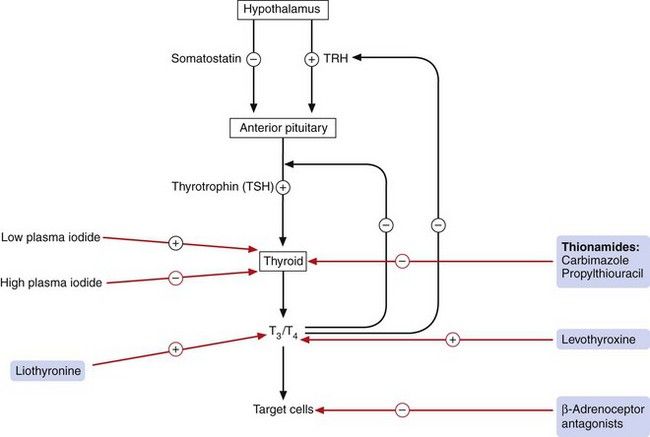
Fig. 41.2 Control of thyroid hormone synthesis and release.
Thyrotropin (thyroid-stimulating hormone, TSH) and thyrotropin-releasing hormone (TRH) are inhibited by circulating levels of T3 and T4. The sites of action of drugs acting on thyroid pathways are also shown.
The thyroid secretes mainly T4 and a small amount of T3. Circulating thyroid hormones are highly protein-bound, mostly to thyroxine-binding globulin (TBG). Less than 0.03% of T4 and less than 0.3% of T3 circulate unbound and only this free fraction of hormone is available to bind to specific intracellular receptors. Most T3 is derived from peripheral deiodination of T4 by iodothyronine deiodinase, which is found in the liver, kidney, brain and brown adipose tissue. About 35% of T4 is converted to T3, while about 40% is converted to reverse T3 (a metabolically inactive isomer of T3). T3 has a half-life in the circulation of about 1.5 days compared with about 7 days for T4. Elimination of T3 and T4 is by conjugation, mainly in the liver.
Thyroid hormones cross cell membranes via active transporters and bind to intracellular thyroid hormone receptors (or TRs) (Ch. 1), which belong to the superfamily of nuclear receptors. Thyroid hormone receptors usually repress target genes but, following thyroid hormone binding, the complex recruits co-activators and regulates gene transcription via thyroid response elements. Thyroid hormone receptors are expressed in most tissues, but there are three isoforms which differ in their tissue distribution and may mediate different effects of thyroid hormones. T3 also has non-genomic actions that include stimulation of cellular uptake of amino acids and glucose, and interactions with G-protein-coupled membrane receptors with activation of phosphatidylinositol 3-kinase and mitogen-activated protein kinase (MAPK) pathways.
Hyperthyroidism
The commonest form of hyperthyroidism (often, and interchangeably, called thyrotoxicosis) is Graves’ disease, an autoimmune condition in which thyroid-stimulating immunoglobulin binds to thyrotropin (TSH) receptors on thyroid cells and initiates signal transduction. This is often accompanied by an immunologically mediated inflammatory reaction in the extrinsic muscles and fat of the orbit, causing swelling and the characteristic exophthalmos. Toxic multinodular goitre, thyroid adenomas (toxic or ‘hot’ nodules) and various forms of thyroiditis are much less common causes of hyperthyroidism. Rarely, the condition arises from excess production of thyrotropin or it can be induced by treatment with amiodarone (Ch. 8). Symptoms of hyperthyroidism include weight loss, palpitation, sweating, fatigue, nervousness, heat sensitivity and tremor. These are in part mediated by the action of excess thyroid hormone, and partly by excess sensitivity of tissues to β-adrenoceptor stimulation. Signs are often less marked in the elderly, who are more likely to present with atrial fibrillation that is resistant to treatment.
Drugs for treatment of hyperthyroidism
Mechanism of action: Thionamides inhibit thyroid peroxidase and, therefore, the synthesis of thyroid hormone (Fig. 41.2). The long half-life of T4 means that changes in the rate of synthesis take 4–6 weeks to lower circulating T4 and T3 concentrations to within the normal range. These drugs also appear to have an immunosuppressant effect in individuals with autoimmune thyroid disease. They reduce the levels of thyroid-stimulating immunoglobulin, although the clinical importance of this is uncertain. Large doses of propylthiouracil also decrease peripheral conversion of T4 to T3.
Pharmacokinetics: Carbimazole is converted by first-pass metabolism to the active derivative methimazole. Propylthiouracil has about one-tenth of the activity of methimazole and a shorter half-life; it is usually reserved for individuals intolerant to carbimazole. Both drugs accumulate in the thyroid, which extends their duration of action.
 Gastrointestinal upset (especially nausea and epigastric discomfort), headache, arthralgia and pruritic rashes are common in the first 8 weeks of treatment.
Gastrointestinal upset (especially nausea and epigastric discomfort), headache, arthralgia and pruritic rashes are common in the first 8 weeks of treatment. Allergic reactions, including vasculitis, a lupus-like syndrome, myopathy, cholestatic jaundice and nephritis. Some cross-sensitivity occurs between carbimazole and propylthiouracil.
Allergic reactions, including vasculitis, a lupus-like syndrome, myopathy, cholestatic jaundice and nephritis. Some cross-sensitivity occurs between carbimazole and propylthiouracil. Bone marrow suppression, especially agranulocytosis, is an important unwanted effect and is more common with propylthiouracil than with carbimazole. A severe sore throat with fever is often the presenting complaint, and the occurrence of this, or any other infection, should be immediately reported to a doctor. The onset of agranulocytosis is sudden, and probably immunologically mediated, so that routine blood counts are unhelpful for monitoring. The blood count usually recovers about 3 weeks after drug withdrawal.
Bone marrow suppression, especially agranulocytosis, is an important unwanted effect and is more common with propylthiouracil than with carbimazole. A severe sore throat with fever is often the presenting complaint, and the occurrence of this, or any other infection, should be immediately reported to a doctor. The onset of agranulocytosis is sudden, and probably immunologically mediated, so that routine blood counts are unhelpful for monitoring. The blood count usually recovers about 3 weeks after drug withdrawal. Placental transfer of the active metabolite of carbimazole can produce neonatal hypothyroidism, but propylthiouracil does not transfer in large enough quantities to cause problems. However, in Graves’ disease the thyroid-stimulating antibody crosses the placenta and causes fetal thyrotoxicosis; therefore, carbimazole is the treatment of choice for maternal Graves’ disease. Carbimazole is secreted in breast milk but rarely produces hypothyroidism in the infant.
Placental transfer of the active metabolite of carbimazole can produce neonatal hypothyroidism, but propylthiouracil does not transfer in large enough quantities to cause problems. However, in Graves’ disease the thyroid-stimulating antibody crosses the placenta and causes fetal thyrotoxicosis; therefore, carbimazole is the treatment of choice for maternal Graves’ disease. Carbimazole is secreted in breast milk but rarely produces hypothyroidism in the infant.Management of hyperthyroidism
Carbimazole is the drug of choice for Graves’ hyperthyroidism, and will usually decrease the thyroid hormone concentration to normal levels over 4–8 weeks. It is usual to start treatment with a high dosage unless the thyrotoxicosis is mild, when smaller initial doses may be more appropriate. Once the thyroid hormone concentration is normal, the dosage is then gradually reduced every 4–6 weeks to reach the lowest possible dose that controls the serum T4. Initially treatment should be continued for 12–18 months, after which the dose can be tapered or treatment withdrawn. Occasionally, a block–replace regimen is used, giving a high dosage of carbimazole in conjunction with thyroxine replacement for 6–12 months. This maintains normal thyroid function regardless of the dose of carbimazole.
A β-adrenoceptor antagonist (especially propranolol because of its non-selective action; Ch. 5) is particularly useful for symptomatic relief from tremor, anxiety or palpitation during the early period of treatment with carbimazole. It has immediate effects on symptoms but does not alter the rate of thyroid hormone synthesis or secretion.
Exophthalmos associated with Graves’ disease usually responds poorly to treatment with antithyroid drugs, since it is caused by TSH receptor antibody. Severe thyroid eye disease can be helped by treatment with oral prednisolone if antithyroid treatment is not improving the condition.
Approximately 50% of people with Graves’ disease have a single episode that is cured by drug treatment (spontaneous remission). Those who relapse will usually do so within 6 months, and thereafter repeat relapses are common. Most are then offered definitive treatment by either a subtotal thyroidectomy (for a large goitre) or a therapeutic dose of radioactive iodine (131I).
Radioiodine can be used as first-line treatment for Graves’ disease or for relapse after antithyroid drug treatment. Radioiodine can make thyroid ophthalmopathy worse, but this can be prevented by treatment with a corticosteroid such as prednisolone for 2–3 months. Before radioiodine treatment it is often recommended that the thyrotoxicosis should be stabilised with carbimazole. This reduces the risk of exacerbation of hyperthyroidism from radiation thyroiditis immediately after isotope treatment. However, antithyroid drug treatment must be stopped 3–5 days before radioactive iodine is given or it will prevent uptake of the radioiodine by the thyroid cells. A β-adrenoceptor antagonist can be useful in this period to prevent symptomatic relapse. Carbimazole can be restarted 2–4 days after radioiodine, to cover the period of up to 8 weeks before radioiodine is fully effective. Between 10 and 20% of individuals will require a second dose of radioiodine to achieve euthyroid status. Permanent hypothyroidism can occur following radioiodine treatment. The incidence of hypothyroidism is related to the initial dose of radioactivity up to 1 year after treatment; thereafter, the risk is 2–3% annually. The theoretical increase in risk of cancer or leukaemia following radioiodine treatment has not been substantiated in clinical studies.
Surgery in Graves’ disease is used if there is a poor response to antithyroid drugs, a very large goitre, for coexisting thyroid malignancy or if the person expresses a preference for this treatment. Before surgery, carbimazole is usually used to achieve a euthyroid state. If the thyrotoxicosis is drug-resistant then oral potassium iodide can be used for up to 2 weeks before surgery to inhibit thyroxine synthesis and release and to reduce the vascularity of the hyperplastic thyroid gland. Hypothyroidism, often delayed by several months or years, is common after surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


