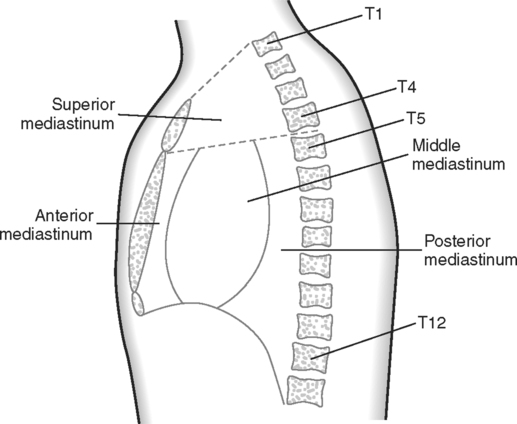
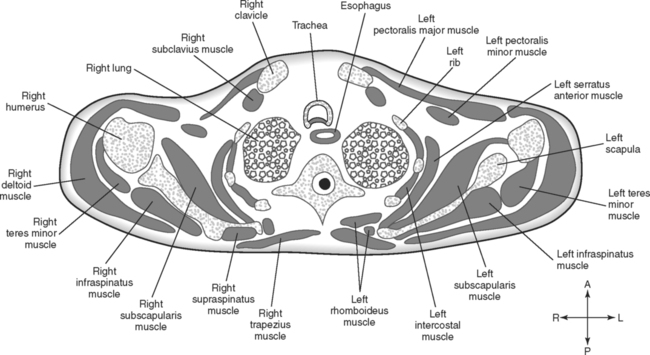
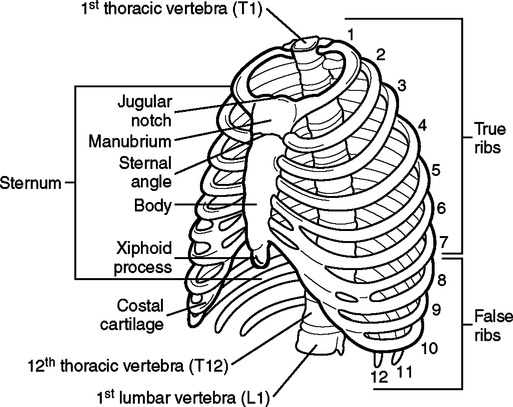
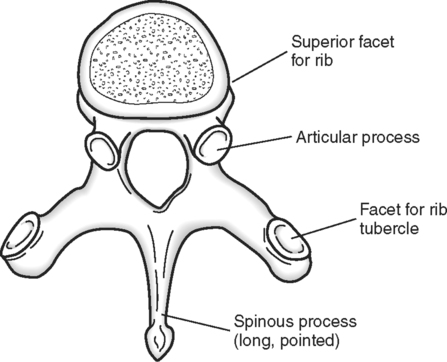
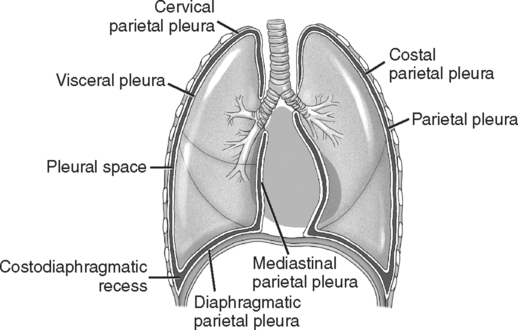
Upon completion of this chapter, the student should be able to do the following: • Identify and describe the bones that form the thoracic cage. • State the vertebral level of the jugular notch, sternal angle, and xiphisternal junction. • State the boundaries of the superior and inferior thoracic apertures. • List three muscles that form thoracic boundaries. • Identify muscles associated with the pectoral, back, and shoulder regions. • Describe the pleura and pleural cavities. • Compare the features of the right and left lungs. • List the divisions of the mediastinum and the contents of each region. • Describe the pericardial sac, pericardium, and pericardial cavity. • Describe the three layers of the heart wall. • Define and state the location of the apex, base, surfaces, and borders of the heart. • Discuss the features and relationships of the chambers and valves of the heart. • Compare the right and left coronary arteries with respect to origin, branches, location, and regions they supply. • Describe the venous drainage of the heart. • Trace the pathway of a stimulus through the conduction system of the heart. • Identify the great vessels associated with the heart by describing the location and relationships of each vessel. • Trace the flow of blood through the heart from the right atrium to the ascending aorta. • Discuss the location and relationships of the thymus, trachea, esophagus, azygos vein, and hemiazygos vein. • State the origin and location of the brachial plexus and name five nerves that emerge from the plexus. • Describe the structure of the female breast. • Name four groups of lymph nodes involved in lymphatic drainage of the breast. • Identify the skeletal components, muscles, blood vessels, and viscera of the thorax in transverse, sagittal, and coronal sections. Key Terms, Structures, and Features to Be Identified and/or Described Common carotid arteries Cricoid cartilage Internal carotid arteries Pectinate muscle R & L brachiocephalic veins R & L lungs R & L pulmonary arteries R & L subclavian arteries The skeleton of the thorax is formed by the sternum anteriorly, the 12 thoracic vertebrae posteriorly, and the ribs with their costal cartilages laterally. These bones form a thoracic cage that serves as an attachment for muscles and protects the vital viscera the cage encloses. The osseous components of the thorax are illustrated in Fig. 2-1. The posterior median skeleton of the thoracic cage is formed by the 12 thoracic vertebrae. Features of these vertebrae that are specifically related to the thorax include facets on the transverse processes and vertebral bodies for articulation with the ribs and the long spinous processes. Features of the thoracic vertebrae are illustrated in Fig. 2-2. When the vertebral column is flexed, the most prominent spinous process usually is that of the seventh cervical vertebra, although sometimes the first thoracic spinous process may be just as evident. When the arms are at the sides, a line drawn through the tip of the third thoracic spinous process indicates the level of the base of the scapular spine. The inferior angle of the scapula is at the same level as the middle of the seventh thoracic spinous process. The position of these landmarks changes when the arms are raised. Numerous muscles are attached to the skeleton of the thorax. Most of these are muscles that move the pectoral girdle or are associated with the shoulder joint. This section discusses only the muscles that form a part of the thoracic boundary and are associated with a change in the intrathoracic volume during breathing. Increasing the volume of the thoracic cavity reduces the pressure and permits inspiration. Conversely, reducing the volume increases the pressure and forces air out of the lungs during expiration. To increase intrathoracic volume, the boundaries of the thoracic cavity may increase in three different dimensions: vertically, transversely, and anteroposteriorly. Elastic recoil of the lungs and the weight of the thoracic wall primarily account for the decrease in each dimension during expiration. The muscles of the thoracic wall are illustrated in Fig. 2-3 and summarized in Table 2-1. TABLE 2-1 The diaphragm covers the thoracic outlet, forming a muscular, movable partition between the thoracic and abdominal cavities. Contraction of the diaphragm enlarges the thoracic cavity in the vertical dimension during inspiration. Because the diaphragm is visualized to a greater extent in abdominal sections than in thoracic sections, it is described in greater detail in the Chapter 3. Numerous muscles span the back and pectoral regions of the thorax but are functionally associated with the upper extremity. Many of these muscles anchor the arm to the trunk, as well as function in movement. Sections of the thorax also show the humerus and bones of the pectoral girdle. The pectoral girdle consists of the clavicle, or collar bone, anteriorly and the scapula, or shoulder blade, posteriorly. Because these skeletal and muscle components are clearly evident on thoracic sections, they are included here. (A more thorough discussion of the upper extremity and its associated articulations is presented in Chapter 7.) The pectoral region is located on the anterior thoracic wall. Four muscles are associated with this region. These muscles help attach the upper limb to the thoracic skeleton. All are associated with movements of the arm either by acting directly on the humerus or by acting on the bones of the pectoral girdle. These muscles are summarized in Table 2-2 and are illustrated in Fig. 2-4. TABLE 2-2 Muscles of the Pectoral Region The muscles of the back and shoulder region may be divided into three groups: superficial back muscles, deep back muscles, and muscles associated with the scapula. Several of these muscles are illustrated in Fig. 2-4, and they are summarized in Table 2-3. TABLE 2-3 Muscles of the Back and Shoulder Region The two pleural cavities are completely closed and separated from each other. They are lined by a serous membrane called the pleura. The pleura is essentially a continuous sheet in each cavity; however, for descriptive purposes, it is divided into the visceral layer and the parietal layer. You can visualize this as a balloon indented by your fist. The balloon is a single sheet of material, but when you stick your fist into it, you have two layers, the outside, or parietal, layer and the layer next to your hand, the visceral layer. The visceral pleura is intimately adherent to the lung, covering its entire surface and continuing deeply into its fissures. The parietal pleura lines the thoracic wall and is divided into four regions, as illustrated in Fig. 2-5. The costal parietal pleura is applied to the ribs, costal cartilages, intercostal muscles, and sternum. The diaphragmatic parietal pleura is fused with the diaphragm and is continuous with the mediastinal parietal pleura, which is adjacent to the mediastinum. The cervical parietal pleura projects into the thoracic inlet to cover the apex of the lung. The lungs and pleura occupy the lateral portions of the thoracic cavity. All other thoracic structures are crowded into a central space called the mediastinum. The mediastinum is divided into four regions, as illustrated in Fig. 2-6.
The Thorax
Anatomical Review of the Thorax
Osseous Components
Thoracic Vertebrae.
Muscular Components
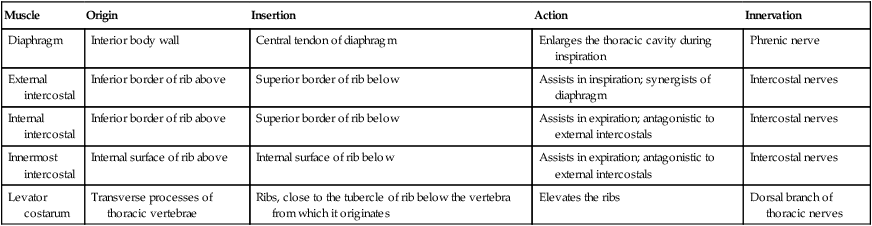
Muscles of the Thoracic Wall.
Muscle
Origin
Insertion
Action
Innervation
Diaphragm
Interior body wall
Central tendon of diaphragm
Enlarges the thoracic cavity during inspiration
Phrenic nerve
External intercostal
Inferior border of rib above
Superior border of rib below
Assists in inspiration; synergists of diaphragm
Intercostal nerves
Internal intercostal
Inferior border of rib above
Superior border of rib below
Assists in expiration; antagonistic to external intercostals
Intercostal nerves
Innermost intercostal
Internal surface of rib above
Internal surface of rib below
Assists in expiration; antagonistic to external intercostals
Intercostal nerves
Levator costarum
Transverse processes of thoracic vertebrae
Ribs, close to the tubercle of rib below the vertebra from which it originates
Elevates the ribs
Dorsal branch of thoracic nerves
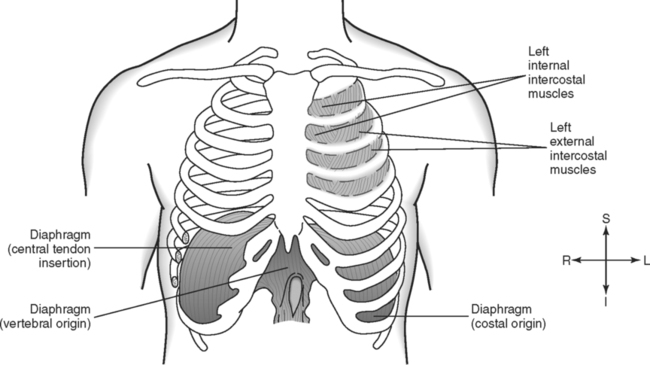
Diaphragm.
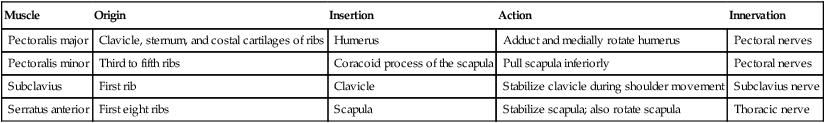
Muscles of the Pectoral Region.
Muscle
Origin
Insertion
Action
Innervation
Pectoralis major
Clavicle, sternum, and costal cartilages of ribs
Humerus
Adduct and medially rotate humerus
Pectoral nerves
Pectoralis minor
Third to fifth ribs
Coracoid process of the scapula
Pull scapula inferiorly
Pectoral nerves
Subclavius
First rib
Clavicle
Stabilize clavicle during shoulder movement
Subclavius nerve
Serratus anterior
First eight ribs
Scapula
Stabilize scapula; also rotate scapula
Thoracic nerve
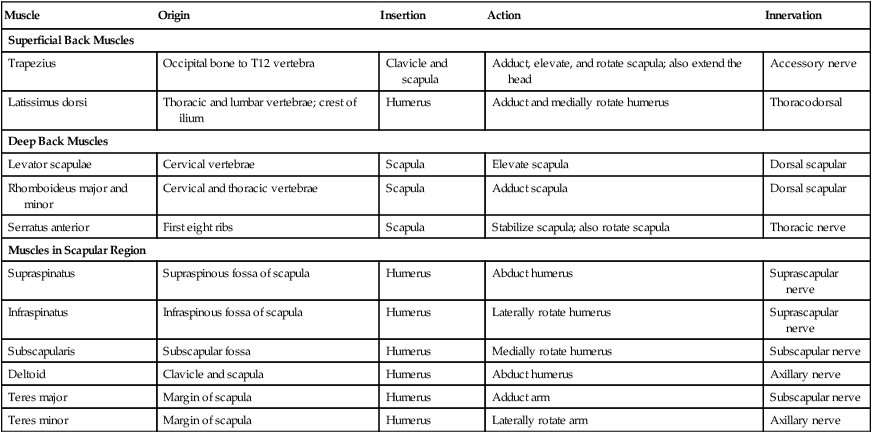
Muscles of the Back and Shoulder Region.
Muscle
Origin
Insertion
Action
Innervation
Superficial Back Muscles
Trapezius
Occipital bone to T12 vertebra
Clavicle and scapula
Adduct, elevate, and rotate scapula; also extend the head
Accessory nerve
Latissimus dorsi
Thoracic and lumbar vertebrae; crest of ilium
Humerus
Adduct and medially rotate humerus
Thoracodorsal
Deep Back Muscles
Levator scapulae
Cervical vertebrae
Scapula
Elevate scapula
Dorsal scapular
Rhomboideus major and minor
Cervical and thoracic vertebrae
Scapula
Adduct scapula
Dorsal scapular
Serratus anterior
First eight ribs
Scapula
Stabilize scapula; also rotate scapula
Thoracic nerve
Muscles in Scapular Region
Supraspinatus
Supraspinous fossa of scapula
Humerus
Abduct humerus
Suprascapular nerve
Infraspinatus
Infraspinous fossa of scapula
Humerus
Laterally rotate humerus
Suprascapular nerve
Subscapularis
Subscapular fossa
Humerus
Medially rotate humerus
Subscapular nerve
Deltoid
Clavicle and scapula
Humerus
Abduct humerus
Axillary nerve
Teres major
Margin of scapula
Humerus
Adduct arm
Subscapular nerve
Teres minor
Margin of scapula
Humerus
Laterally rotate arm
Axillary nerve
Thoracic Cavity
Pleural Cavities.
Mediastinum.