The Nutrition Transition: Global Trends in Diet, Lifestyle, and Noncommunicable Diseases1
Benjamin Caballero
1Abbreviations: BMI, body mass index; GDP, gross domestic product; GNP, gross national product; LMICs, low- and middle-income countries; QSR, quick service restaurant; SES, socioeconomic status; UN, United Nations; WHO, World Health Organization.
Food has been a critical factor for the survival of the human species since the beginning of time. For centuries, humans have struggled to secure enough food for survival, and to achieve a body size that optimized chances of survival, productivity, and reproduction. In the past century, the dramatic increase in access to dietary energy by millions of people in the developing world and the relative reduction in infectious disease burden, for the first time in history, have led to an increase in the body size of the human species that exceeds the desirable limits. Around the year 2002, a sort of milestone was reached: The number of overweight people on the planet exceeded the number of underweight people (1). Today, we confront a global epidemic of overweight and obesity, which is leading inevitably to a dramatic increase in diabetes, cardiovascular diseases, and other conditions associated with excess body mass. Furthermore, in many countries, undernutrition (underweight) coexists with overnutrition (overweight), even within the same household (2, 3). About 1 billion adults are overweight, and more than 300 million are clinically obese.
THE PERSISTENT PROBLEM OF UNDERNUTRITION
Approximately 20 million children in the world are severely undernourished, and half of them will die every year—more than 1000 per hour. The World Health Organization (WHO) estimated that more than two thirds of those deaths are preventable by simple relatively low-cost interventions (4), because the leading causes of death—diarrhea, pneumonia, and malaria—are treatable or preventable. Poverty continues to be a major underlying factor in the persistent burden of undernutrition and preventable diseases in children. Approximately half the world population lives on less than $2 per day, and 20% of these on less than $1 per day. Poverty level correlates strongly with the prevalence of underweight. The role of socioeconomic status (SES) on the nutrition transition is further discussed later.
THE GLOBAL EPIDEMIC OF OBESITY
Overweight/obesity is an important risk factor for death. It ranks fifth among leading mortality risks, and is responsible for 7% to 8% of deaths globally. Overweight has been a longstanding public health concern in developed countries, but the focus on developing countries is relatively recent. The WHO Technical Report No. 894, one of the first devoted to the “global epidemic” of obesity, was published in 2000 (5). Since then, the focus and research on global obesity, as well as on related chronic, noncommunicable disorders associated with excess weight, have expanded considerably (6).
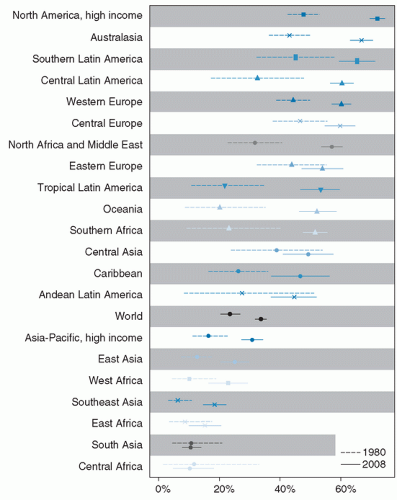
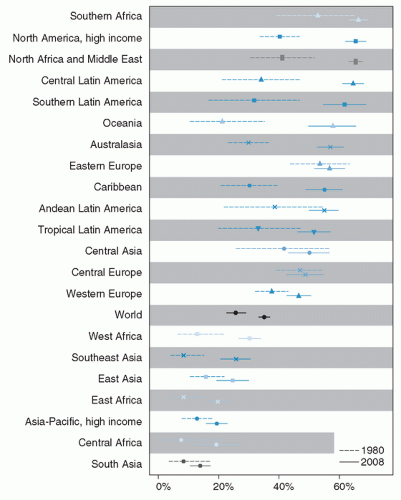
The global obesity epidemic continues its upward trend in most countries and regions. An analysis by Finucane et al (7) provided evidence of this continuing progression. Between the period evaluated, 1980 to 2008, body mass index (BMI) increased in all but eight of the 199 countries studied. Flat trends were observed in some Eastern European countries in women and in Central Africa and South Asia in men. The data also showed a wide range of mean BMI in different populations, from 19.9 in men from Congo to 35 in women from Nauru. The authors estimated that, as of 2008, there were 1.46 billion individuals in the world with excess body weight (BMI ≥25), of whom about 35% were obese (BMI >30). The data showed a moderate excess of obesity in women relative to men, but with wide
country and regional variations. Figures 109.1 and 109.2 depict the changes in prevalence of obesity between 1980 and 2008. Well-recognized caveats in interpreting combined datasets from different countries exist, particularly with the use of a single cutoff point to define overweight and obesity across regions. Nevertheless, these data provide an important assessment of trends in the obesity epidemic since 1980.
country and regional variations. Figures 109.1 and 109.2 depict the changes in prevalence of obesity between 1980 and 2008. Well-recognized caveats in interpreting combined datasets from different countries exist, particularly with the use of a single cutoff point to define overweight and obesity across regions. Nevertheless, these data provide an important assessment of trends in the obesity epidemic since 1980.
Obesity prevalence is also on the rise in young children (0 to 5 years of age). Estimates indicate that the global prevalence of overweight and obesity in this age group has increased from 4.2% in 1990 to 6.7% in 2010 (8). This is equivalent to 43 million overweight or obese children, of whom 35 million are in developing countries. This same report projected that by the year 2020 the prevalence will reach 9.1%, or approximately 60 million children.
THE NUTRITION TRANSITION
The term “transition” has been used to describe the epidemiologic transition (9), and it was applied by Popkin and others to describe trends associated with diet, food consumption, and chronic diseases that are occurring in the developing world (10, 11). This nutrition transition can be seen as part of the changes that shaped human health during the last half of the twentieth century, namely, the demographic, economic, and technologic changes that developing countries experienced during that period (12, 13). The nutrition transition has been driven by three major factors: changes in global food availability and dietary intake, urbanization, and a lifestyle characterized by low levels of physical activity. Technical advances in communications also have played an important role by facilitating the rapid and extensive dissemination of cultural preferences and lifestyle trends.
DIETARY TRENDS
Since the 1980s and 1990s, major shifts in diet quantity and composition have occurred across the world. Per capita energy availability increased markedly. In the developing world (excluding sub-Saharan Africa), this increase averaged approximately 600 kcal/day, but was as much as 1000 kcal/day in China (14). Overall, low- and middle-income countries (LMIC) have seen modest declines in consumption of cereals and pulses and an increase in animal food sources, whereas a low consumption of fruit and vegetables continues to be a concern.
Major contributors to the increase in total dietary energy intake are vegetable oils and refined carbohydrates (sugars). Projections indicate that fat and sugar consumption will continue to be the main factors driving the increased dietary energy availability (15).
Major contributors to the increase in total dietary energy intake are vegetable oils and refined carbohydrates (sugars). Projections indicate that fat and sugar consumption will continue to be the main factors driving the increased dietary energy availability (15).
The previous relationship between income and diet in poor countries led to the traditional concept that a low per capita gross national product (GNP) is associated with a heavily plant-based diet, of low energy density; this diet profile has been progressively altered by global trends in food production and marketing. Food balance sheets and other research data from developing countries (16, 17) have shown that current diets in LMIC have increasing proportions of calories derived from fat (primarily vegetable oils) and refined carbohydrates. A number of factors may explain these changes in diet composition. First, there has been an increase in worldwide availability of relatively cheap vegetable oil (18, 19). Second, cultural perceptions of diet quality, influenced by commercial advertisement, have led to the consumption of more processed food products, many containing refined sugars. A quest for variety and convenience (i.e., prepared foods) also has been cited as an important factor (20). In a model to assess the impact of urbanization, Drewnowski and Popkin predicted a substantial increase in consumption of caloric sweeteners as urbanization increases (21). The continuing expansion of the fast food market in LMICs is also of concern. More than half the revenues of the US fast food industry are obtained outside of the United States, mostly by the rapid growth of minimum service food stands (quick service restaurants [QSRs]) in LMICs (22). Another important factor determining food access and quality in developing countries is the dramatic expansion of retail food chains (supermarkets). In many LMICs, almost half the daily calories are now obtained from supermarkets, and this trend continues to grow.
In the United States, supermarkets appear to have a favorable effect on food quality, in part because they may provide more variety and quantity of produce and healthier options of processed foods (23). Thus, the concern in developed countries centers on “food deserts,” areas with no supermarkets, in which individuals purchase food in convenience stores in gas stations, or small corner stores with limited offerings. Although data from LMICs on this topic are still scarce, some evidence points to an opposite effect of supermarkets in developing countries. Data from
Guatemala suggest that supermarket use may result in more consumption of energy-dense, nutrient-poor foods (24). Additional research is needed on this topic.
Guatemala suggest that supermarket use may result in more consumption of energy-dense, nutrient-poor foods (24). Additional research is needed on this topic.
POPULATION TRENDS
Experts estimated that the 7 billionth human being was born sometime in October 2011. For thousands of years human population increased at a modest rate. In the mid-1800s, as mortality began to decline in industrialized countries, growth rates rose progressively, but remained well below 1% until the 1920s. Highest growth rates were reached in the mid-1900s, but declined thereafter, as mortality continued to fall, with fertility rates following. By the end of the twentieth century, all but 16 countries had transitioned to lower fertility rates (25). This decline in population growth in the last half of the twentieth century is a key element in the modern nutrition transition. Declining fertility is associated with lower infant mortality and improved child survival, and lower mortality and increased life expectancy result in an increased number of persons surviving to ages with higher prevalence of chronic, noncommunicable diseases. Growth projections for the next several decades predict a drastic increase in the population of persons greater than 60 years of age. This aging of the world population will undoubtedly be associated with an increase in the number of people at risk for chronic diseases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree