Chapter Twenty-Nine. The immune system
Introduction
The immune system protects us from environmental factors such as micro-organisms, irritants and abnormal cells. Pathogens such as viruses, bacteria and fungi constantly invade the body, both on its surface and internally (Male et al 2006). Larger organisms such as worms are parasitic, obtaining their food from our metabolic processes (Kendall 2007). Many micro-organisms cannot harm us if we are well but may cause death if the immune system is defective.
In developed countries, infection accounts for less than 2% of deaths. However, there are developing problems such as resistant strains of bacteria such as meticillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile (C-diff.). Also, global travel makes the transfer of deadly organisms such as the so-called bird flu more rapid.
Divisions of the immune system
The immune system recognises pathogens and mounts an immune response to eliminate them. Because there are many pathogens a wide variety of immune responses is needed and there are three lines of defence. The first two, surface barriers and the inflammatory response, are non-specific ( innate) and the third is a specific response ( acquired, adaptive) to a particular foreign protein. Innate immunity immediately protects the body from a range of substances whilst acquired immunity acts against a particular invader but must be primed by its presence and takes time to develop. The two categories of immune response are interdependent and work together to either destroy the invader or reduce its harmful effects (Fig. 29.1).
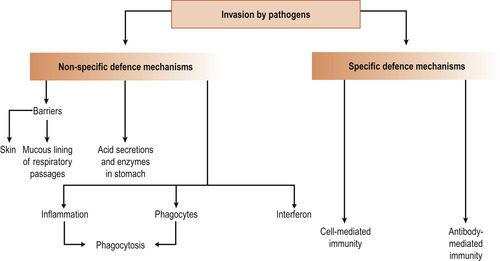 |
| Figure 29.1 Summary of specific and non-specific defence mechanisms. Non-specific mechanisms prevent entry of many pathogens and act rapidly to destroy those that manage to cross the barriers. Specific defence mechanisms take longer to mobilise but they are highly effective in destroying invaders. (From Montague S E, Watson R, Herbert R A 2005, with kind permission of Elsevier.) |
Cells of the immune system
Immune responses are mediate by a variety of cells and the soluble molecules they secrete. Leucocytes (white blood cells, WBCs) are protective against bacteria, viruses, parasites, toxins and tumour cells. There are normally about 4000–11 000 per cubic mm (4–11 × 10 9/L). Most leucocytes are in the tissues and there is a wide variation in the blood count as cells enter and leave the circulation from hour to hour. All leucocytes are produced in the bone marrow from haemopoietic stem cells (Male et al 2006).
Types of leucocyte
Several types of leucocyte are distinguished by their shape, appearance and function. Granulocytes (polymorphonuclear leucocytes) have granules in their cytoplasm which contain substances that fight infection. They are 10–14 μm in diameter and have a lobed nucleus. They are divided into three groups by the size of their granules: neutrophils, eosinophils and basophils. All are phagocytic, engulfing and destroying foreign proteins. Agranulocytes, which include lymphocytes and monocytes, do not contain granules. Natural killer cells (NK cells) are a specialised type of large, granular lymphocyte.
Granulocytes
1. Neutrophils contain granules that stain violet because they take up both acidic red dyes and basic blue dyes. They account for more than 50% of granulocytes and have the most lobular nuclei. Neutrophils migrate to inflammation sites. They are short-lived cells that engulf foreign material such as bacteria, destroy it and die.
2. Eosinophils have large granules that stain red with acidic dyes. They make up 1–4% of leucocytes. They attack parasitic worms by surrounding them and releasing granular enzymes onto the parasite’s surface to digest it from the outside. Eosinophils also deal with allergy by destroying antigen–antibody complexes.
3. Basophils have large granules that take up a basic dye and stain blue-black. They account for only 0.5% of white cells. Their granules contain histamine, an inflammatory substance that acts as a vasodilator and draws other white cells to an inflammation site. Mast cells are similar to basophils and are present in connective tissue. Both cell types release histamine when they bind to immunoglobulin E.
The production of granulocytes
The process of granulopoeisis takes about 14 days but is considerably reduced if cells are needed. There is progressive condensation and lobulation of the nucleus, loss of organelles and development of granules in the cytoplasm. Within 7 h of reaching the circulation, half of the granulocytes will have migrated into tissue and will not return. They survive about 5 days and are eliminated in faeces and respiratory secretions and form pus at infection sites. For every granulocyte in blood there are 50 in bone marrow.
Natural killer (NK) cells are present in blood and lymph and account for 15% of blood lymphocytes. Unlike other lymphocytes which only react to specific virus-infected or tumour cells, NK cells react against cells which do not express major histocompatibility complex (MHC) class 1 molecules (see below), an important factor in the immunology of pregnancy.
Agranulocytes
Lymphocytes are round cells with large round nuclei and are the second most common type of leucocyte. Large numbers exist in the body, mostly in lymphoid tissue. They recirculate between blood and lymph and are subdivided into small and large lymphocytes. There are two types of lymphocytes: T and B lymphocytes. Some lymphocytes leave the bone marrow and migrate to the thymus gland where they will become T cells. They are selected so that they will not attack self-antigens present on the surface of an individual’s cells. B cells were first identified in the bursa of Fabricius, a pocket of lymphoid tissue associated with the digestive tract in birds. T cells are involved in cell-mediated immunity and account for 80% of the lymphocytes found in blood. B cells are involved in humoral immunity and produce antibodies.
Monocytes are large cells produced in the bone marrow from myeloid progenitors. Mature cells spend about 30 h in the blood and then migrate to the tissues where they develop into phagocytic macrophages (giant eaters). Macrophages regulate the immune response by presenting antigens to activate B and T cells.
Non-specific responses
These can be divided into surface barriers, such as skin and mucous membranes, and cellular and chemical defences.
Surface barriers include:
• A thickly keratinised unbroken skin.
• Intact mucous membranes lining the organs.
• Acidic secretions, such as in the vagina, gastric juices and urine.
• Sticky mucus to trap organisms.
• Ciliated cells that sweep particles towards the outside.
• Lysozyme, an enzyme that destroys bacteria, in saliva and tears.
Phagocytes
If the intact surfaces are breached, cellular and chemical non-specific mechanisms are triggered. In most cases, phagocytic cells (Fig. 29.2) are involved. These are amoeba-like and travel through tissue spaces in search of invading organisms or other debris to engulf and destroy.
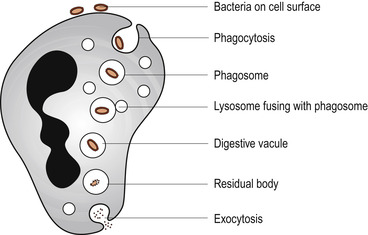 |
| Figure 29.2 Diagram of a neutrophil undergoing phagocytosis. (From Montague S E, Watson R, Herbert R A 2005, with kind permission of Elsevier.) |
Macrophages are the main phagocytic cells but neutrophils become phagocytic if an infection is present. Macrophages are long-lived but neutrophils are destroyed during phagocytosis. Both cells destroy microbes by producing free radicals. Neutrophils also produce antibiotic-like chemicals called defensins. Complement proteins and antibodies coat foreign proteins and provide binding sites for phagocyte attachment, a process called opsonisation.
Inflammation
Inflammation is a localised response when there is a tissue injury due to trauma or invasion by micro-organisms. The inflammatory response prevents the spread of damaging substances to nearby tissues, disposes of cell debris and pathogens and allows repair to begin. There are four cardinal signs of inflammation: heat, redness, swelling and pain. Depending on the site and type of tissue damage, chemicals are released into the extracellular fluid by injured cells, phagocytes, lymphocytes, mast cells and blood proteins. Four major plasma enzyme systems are involved in the control of inflammation (Male et al 2006):
1. The clotting system.
2. The fibrinolytic system.
3. The kinin system.
4. The complement system.
The most important molecules are histamine, kinins, prostaglandins, complement and lymphokines. They induce vasodilation of localised small blood vessels, causing heat and redness. Capillary wall permeability increases, allowing a fluid exudate containing clotting factors and antibodies to seep into the tissue spaces and cause oedema and swelling. Clotting proteins form a fibrin mesh which limits the spread of harmful agents and acts as scaffolding for tissue repair. Pain results from pressure on local nerve endings, release of bacterial toxins, lack of cellular nutrition and the effects of prostaglandins and kinins. Loss of function may occur, forcing the person to rest the injured part to aid healing.
The damaged area is first invaded by phagocytes. Rapid release of neutrophils by the bone marrow is caused by leucocyte-inducing factors so that four times as many neutrophils may be in the blood stream after a few hours. These cells are attracted to the injury site by chemicals called chemotactic agents. At the site they cling on to capillary walls ( margination or pavementing) and squeeze through capillary walls ( diapedesis) to the site where they devour bacteria, toxins and dead tissue. Monocytes now enter the tissue, swell and mature into macrophages.
If the infection is severe, pus—a mixture of dead neutrophils, living and dead pathogens and damaged tissue cells—is produced. If this becomes walled off by collagen fibres, an abscess forms. Some bacteria like the tuberculosis bacillus are resistant to digestion by macrophages because of their waxy outer coat and remain alive inside the macrophage. Infectious granulomas develop which have a central core of infected macrophages surrounded by uninfected macrophages and an outer fibrous capsule. The person only becomes ill if his resistance to infection is reduced when the bacteria may break out and cause disease.
Fever
Fever is an elevation of the body temperature in response to chemicals called pyrogens such as the interleukins. High fevers are dangerous because they inactivate enzymes and disrupt cellular metabolic processes but mild to moderate fevers are helpful in stimulating the immune system (Kendall 2007) and speeding up both metabolic rate of tissue and defensive actions to aid repair. Antibacterial responses include the sequestering of zinc and iron in the liver and spleen to prevent their use as nutrients by bacteria.
Complement
Complement is a system of about 30 antimicrobial plasma proteins constituting about 10% of total plasma proteins. They normally circulate in the blood in an inactive state. In evolutionary terms they are very old and developed long before the adaptive immune system (Male et al 2006). Their functions are:
• Control of inflammatory reactions.
• Chemotaxis.
• Clearance of immune complexes.
• Cellular inactivation.
• Antimicrobial defence.
• Development of antibody responses.
Important complement proteins are C1–C9. Activation of the complement system releases chemical mediators that increase most parts of the inflammatory response and enhance the specific immune system. Complement can be activated by three pathways, which activate C3, causing it to split into two fragments, C3a and C3b:
1. The classical pathway (Fig. 29.3) is activated by the formation of antigen–antibody complexes.
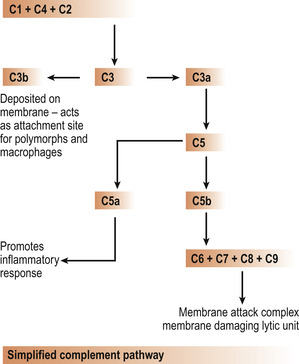 |
| Figure 29.3 Simplified complement pathway. (From Montague S E, Watson R, Herbert R A 2005, with kind permission of Elsevier.) |
2. The lectin pathway is similar but activated by bacterial carbohydrates.
3. The evolutionary older alternative pathway provides non-specific immunity and is triggered by the presence of microbial pathogens.
An orderly cascade of complement protein activation occurs and C3b binds to the target cell’s surface, resulting in the insertion of a group of complement proteins called the membrane attack complex (MAC) into the bacterial cell wall, punching a hole and allowing solutes to leak from the cell which destroys it (Male et al 2006).
Specific defence: the immune system
Tissues of the lymphatic system
The lymphatic system consists of two parts: a network of lymphatic vessels and lymphoid organs and tissues throughout the body. The organs and tissues are divided into primary lymphoid organs such as the bone marrow and thymus gland where B and T cells mature and the peripheral lymphoid system where they spend most of their active lives (Fig. 29.4). The peripheral lymphoid system includes encapsulated organs such as the spleen, tonsils and lymph nodes. Uncapsulated lymphoid tissue is found associated with mucosal surfaces in the gut, lungs and urogenital tract.
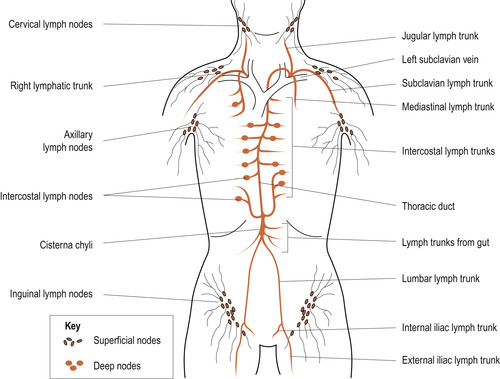 |
| Figure 29.4 General arrangement of the lymphatic system. (From Montague S E, Watson R, Herbert R A 2005, with kind permission of Elsevier.) |
Lymph nodes
The immune response takes place in the lymphatic system. The kidney-shaped lymph nodes (Fig. 29.5) are about 2–10 mm in diameter and filter lymph. They consist of a radial network of fibres in which lymphocytes are embedded. The inner medulla contains macrophages, T cells, B cells and plasma cells. B cells are concentrated in primary and secondary follicles in the cortex. Cells at the centre of a follicle divide while those at the periphery produce antibodies. T cells are found in the paracortical area.
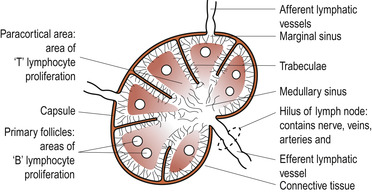 |
Figure 29.5
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|