Learning Outcomes
After completing this chapter, you will be able to
 Identify the major structures of each of the body systems presented.
Identify the major structures of each of the body systems presented.
 Describe the major functions of each of the body systems presented.
Describe the major functions of each of the body systems presented.
 Describe common diseases and disorders that can develop when something goes wrong in a body system.
Describe common diseases and disorders that can develop when something goes wrong in a body system.
 Recognize the role of drug therapy in the common diseases and disorders of the body systems.
Recognize the role of drug therapy in the common diseases and disorders of the body systems.
Key Terms
| anatomy | The study of body structure. |
| antigen | A substance that is capable of causing the production of an antibody. |
| autoimmunity | A misdirected immune response that happens when the body attacks itself. |
| diastole | When the heart muscle is relaxed and the chambers are filling with blood; the pressure is at the lowest point in a normal heart. |
| digestion | The process whereby ingested food is broken up into smaller molecules by chemical or mechanical means. |
| endocrine | The internal secretion of substances into the systemic circulation (bloodstream). |
| endocrine glands | Glands that have no ducts; their secretions are absorbed directly into the blood. |
| gonads | Reproductive organs; testes in the male, and ovaries in the female. Gonads function to produce reproductive cells and sex hormones. |
Section III: The Dermatologic System |
|
This chapter provides an overview of the structure and function of the human body. By organizing the information by body system, we can become familiar with the major parts of each system (i.e., the structure) and what they do (i.e., the function), as well as what can go wrong (which results in diseases and disorders). You’ll find that the organization of this chapter is similar to that of Chapter 10: Drug Classifications and Pharmacological Actions, wherein detailed information about the drugs used to treat common diseases and disorders is explained.
Overview of the Human Body
In the human body the simplest functioning unit is the cell, which is the basic unit of life. There are many different types of cells in the body, and when cells with the same function or origin are organized in groups, the formation of tissue results. In turn, combinations of tissues form organs, such as the heart, lungs, brain, and skin. Organs within the body are then connected into highly organized body systems that work together within the body.
Each body system is linked to function as a single working unit to ensure that all body functions are in balance, which is referred to as homeostasis.
Anatomy is the study of body structure; the study of the collective functions and processes of the body systems is known as physiology. It is important to remember that none of these body systems work alone; in order to maintain a stable internal environment, the proper functioning of each system requires and depends upon the proper functioning of one or more of the other body systems. When the normal physiological function of a body system becomes abnormal and a disease state occurs, this is known as pathophysiology.
The Nervous System
Overview of Structure and Function
The anatomy (structure) of the nervous system consists of the brain, spinal cord, and a system of nerve cells (neurons) that connect to organs and tissues throughout the body (see figure 9–1). There are two major parts to the nervous system: the central nervous system and the peripheral nervous system. The central nervous system consists of the brain and the spinal cord, whereas the peripheral nervous system consists of a network of nerves that exit from the spinal cord and extend throughout the entire body.
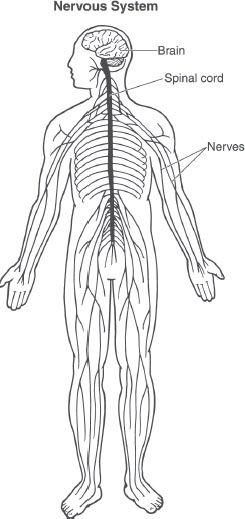
Figure 9–1. The nervous system. The nervous system is comprised of the brain, the spinal cord, and an extensive network of nerves. The system controls many activities of the body by transmitting electrical signals via neurons and the release of chemical signals known as neurotransmitters.
Further divisions occur within the peripheral nervous system. The afferent division brings information, such as temperature, from the external environment, as well as information on the status of internal organs, for example heart rate, to the brain. The efferent division delivers signals from the brain to the organs and tissues of the body. The efferent division is further subdivided into the somatic and autonomic nervous systems. The autonomic nervous system is further subdivided into the sympathetic and parasympathetic divisions. Each of the nervous systems in the efferent division is under control of the central nervous system.
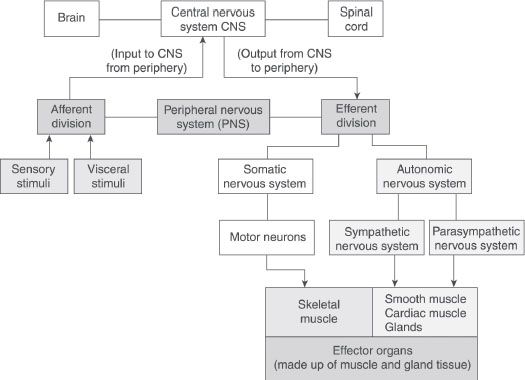
Figure 9–2. The nervous system is a highly organized network. The two major divisions are the central nervous system, which is comprised of the brain and spinal cord, and the peripheral nervous system, which is comprised of a network of nerves outside the spinal cord. The peripheral nervous system is divided into the afferent division, which carries sensory information to the brain, and the efferent division, which carries information from the brain to organs. The efferent division is divided into the autonomic and somatic nervous systems.
The somatic nervous system transmits signals to the skeletal muscles of the body, which are under voluntary control (see figure 9–2). In contrast, the autonomic nervous system communicates with many different organs, for example the heart, muscles, and glands, and it’s not under voluntary control—rather, it is controlled automatically by the brain. Both the sympathetic and parasympathetic divisions have, in general, opposing actions in the body. The sympathetic nervous system works when the body is under stress and is best described as that which causes the flight-or-fight response, whereas the parasympathetic system functions when the body is at rest. The actions of the peripheral nervous system are possible because each division releases special chemical messengers called neurotransmitters, which bind to special proteins (receptors) in organs and tissues. For example, the parasympathetic division uses acetylcholine as its chemical messenger and is sometimes referred to as a parasympathetic-cholinergic system. The sympathetic division uses norepinephrine as its chemical messenger and is known as the sympathetic-adrenergic system. All of the divisions of the peripheral nervous system and their actions, whether initiated voluntarily or automatically, are under control of the central nervous system.
 The nervous system is the major communication system in the body. It receives signals from organs and transmits them to different organs in order to regulate their activities.
The nervous system is the major communication system in the body. It receives signals from organs and transmits them to different organs in order to regulate their activities.
Communication by the nervous system is rapid, and changes in the body can take place quickly. For example, the brain may receive information from special sensors in the skin indicating that the temperature of the skin is too hot. Consequently, the brain transmits a signal to blood vessels near the surface of the skin, informing them to dilate, causing heat to be lost and, as a result, the skin cools. In addition to regulating everyday functions, the central nervous system is the area where information is stored and complex functions are regulated and controlled (for example, forming and storing memories, learning, feeling emotions, feeling motivation, and sleep).
The autonomic (involuntary) nervous system (ANS) is responsible for regulating the internal organs of the body, such as sweat glands, smooth muscle, heart, lungs, eyes, kidneys, and sexual organs. For example, the brain may receive information that the heart is beating too rapidly; it interprets this information and consequently directs the nerve cells of the autonomic nervous system to transmit signals to the heart to slow its rate through the parasympathetic division of the ANS. In contrast, the somatic nervous system, via signaling by the central nervous system, is solely responsible for regulating the contractions of the skeletal muscle.
The ability of the central and peripheral nervous systems to communicate with and regulate the function of organs in the body is possible through the release of neurotransmitters. These messengers are produced and stored in the nerve cells; they are released only when an appropriate signal is transmitted (see figure 9–3).
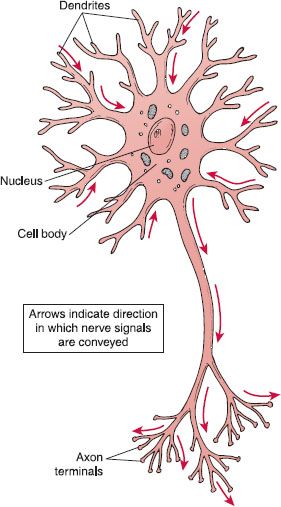
Figure 9–3. The neuron. The neuron is the major cell of the nervous system and is important in communication. It communicates by transmitting electrical signals by way of its axon and releasing chemical messengers from the axon terminal to organs.
Common Diseases and Disorders
Many problems can occur when the communication processes within the nervous system break down or are disrupted. Because many of these conditions are chronic, the technician should expect to see patients returning for refills on a routine basis.
Seizure Disorders. A seizure is a brief, strong surge of electrical activity that affects part of the brain. It can last anywhere between a few seconds and a few minutes; when a seizure occurs, the individual may experience multiple symptoms such as blank staring, strange sensations, confusion, erratic muscle movements, and loss of consciousness. There are many different types of seizures; epilepsy is a medical condition characterized by recurrent seizures. Many causes have been proposed, but it is believed that an imbalance between the brain neurotransmitters GABA and acetylcholine precipitates seizures. Antiepileptic drugs are used to correct the imbalance in the brain’s electrical activity.
Parkinson Disease. A condition in which the nerve cells in the brain that control motor function begin to degenerate and gradually lose their ability to release the neurotransmitter dopamine. This leads to an imbalance between dopamine and acetylcholine. The symptoms include difficulty with initiating and controlling the process of movement, for example, a stooped, slow, stiff, and shuffling gait. Muscle tremors at rest are common. Drug therapy for Parkinson disease focuses on restoring the balance between dopamine and acetylcholine.
Alzheimer Disease. A progressive, degenerative neurological disorder in which brain tissue, in specific areas of the brain, begins to shrink and nerve cells are lost. Abnormal tissue formations are present in the brains of people with the disease. The primary nerve cells that are lost are those that produce the neurotransmitter acetylcholine.
Eventually, the condition leads to impairments in memory, thinking, reasoning, and the ability to communicate. These symptoms slowly become more pronounced over time. Other accompanying conditions include depression and paranoia. Drug treatment includes the use of cholinesterase inhibitors, which prevent the breakdown of acetylcholine.
Multiple Sclerosis. In the central nervous system (CNS), the neurons that comprise the somatic nervous system are covered with a fatty substance called myelin. This substance facilitates the correct conduction of electrical activity from the CNS to the skeletal muscle, and thus allows for coordinated voluntary muscle movement. In multiple sclerosis (MS), this myelin sheath is broken down, lesions appear on the nerves, and multiple symptoms develop—for example, speech and swallowing difficulty occurs, muscle weakness develops, balance and gait become affected, and eye muscles become paralyzed. Numbness and tingling in the extremities also occurs. The lesions in the nerves are thought to be the result of an inflammatory response triggered by the immune system in genetically susceptible individuals. Drug treatment is focused on preventing exacerbations and on treating the symptoms.
Pain. There are many forms of pain. Pain can occur in the skin; in the body structures, such as joints, tendons, and muscles; or in the organs or the brain itself when an individual experiences a headache or a migraine. When it involves the nerves, it is called neuropathic pain. It can also last for varying lengths of time. For example, acute pain can last for six months or less. In contrast, chronic pain lasts for months to years and may be accompanied by other symptoms, such as sleep problems, lack of appetite, and depression. Pain is perceived by specialized receptors in the body that transmit signals via neurotransmitters and specialized pain pathways in the spinal cord to specialized areas of the brain. The brain in turn, through a complex system of processes, releases natural opioids to dampen the perception of pain. Drugs known as analgesics are used to treat pain by blocking the transmission of pain impulses.
Mood Disorders. A mood disorder is a type of mental illness involving a disturbance of mood. The two most common mood disorders are depression and bipolar disorder, also known as manic-depressive disorder. Depression is characterized by a loss of interest in pleasurable activities; depressed mood; lack of energy; problems with sleeping; changes in diet (loss of appetite or overeating); difficulty concentrating; feelings of guilt, worthlessness, or helplessness; irritability or restlessness; and suicidal thoughts. Research suggests that one of the causes of depression is an imbalance of the specific neurotransmitters serotonin and norepinephrine, which are involved in nerve transmission within the brain. Antidepressant drugs work by increasing the levels of these neurotransmitters. Bipolar disorder is characterized by extreme mood swings; patients cycle between an agitated or overexcited (manic) state and depression. Treatment is focused on treating the manic and depressed states, as well as preventing the mood swings.
Anxiety Disorders. Anxiety is described as a feeling of being powerless and unable to cope with stressful events. In anxiety disorders, worrying is excessive and out of proportion to the situation so that it interferes with daily functioning. There are several types of anxiety disorders including generalized anxiety disorder, panic disorder, social anxiety disorder, and obsessive-compulsive disorder (OCD). The exact mechanism that causes anxiety disorders is unknown, but it is believed that a number of factors contribute to it, including environmental, genetic, and chemical. Pharmacologic treatment involves drugs that correct the imbalance of neurotransmitters in the brain.
Psychotic Disorders. Psychosis is a mental disorder in which a person’s capacity to recognize reality is distorted. Schizophrenia is one type of psychosis. It is a chronic, disabling disorder that alters the way an individual thinks, behaves, expresses emotions, perceives reality, and interacts with people. Common symptoms include hallucinations (hearing or seeing things that are not real) and delusions (fixed beliefs that are false).
The cause of schizophrenia is unclear, but several factors are believed to be involved: heredity (genetics), an imbalance of the neurotransmitter dopamine in the brain, and environmental factors. Antipsychotic drugs are used to control schizophrenia.
Attention Deficit Hyperactivity Disorder (ADHD).
A condition that is characterized by difficulty staying focused and paying attention as well as hyperactivity. It is most commonly seen in childhood, but may continue into adolescence and adulthood. The cause of the disorder is unknown, but it may be due to genetics, environmental factors, or a deficiency of the neurotransmitters norepinephrine and dopamine. Treatment consists of behavioral modification and drugs such as stimulants.
Myasthenia Gravis. A chronic neuromuscular disease in which communication between the somatic nervous system and the muscles is disrupted. Special proteins, called receptors, that are found in the skeletal muscle are destroyed by the body’s own defense systems, and the neurotransmitter acetylcholine can no longer function to initiate contraction of the muscle. The symptoms are muscle weakness; difficulty speaking, swallowing, and breathing; extreme fatigue; and drooping eyelids. Drug treatment includes the use of acetylcholinesterase inhibitors, drugs that block the enzyme that breaks down acetylcholine.
The Cardiovascular System
Overview of Structure and Function
The cardiovascular system is comprised of the heart, blood vessels called arteries, capillaries and veins, and the blood (see figure 9–4). Blood is a fluid that flows throughout the body and contains blood cells. Blood is a mixture of plasma and cells such as platelets and red and white blood cells (see figure 9–5). The red blood cells (erythrocytes) are responsible for transporting oxygen to, and carbon dioxide away, from the cells of body tissues. Specialized cells, known as white blood cells (leukocytes), are also found in blood, and they help the body fight against invading microorganisms. Blood is also responsible for carrying nutrients to cells, and breaking down products away from them. Blood vessels function to transport blood throughout the body. The heart is a strong muscular organ that pumps blood through the blood vessels to all organs and tissues of the body.
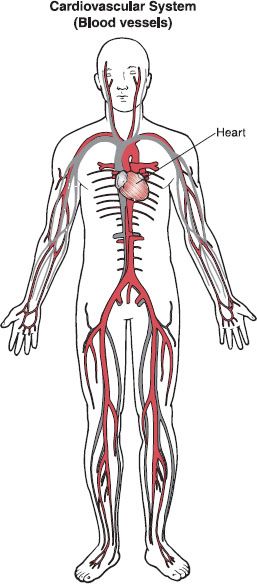
Figure 9–4. The cardiovascular system. The cardiovascular system is comprised of the heart and an extensive system of arteries and veins that transports blood, nutrients, and gases to and from organs. In general, arteries carry blood rich in oxygen away from the heart, except the pulmonary artery, which carries blood low in oxygen to the lungs. In general, veins carry blood low in oxygen to the heart, except the pulmonary vein, which carries oxygenated blood from the lungs.
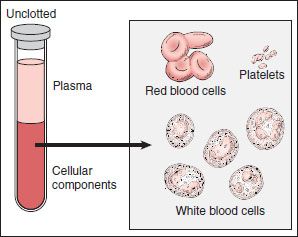
Figure 9–5. Components of blood. Cellular components found in the blood.
The heart is a fist-sized, hollow muscular organ, located in the center of the chest (thoracic) cavity between the lungs and behind the breast bone (sternum). In the chest cavity, the bottom (apex) of the heart is tilted toward the left side of the body (see figure 9–6A). Surrounding the heart is a protective covering (the pericardium), which is attached to the chest wall. Beneath the covering is the outside layer of the heart, which contains the blood vessels of the heart (coronary arteries), nerve fibers, and fat. Underneath this is the middle layer of the heart, which consists of specialized muscle cells (the myocardium) that make up the majority of the heart tissue. This muscular tissue is responsible for contracting the heart in response to nerve signals from the autonomic nervous system. The inside of the heart (and its structures) is lined with a special membrane (the endocardium), which allows for the smooth flow of blood. Throughout the heart muscle is a fibrous network of special connective tissue, which adds structure to the heart.
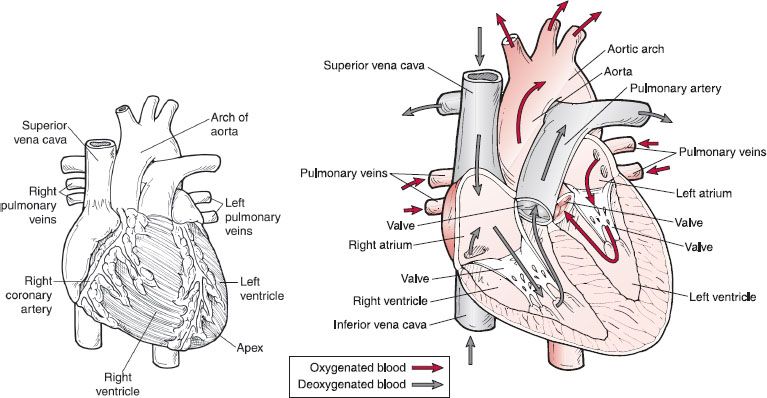
Figure 9–6. A & B. The anatomy of the heart. (A) The heart has its own blood vessels, the coronary artery and veins, which supply blood to and from the heart. (B) The structure is divided into four chambers. The upper chambers are called atria and the lower chambers are called ventricles. On the right side of the heart, the superior and inferior vena cava enter the right atrium, and the pulmonary artery leaves the right ventricle. On the left side of the heart, the left and right pulmonary veins enter the left atrium, and the aorta leaves the left ventricle.
The heart is separated into four chambers. Two upper chambers are called the atria, which are found on the left and right side of the heart; below them are the two ventricles. The right and left sides of the heart are separated into two functional pumps—the right atria and the right ventricle function together as a low-pressure pump that pumps blood into the lungs, and the left atria and left ventricle work as a high-pressure pump responsible for pumping blood throughout the body.
Blood is brought to and away from the heart by blood vessels. Veins deliver blood to the right and left atria of the heart. These veins are called the superior and inferior vena cava when they come into the right atrium, and they are called pulmonary veins when they enter the left atrium. Arteries take blood away from the heart and they exit from both ventricles: the pulmonary artery exits from the right ventricle, and the aorta exits from the left ventricle.
The heart has four valves that prevent backflow and ensure that blood travels in one direction as it flows through the organ. Two valves are between the atria and the ventricles on each side of the heart, and the other two are between the ventricles and the arteries: one between the left ventricle and the aorta and the other between the right ventricle and the pulmonary artery. When valves don’t work properly, the heart can’t pump blood efficiently.
The heart also has a conduction system of nerve pathways that respond to messages from the autonomic nervous system. The conduction system ensures that the heart muscles contract at a controlled rate in a regular rhythm.
The cardiovascular system functions to pump oxygenated blood (high in oxygen, low in carbon dioxide) to every part of the body, and it transports deoxygenated blood (low in oxygen, high in carbon dioxide) from the cells (see figure 9–6B). Blood that is low in oxygen enters the right atrium from the superior and inferior vena cava and flows through the valves separating the two chambers into the right ventricle; from there, it is pumped through the pulmonary veins into the right and left lungs. In the lungs, carbon dioxide is exchanged for oxygen (see figure 9–7). The oxygen-rich blood then returns to the left atrium, and flows through the valve into the left ventricle where it is pumped throughout the body to organs and tissues via a network of blood vessels known as arteries, which branch into smaller vessels called arterioles. Eventually they branch into tiny, thin-walled vessels called capillaries. At the capillary level, nutrients, hormones, oxygen, and drugs are delivered to cells of all organs and tissue, and waste products and carbon dioxide are transported away by venules and veins back to the right side of the heart.
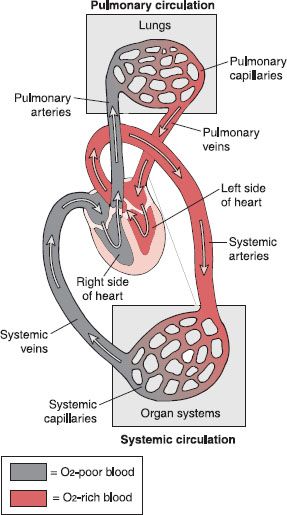
Figure 9–7. How blood flows through the circulatory system. There are two major divisions that transport blood throughout the body. In the pulmonary circulation, blood is pumped between the heart and the lungs to carry out gas exchanges. In the systemic circulation, blood is pumped between the heart and the organs and tissues of the upper and lower body.
The cardiovascular system maintains blood pressure. Flow of blood through the chambers of the heart is pumped in a continuous and repetitive cycle. The two atria contract to push blood into their respective ventricles. Then the two ventricles contract to pump the blood out of the heart. As each set of chambers is contracting (systole), the other set of chambers is relaxing (diastole). Diastole allows the chamber to refill with blood. During this cardiac cycle, the pressure in the heart rises and falls. When the ventricles of the heart contract, and consequently eject blood from the heart, the pressure in the arteries rises. This creates the systolic blood pressure. Conversely, when the ventricles are relaxed and filling with blood, the pressure falls. This creates the diastolic blood pressure. The pressure changes can be measured by a sphygmomanometer, and these two measurements are an indication of blood pressure. Figure 9–8 illustrates the technique for measuring blood pressure.
 Normal systolic blood pressure in adults is less than 120 millimeters of mercury (mmHg). Normal diastolic blood pressure in adults is less than 80 mmHg. Blood pressure is written as systolic over diastolic pressure: 120/80
Normal systolic blood pressure in adults is less than 120 millimeters of mercury (mmHg). Normal diastolic blood pressure in adults is less than 80 mmHg. Blood pressure is written as systolic over diastolic pressure: 120/80
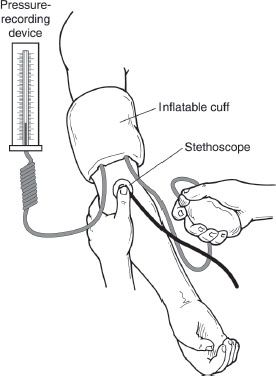
Figure 9–8. The sphygmomanometer. This instrument accurately measures arterial blood pressure. The inflatable cuff is placed over the brachial artery and the pressure in the cuff is varied to determine systolic and diastolic readings of blood pressure.
The heart contains specialized cells, called pacemaker cells, which generate electrical signals that trigger contraction of the heart and set the heart rhythm. The electrical activity of the heart can be traced using a test called an electrocardiogram (ECG or EKG). When the electrical activity of the heart is abnormal, a condition known as an arrhythmia develops. Drugs can be used to return the abnormal electrical activity to normal. In addition, the rate and force with which the heart pumps blood is regulated by the two divisions of the autonomic nervous system: the sympathetic and parasympathetic divisions. The sympathetic division increases the heart rate and the force with which the heart contracts. In contrast, the parasympathetic division slows the heart rate. Alteration of the rate and force of contraction of the heart can also affect blood pressure. The heart, in conjunction with the ability of arterioles to contract and dilate, can further alter blood pressure in the short term. Long-term control of blood pressure is also controlled by the kidney through its ability to alter blood volume.
Common Diseases and Disorders
When the regulation of the cardiovascular system is disrupted, a number of clinical problems can occur. Some examples are described below.
Coronary Artery Disease. This disease is caused when the blood vessels that supply the heart with oxygen become narrowed as the result of atherosclerosis, caused by fatty deposits (plaque) in the inside of blood vessels. This deprives the heart muscle of oxygen and can lead to a myocardial infarction (heart attack) or an abnormal heart rhythm (arrhythmia).
Stroke. Also known as cerebrovascular accidents (CVAs), strokes occur when there is an acute decrease or stoppage of blood flow to a part of the brain. The cause of a stroke can be a blood clot, which blocks the flow of blood in the vessels (ischemic stroke) or when a blood vessel ruptures, preventing blood flow to the brain (hemorrhagic stroke). The following conditions can lead to the development of a stroke: atrial fibrillation, atherosclerosis, an aneurysm (a weakness in the wall of a blood vessel), and high blood pressure. It is important to recognize and treat a stroke right away to prevent and/or minimize permanent changes in speech, language, vision, and memory.
Heart Failure. Also called chronic or congestive heart failure (CHF), heart failure occurs when the heart cannot eject adequate blood from the ventricles of the heart. One or both sides of the heart can be affected. If this occurs in the left side of the heart, sufficient oxygenated blood cannot be pumped around the body, and the individual shows symptoms of tiredness, shortness of breath, lower extremity swelling, and an increased heart rate (pulse). Fluid can build up in the lungs, which decreases the exchange of gases in the lungs, and, consequently, shortness of breath occurs. Heart failure is most commonly caused by a heart attack, high blood pressure, coronary artery disease, abnormal heart valves, and heart defects. Treatment is chronic and aimed at lessening the symptoms of heart failure and preventing further damage. It includes lifestyle changes, medications, and surgery in some cases.
Hypertension. Hypertension occurs when the normal regulation of blood pressure is disrupted and the diastolic pressure remains chronically elevated—over 90 mmHg— and is accompanied by an increased systolic pressure of over 140 mm Hg. Uncontrolled blood pressure increases the risk for stroke, heart attack, heart failure, and kidney and retinal damage. Treatment is chronic and involves lifestyle changes as well as anti-hypertensive medications.
RX for Success
A healthy lifestyle is critical to preventing heart disease and stroke, and includes activities such as quitting smoking, maintaining a healthy weight, practicing good nutrition, and exercising.
Venous Thromboembolism. In this condition, a clot forms in the veins of the body, for example, in the legs. Small portions of the clot can break away and travel to the lungs, causing a pulmonary (lung) embolism. This condition requires urgent treatment with anti-clotting drugs (anticoagulants).
Arrhythmias/Dysrhythmias. Abnormal rhythms of the heart. Some can cause the heart to beat too slowly (bradycardia) or too rapidly (tachycardia), while others produce abnormal electrical activity. Common arrhythmias originating in the atria include atrial fibrillation and atrial flutter. Premature ventricular contractions (PVCs), ventricular tachycardia, and ventricular fibrillation originate in the ventricles. Symptoms include dizziness, fatigue, and palpitation (forcible and rapid heartbeats). Drug treatment is usually chronic and is aimed at controlling the heart rate and maintaining a normal rhythm.
The Respiratory System
Overview of Structure and Function
The respiratory system consists of the upper airways, the respiratory tract, and the lungs. When air is breathed in, it enters the body through the upper airways—the nasal and oral cavities—into a muscular tube called the pharynx (see figure 9–9). From there, it moves into the voice box (larynx), which also contains the vocal cords and the epiglottis, a flap-like structure at the opening of the larynx that prevents food and water from entering into the respiratory tract. From the larynx, air enters the trachea, which is a rigid tube held open by C-shaped rings of cartilage, and then into smaller airway passages called bronchi.
There are two major bronchi that conduct air to the left and right lungs. Inside each of the lungs, the bronchi divide many more times; as they divide, they become progressively smaller until they become tiny tubes that have no cartilage, called bronchioles. Finally, they terminate in single-layered cell structures called alveoli, where the exchange of gases takes place between the lungs and the blood. Breathing—and therefore the exchange of gases— can occur because movement of the muscles of the chest wall create pressure changes that are responsible for air moving into the lungs (inspiration) and out of the lungs (expiration).
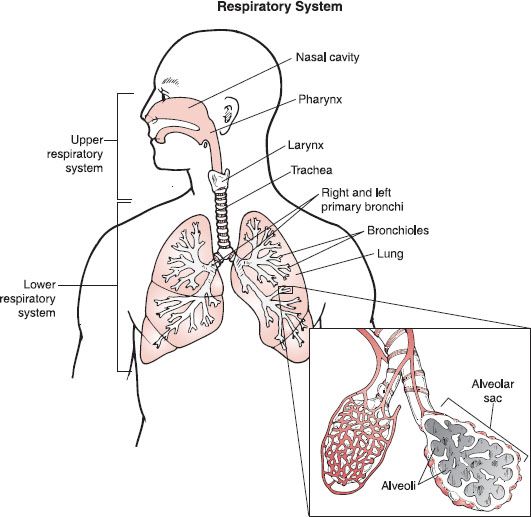
Figure 9–9. Anatomy of the respiratory system. The upper respiratory system is comprised of structures that bring air into the lungs. The lower respiratory system contains the bronchi, bronchioles, and the lungs. At the terminal end of the bronchioles are the alveolar sacs where the exchange of gases takes place.
Lining the larynx and trachea are specialized cells that secrete mucus, which traps particles and dust from the air breathed in to the lungs. The mucus and trapped particles are then propelled toward the pharynx by the beating action of cilia (hair-like projections), where they are swallowed.
The respiratory system is responsible for gas exchange, which ultimately allows oxygen to be taken to cells in the body and carbon dioxide to be removed from the same cells. Gas exchange occurs at two levels: in the lungs between the alveoli and the blood, and at the cellular level between blood and the tissues. In red blood cells (erythrocytes), a molecule called hemoglobin is responsible for carrying oxygen. Carbon dioxide is transported in the blood, some attached to hemoglobin and the rest dissolved in the blood.
Deoxygenated blood (low in oxygen and high in carbon dioxide) travels from the right side of the heart to the lungs; at the level of the alveoli, carbon dioxide is released from the red blood cells into the lungs and exchanged for oxygen that has been brought into the lungs by the process of inspiration. Carbon dioxide is released by the lungs (through the nose or mouth) into the air by the process of expiration. The blood, rich in oxygen, then travels to the left side of the heart where it is pumped to cells of the various tissues and organs oxygen delivering to the cells. After the exchange of gases in the cells, the deoxygenated blood again returns to the lungs via the right side of the heart.
Another function of the respiratory system is maintaining the balance of acidity and alkalinity (pH) of the blood. The blood is kept at a slightly alkaline level (its pH is 7.4) in order to prevent the malfunction of critical proteins, such as receptors and enzymes. The respiratory system regulates blood pH by eliminating carbon dioxide from the body. If an individual’s breathing rate becomes abnormally low, respiratory acidosis can occur; if it becomes too fast, for example, during hyperventilation, then respiratory alkalosis occurs. If the blood becomes too acidic, a condition called acidosis develops, and this can affect the functioning of the nervous system, and in severe cases can cause respiratory failure. The nervous system is also affected if the pH of the blood becomes too basic. In this case, a condition called alkalosis develops and the nervous system becomes overactive, which results in seizures and convulsions.
Other functions of the respiratory system involve filtering out irritants in the air breathed and protecting the body from invading pathogens.
Common Diseases and Disorders
Asthma. Asthma is a disease of the lungs characterized by inflammation of the bronchioles, increased mucus secretion, and abnormal contractions of the smooth muscles in the bronchioles, which leads to the narrowing of the airway passages. The symptoms are difficulty breathing, wheezing, and coughing. The cause of the disease is often an allergic response to pollen, molds, dust mites, or pet dander. Other factors can also induce asthma, such as exercise, cold air, and stress. Treatment of asthma involves the use of drugs that can open and relax the airways of the lungs and decrease the inflammation that is associated with this disease.
Chronic Obstructive Pulmonary Disease (COPD).
Includes two conditions known as emphysema and chronic obstructive bronchitis. In emphysema, there is damage and destruction of the walls between the air sacs (alveoli), causing them to lose their shape and become floppy. The damage leads to fewer and larger alveoli instead of many tiny ones. This makes it difficult to exchange gases between the blood and the air entering the lungs. In chronic bronchitis, the lining of the bronchi is irritated and inflamed. This causes the lining to thicken. Thick mucus forms, which plugs the airways. The symptoms of COPD are difficulty breathing, coughing, wheezing, and chest tightness. The disease is believed to be caused by factors such as smoking, other environmental hazards such as air pollutants, and occupational hazards such as coal and stone dust. Treatment is chronic and includes lifestyle changes and drugs that open or dilate the airways and reduce inflammation.
Upper and Lower Respiratory Infections. Many viruses can lead to upper respiratory tract infections of the nose, oropharynx, and larynx—for example, the common cold, pharyngitis, and laryngitis. Lower respiratory tract infections (lower airways and lungs) can be caused by either viruses or bacteria. Examples include the influenza virus and pneumonia, which can be caused by either bacteria or viruses. Supportive treatment is used for viral infections, and antibiotics are used to treat infections caused by bacteria.
The Musculoskeletal System
Overview of Structure and Function
This system consists of a framework of individual bones called the skeleton. The skeleton is made up of 206 bones, each of which varies in size and shape (see figure 9–10). Bones are connected by ligaments, and the points of connection are joints. Some bones, such as those in the skull, are fixed to hold the structure together and prevent movement. Others are partially moveable to allow some flexibility, such as the spine. Additionally, some joints are freely moveable, such as those found in the hipbones, arms, and legs.
The skeleton of a man and woman are almost identical, with only small differences between the sexes. For example, the density of the bones in the arms and legs are heavier in males, and the hip bones of females are wider.
Covering the skeleton are the skeletal muscles, most of which are connected to the bones by tendons. Some muscles, such as the facial muscles, are attached to the skin. There are more than 600 muscles in the body, which vary in mass and length (see figure 9–11). Each muscle consists of numerous individual muscle cells called muscle fibers that are highly elongated in shape, and, in many cases, these muscle fibers can run the length of the bone they are covering (see figure 9–12).
The muscle fibers are made up of thick and thin filaments that contain specialized proteins, called actin and myosin. Actin and myosin are responsible for making a muscle contract and relax. The orderly arrangement of actin and myosin in the muscle fibers gives skeletal muscle its characteristic striped appearance when viewed under the microscope. Skeletal muscle is under voluntary control through the somatic branch of the peripheral nervous system.
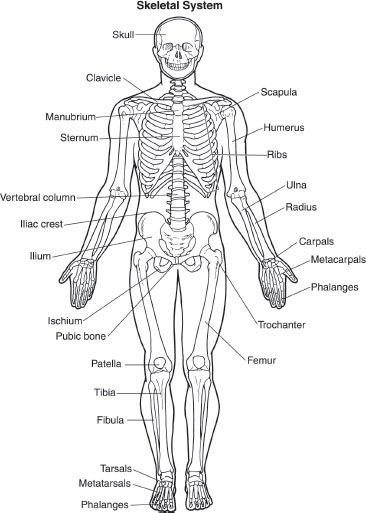
Figure 9–10. The skeletal system anterior view. The skeletal system is an extensive system of large and small bones that supports the muscle and protects the internal organs.
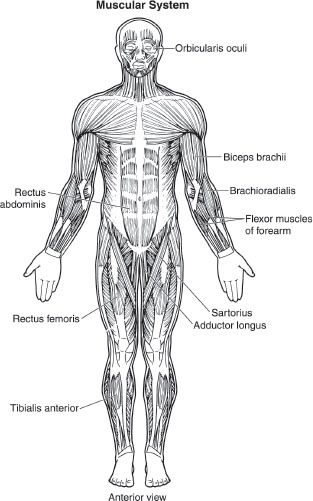
Figure 9–11. The skeletal muscles of the body. The skeletal muscles of the body attach to the skeleton via ligaments and tendons. When they contract, they can move or restrain parts of the body.
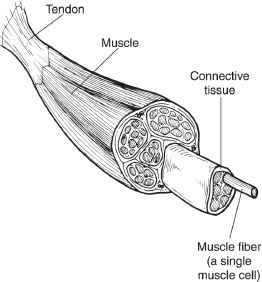
Figure 9–12. The structure of skeletal muscle. Each muscle is comprised of single muscle cells known as muscle fibers. The muscle fiber is formed from bundles of myofibrils that are surrounded by a specialized membrane known as the sarcolemma, which contains the sarcoplasmic reticulum and T-tubules. Each myofibril is composed of thick and thin filaments, and their arrangement gives skeletal muscle its striated appearance.
In addition to skeletal muscle, there are two other types of muscle found in the body: smooth (visceral) muscle and cardiac muscle. Both of these are under involuntary control by the autonomic nervous system and internal pacemakers. Smooth muscle is the primary muscle found in the internal organs of the body: stomach, intestines, glands, and blood vessels. This type of muscle also contains the same contractile proteins, actin and myosin. Actin and myosin, however, are arranged in layers, which allow this muscle to stretch and expand. A good example is the muscle of the bladder. Cardiac muscle is found exclusively in the heart, and, like skeletal muscle, it has a characteristic striped appearance.
The skeleton functions as a dense, protective framework for the body, which can shield internal organs, in addition to forming a structure to which other tissues, such as muscle, can attach. The skeleton also supports the weight of the body. Moreover, most bones of the body contain red bone marrow inside their structure. The red bone marrow is essential for the production of all blood cells.
The skeletal muscles function to move the body by their ability to contract and relax in a synchronized fashion. When the somatic nervous system sends a signal to the muscle, it contracts. Some muscles contract and relax quickly, such as the eyelid muscles, whereas others contract for a longer period of time, such as the muscles in the back that control posture.
 The proper functioning of muscles allows an individual to carry out a wide range of complex movements, from gross motor control movements required for running to fine motor control movements required for playing the piano.
The proper functioning of muscles allows an individual to carry out a wide range of complex movements, from gross motor control movements required for running to fine motor control movements required for playing the piano.
Skeletal, smooth, and cardiac muscles are regulated by the nervous system. Smooth and cardiac muscles, however, have their own ability to initiate electrical signals (and therefore muscle activity) without input from the nervous system. This type of function is called pacemaker activity.
Common Diseases and Disorders
Osteoporosis. A condition that affects the bones. The structure of the bone changes from a dense and heavy structure to a thinner and lighter one because of a loss of proteins and minerals such as calcium and phosphate. In this condition, bone loss occurs faster than bone replacement, and the bones become fragile, lighter, and prone to fractures.
The symptoms of the disease are “silent,” and it is often not until a fracture occurs, or a characteristic “rounding” of the back is evident, or a person becomes shorter, that the disease has progressed to a point that a diagnosis can be made. Risk factors for developing osteoporosis include being female (especially after menopause), older age, a family history of osteoporosis or broken bones, certain diseases (such as Cushing syndrome, which is marked by an over production of the hormone cortisol), and low calcium and vitamin D intake. Treatment includes calcium and vitamin D supplements and medications to prevent bone loss and rebuild bone.
Rheumatoid Arthritis. An inflammatory disease of the joints that can occur at any age. It is believed to be an autoimmune disease whereby the body produces specific proteins called antibodies that cause inflammation of a special membrane around the joints. In the early stages of the disease, the person may complain of a low-grade fever, lack of energy, loss of appetite, or a general feeling of malaise. As the disease advances, the joints become swollen, red, painful, and stiff. Joint destruction can occur rapidly in rheumatoid arthritis. Treatment involves drugs that decrease the inflammation in the joints and prevent further destruction of the joint tissue.
Osteoarthritis. A condition whereby the cartilage of the joint deteriorates. This starts to affect the bone underneath, which eventually begins to thicken and distort. It generally affects the weight-bearing joints (i.e., the hips, knees, and spine) of the body. Pain, swelling, and stiffness of the joints are characteristic symptoms of this condition. This type of arthritis most often occurs as a result of aging. The joint damage occurs slowly as the joints wear out. Drug treatment is focused on relieving pain and joint swelling.
Muscle Sprain and Strain. When a muscle or a tendon becomes injured, for example, during a sport activity or overwork, it is called a strain injury.12 If the ligament becomes injured, it is called a sprain injury.12 Sprains and strains can happen in a number of regions in the body, such as the back, wrist, ankle, knee, and hamstring muscles. Over-the-counter drugs such as ibuprofen are commonly prescribed to reduce the pain and swelling associated with these injuries.
The Endocrine System
Overview of Structure and Function
The endocrine system is made up of a group of glands that release chemical substances into the blood. The glands that make up the endocrine system are widely dispersed throughout the body and are not structurally related to each other. Even though the endocrine glands are not connected to each other, they make up a system in a functional sense by performing the same role: they secrete chemical messengers called hormones into the bloodstream. The hormones circulate in the bloodstream and affect many types of body cells. The major endocrine glands are shown in figure 9–13.
The endocrine system is made up of the endocrine glands and the hormone(s) they secrete into the bloodstream. The hormone, together with the target tissue or cells, functions to relay information and instructions throughout the body.
The purpose of the secreted hormones is to bring on a specific response in other cells of the body, which are in another location. Some hormones function only to regulate the production of other hormones, whereas others exert their effects on the target tissues themselves. The hormones are secreted into the bloodstream, giving them access to all other cells of the body.
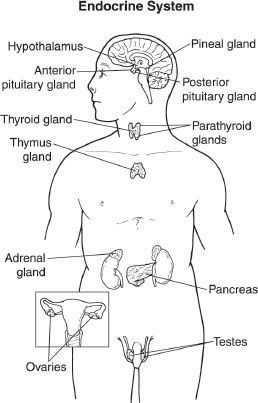
Figure 9–13. The major glands of the endocrine system. The endocrine system is made up of a group of glands that secrete chemical substances, known as hormones, into the bloodstream. The endocrine glands are widely dispersed throughout the body and are not structurally related to each other.
The endocrine system works to
 Maintain the body’s normal internal balance (homeostasis)
Maintain the body’s normal internal balance (homeostasis)
 Help the body deal with stressful situations
Help the body deal with stressful situations
 Regulate growth and development
Regulate growth and development
 Control reproduction
Control reproduction
 Produce, use, and store energy
Produce, use, and store energy
The endocrine glands are characterized by the hormone(s) that they secrete and the target tissue(s) that the hormone affects (see table 9–1).
Common Diseases and Disorders
Because there are so many endocrine glands, hormones, and target cells throughout the body, when something in one of the endocrine glands goes wrong, it can have a profound impact on a number of other bodily functions. Generally, problems within the endocrine system are due to one of two things: either too little or too much of a hormone is produced. Thus, disorders resulting from decreased production of hormones by the endocrine glands are treated by giving the patient a replacement hormone. When too much of a hormone is produced, drugs are used to inhibit hormone production. Disturbances within the endocrine system may also occur from damage done directly to the endocrine gland, or, less commonly, from a decreased sensitivity of the target tissue to the hormone. Because the actions of hormones are so extensive, this review will focus only on the most common endocrine disorders.
Table 9–1. Endocrine Glands and Hormonal Physiologic Effects on the Body
| Endocrine Gland | Principal Hormone(s) Secreted | Target Tissue(s) | Physiologic Effect of Hormone |
| Hypothalamus | Releasing and inhibiting hormones | Anterior pituitary | Controls release of anterior pituitary hormones |
| Anterior pituitary | Thyroid-stimulating hormone (TSH) | Thyroid | Production of thyroid hormone |
| Adrenocorticotropic hormone (ACTH) | Adrenal cortex | Secretion of cortisol | |
| Growth hormone | Bones; soft tissues | Stimulates growth of bones and soft tissues | |
| Follicle-stimulating hormone (FSH) | Females: ovary | Promotes growth of ovarian follicle; stimulates estrogen secretion | |
| Luteinizing hormone (LH) | Males: testes | Stimulates sperm production | |
| Females: ovary | Stimulates ovulation; stimulates estrogen and progesterone secretion | ||
| Prolactin | Males: testes | Stimulates testosterone secretion | |
| Females: breast | Promotes breast development; stimulates milk secretion | ||
| Posterior pituitary | Vasopressin (antidiuretic hormone) | Kidney | Causes water retention |
| Oxytocin | Uterus | Causes contractions | |
| Breasts | Causes ejection of milk | ||
| Pineal | Melatonin | Brain; anterior pituitary; reproductive organs; possibly other sites | Sets the body’s “time clock;” causes sleep in response to darkness |
| Thyroid | Thyroid hormones (T3 and T4) | Most cells | Increases the metabolic rate; necessary normal growth and development |
| Parathyroid | Parathyroid hormone | Bone; kidney; intestine | Increases amount of calcium in the bloodstream; decreases amount of phosphate in the bloodstream |
| Thymus | Thymosin | T lymphocytes | Enhances the production of T lymphocytes |
| Pancreas | Insulin | Most cells | Promotes use and storage of nutrients, particularly glucose, after eating |
| Glucagon | Most cells | Maintains glucose levels in the bloodstream during periods of no food | |
| Somatostatin | Digestive system | Inhibits digestion and absorption of nutrients | |
| Adrenal medulla | Epinephrine and norepinephrine | Nervous system sites throughout the entire body | Reinforces the nervous system; “fight or flight” system |
| Adrenal cortex | Aldosterone | Kidney | Increases sodium retention and potassium secretion |
| Cortisol | Most cells | Increases glucose in the bloodstream | |
| Androgens | Females: bone and brain | Puberty growth spurt and sex drive in females | |
| Testes (male) | Testosterone | Male sex organs; body as a whole | Stimulates production of sperm; responsible for development of sex characteristics; promotes sex drive |
| Ovaries (female) | Estrogen | Female sex organs; body as a whole | Stimulates uterine and breast growth; responsible for development of sex characteristics |
| Progesterone | Uterus | Prepares for pregnancy |
Diabetes Mellitus. Diabetes is the most common endocrine disease, characterized by high levels of glucose (sugar) in the bloodstream and urine. Symptoms include frequent urination, unusual thirst, extreme hunger, and frequent infections. Type 1 diabetes (previously known as juvenile diabetes) is characterized by a lack of insulin production from the pancreas. It is most commonly diagnosed in children and young adults and it is treated with insulin. Type 2 diabetes is the most common type of diabetes, and it is characterized as either decreased production of insulin or an abnormal sensitivity of the tissues to the insulin that is present. Type 2 diabetes is treated with diet alone, oral hypoglycemic agents, insulin, or a combination of those remedies.
Diabetes Insipidus. This condition occurs when the pituitary gland doesn’t produce antidiuretic hormone (ADH, or vasopressin), or if the kidneys do not respond to the hormone ADH. As a result, the kidneys are unable to reabsorb water, which leads to high volumes of urine excreted and extreme thirst. It is treated with the replacement hormone vasopressin.
Thyroid Disease. Thyroid disease can result from the production of too little thyroid hormone (hypothyroidism), which is characterized by weakness, fatigue, muscle cramps, intolerance to cold, dry skin, and lethargy. Production of too much thyroid hormone causes hyperthyroidism, which is characterized by weakness, sweating, weight loss, nervousness, moist skin, and intolerance to heat. An individual suffering from hypothyroidism can be treated with thyroid hormone replacement. Hyperthyroidism is not as easily treated. Depending upon the cause of increased thyroid levels, treatment may range from using a thyroid hormone blocker to treatment of the thyroid gland with radioactivity to destroy part of the gland.
The Immune System
Overview of Structure and Function
The body is equipped with a complex defense system— the immune system—which provides constant protection against invasion by foreign substances or organisms. The immune system is the name of a collection of molecules, cells, and organs whose complex interactions form an efficient system that is usually able to protect an individual from both outside invaders and its own altered internal cells, and also able to rid the body of unwanted cellular debris.
The immune system is composed of the cells in our bone marrow, the thymus gland, the lymphatic system of ducts and nodes, the spleen, and the blood that all work together to protect the body from invasion (see figure 9–14).
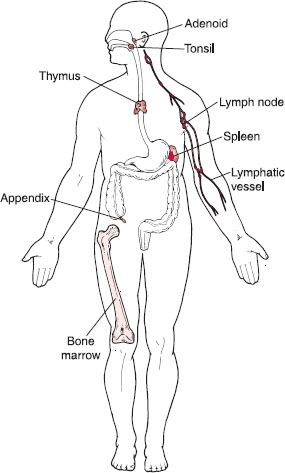
Figure 9–14. Tissues of the immune system. The immune system is composed of the cells of the bone marrow, the thymus, and the lymphatic system of ducts and nodes, spleen, and lymphoid tissue (tonsils, adenoids, appendix), which protect the body against foreign materials. Note that the components of the immune system are widely dispersed throughout the body.
The “worker” cells of the immune system, which are responsible for the various immune defenses, are found in the bloodstream and known as white blood cells (leukocytes). Several different types of leukocytes circulate in the blood stream. There are numerous other cells that contribute to the function of the immune system including phagocytes (such as monocytes, macrophages, and neutrophils), granulocytes (eosinophils and basophils), and lymphocytes. The two types of lymphocytes are called B cells and T cells.
The organs of the immune system are located throughout the body, and they are known as lymphoid organs because they are concerned with the growth, development, and deployment of lymphocytes. The organs of the immune system are connected with one another and with other organs of the body by a network of lymphatic vessels similar to blood vessels. Immune cells and foreign particles are transported through the lymphatic vessels in lymph, a clear fluid that bathes the body’s tissues. The major lymphoid organs of the immune system are lymph nodes, tonsils, adenoids, the appendix, the spleen, and the thymus. Lymph nodes are small, bean-shaped structures that are located throughout the body along the lymphatic routes. Lymph nodes function to remove any cellular debris before it enters the bloodstream. They contain specialized compartments where immune cells congregate.
 When the body is threatened by microorganisms, viruses, or cancer cells, the immune system goes into action to provide protection by destroying the threatening organisms. This is known as the immune response.
When the body is threatened by microorganisms, viruses, or cancer cells, the immune system goes into action to provide protection by destroying the threatening organisms. This is known as the immune response.
Under normal circumstances, the immune system does not mount a response against itself. This lack of an immune response is called tolerance. It is vitally important that the immune response is able to distinguish between self and nonself. Every cell carries distinctive molecules that identify it as self, and immune cells do not attack tissues that carry a self marker.
Foreign molecules carry distinctive markers as well: characteristic shapes that allow the immune system to recognize them as foreign and initiate an immune response. Any substance capable of triggering an immune response (and carrying a distinctive nonself marker) is known as an antigen. An antigen can be a bacterium or a virus, or even a portion or product of one of these organisms. Antigens also trigger the production of antibodies by the immune system, and this is the mechanism by which immunity, or resistance, to a disease is acquired. Tissues or cells from another individual also act as antigens; that is why transplanted tissues are rejected as foreign without preventive drug therapy.
Invading microorganisms attempting to get into the body must first get past the body’s first line of defense: the skin and mucous membranes. If the invader gets past these initial physical barriers, the immune system “players” are called to duty.
The Immune Response. The immune response is engineered to rid the body of unwanted invaders, and it can occur in a number of different ways. These mechanisms, known all together as immunity, include both innate (naturally occurring) and also adaptive or acquired immune responses. Innate immune responses are nonspecific responses that defend against foreign material nonselectively, even the first time the body is exposed to it. Adaptive or acquired immune responses are specific responses that target specific invaders, because the body has been exposed to the invader at least once before. In an adaptive immune response, the body is ready because it has been specially prepared for the invader to return.
The immune response is initiated once the immune system recognizes a foreign molecule. The first immune system cells the invader encounters are cells circulating in the bloodstream that attack all invaders, regardless of the antigens they carry. One example of an innate immune response is the inflammation response. Inflammation is a nonspecific response to foreign invasion or tissue damage that occurs when neutrophils and macrophages destroy foreign or damaged cells. The ultimate goal of inflammation is to bring more help from the immune system to destroy the invaders, remove the dead cells, and begin the process of tissue healing and repair. These actions are responsible for the signs and symptoms of inflammation: swelling, redness, heat, and pain.
Common Diseases and Disorders
A number of clinical problems can occur when something within the immune system goes wrong. If the immune system is deficient in the number of T cells it produces, the immune system fails to defend itself against viral infections. Similarly, if the immune system is deficient in its ability to make B cells, the immune system fails to defend itself against bacterial infections.
Allergy. One of the most well-known disorders of the immune system is allergy. Allergies occur when the body mounts an immune response against a normally harmless substance such as grass pollen. In this case, the offending agent is called an allergen. The first time an allergy-prone individual is exposed to an allergen (such as grass pollen), the individual’s B cells make large amounts of grass pollen IgE antibody. These IgE molecules attach to granulecontaining cells known as mast cells, which are plentiful in the lungs, skin, tongue, and linings of the nose and gastrointestinal tract. The next time the individual is exposed to grass pollen, the IgE-primed mast cells release powerful chemicals, including histamine, that cause the wheezing, sneezing, itching, and other symptoms of allergy. Drugs called antihistamines are commonly used to treat and prevent allergies.
Autoimmune Disease. Characterized by the body’s immune system destroying its own normal cells. When the body loses its ability to correctly identify body cells belonging to self, it can mount immune responses directed against its own cells and organs. In this event, antibodies produced by B cells against its own body are called autoantibodies, and they are responsible for many diseases. Autoimmunity can cause a broad range of human illnesses. For instance, T cells that attack pancreas cells contribute to diabetes, and an autoantibody known as rheumatoid factor is common in persons with rheumatoid arthritis.
Acquired Immune Deficiency Syndrome (AIDS).
Caused by infection with the human immunodeficiency virus (HIV). This virus is passed from one person to another through blood-to-blood and sexual contact. HIV destroys T-helper cells, which are essential to the normal function of the immune system. Infection with HIV can weaken the immune system to the point that it has difficulty fighting off infections. These types of infections are known as opportunistic infections because they take the opportunity a weakened immune system provides to cause illness. Many of the infections that cause illness or may be life threatening for people with AIDS usually do not cause illness in those with a normal immune system.
Most people infected with HIV carry the virus for years before enough damage is done to the T-helper cells and the immune system for AIDS to develop. There is a strong connection between the amount of HIV in the blood and the decline in T-helper cells, and the development of AIDS. Therefore, drug therapy has been targeted at reducing the amount of virus in the body with anti-HIV medications to slow the immune system destruction and progression of the disease.
The Gastrointestinal System
Overview of Structure and Function
At its simplest, the gastrointestinal (GI) tract is a hollow tube running through the body from the mouth to the anus. The adult gastrointestinal tract (also known as the digestive tract) is about 30 feet long. The basic components of the gastrointestinal system are described below (see figure 9–15):
 Mouth: The mouth, or oral cavity, is the entrance to the digestive tract. Food is broken down mechanically by chewing. Saliva is added as a lubricant, and it also contains enzymes that begin the digestion of starch.
Mouth: The mouth, or oral cavity, is the entrance to the digestive tract. Food is broken down mechanically by chewing. Saliva is added as a lubricant, and it also contains enzymes that begin the digestion of starch.
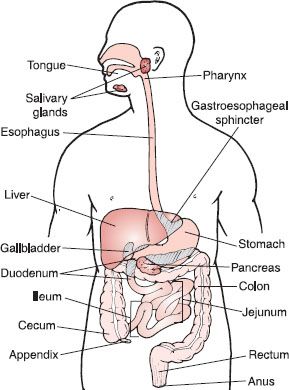
Figure 9–15. Anatomy of the major components of the gastrointestinal tract. The gastrointestinal tract can be thought of as a long, hollow tube running through the body from the mouth to the anus. Shown are the basic components of the gastrointestinal tract, which function to transfer energy from ingested food to the internal cells of the body and rid the body of undigested waste.
 Pharynx: The pharynx is about five inches long, and it is a cavity located at the rear of the throat. It serves as a shared passageway for food and air. flap called the epiglottis reflexively closes the trachea while food is being swallowed.
Pharynx: The pharynx is about five inches long, and it is a cavity located at the rear of the throat. It serves as a shared passageway for food and air. flap called the epiglottis reflexively closes the trachea while food is being swallowed.
 Esophagus: The esophagus is a fairly straight muscular tube that extends between the pharynx and the stomach; it serves simply to connect the mouth with the stomach. It is the least complex section of the gastrointestinal tract. The esophagus is guarded at both ends by sphincters, rings of muscle that control passage of contents through an opening into or out of a hollow organ. When the sphincter is closed, it prevents passage through the tube it guards.
Esophagus: The esophagus is a fairly straight muscular tube that extends between the pharynx and the stomach; it serves simply to connect the mouth with the stomach. It is the least complex section of the gastrointestinal tract. The esophagus is guarded at both ends by sphincters, rings of muscle that control passage of contents through an opening into or out of a hollow organ. When the sphincter is closed, it prevents passage through the tube it guards.
 Stomach: The stomach is a pouch-like chamber located in the upper middle of the abdominal cavity; it lies between the esophagus and the small intestine. The stomach stores food while thoroughly mixing it with acids and enzymes, breaking it into much smaller digestible pieces. When it is empty, an adult’s stomach has a volume of one-fifth of a cup, but it can expand to hold more than 8 cups of food after a large meal. Chemical digestion of most food begins in the stomach, and food particles are reduced to a liquid form. Preliminary absorption of some drugs begins in the stomach.
Stomach: The stomach is a pouch-like chamber located in the upper middle of the abdominal cavity; it lies between the esophagus and the small intestine. The stomach stores food while thoroughly mixing it with acids and enzymes, breaking it into much smaller digestible pieces. When it is empty, an adult’s stomach has a volume of one-fifth of a cup, but it can expand to hold more than 8 cups of food after a large meal. Chemical digestion of most food begins in the stomach, and food particles are reduced to a liquid form. Preliminary absorption of some drugs begins in the stomach.
 Small Intestine: The small intestine is a coiled tube nearly ten feet long. The final stages of chemical digestion occur in the small intestine, where almost all nutrients from the ingested food are absorbed. The inner wall of the small intestine is covered with microscopic fingerlike projections called villi. The villi are where nutrients and many drugs are absorbed into the body.
Small Intestine: The small intestine is a coiled tube nearly ten feet long. The final stages of chemical digestion occur in the small intestine, where almost all nutrients from the ingested food are absorbed. The inner wall of the small intestine is covered with microscopic fingerlike projections called villi. The villi are where nutrients and many drugs are absorbed into the body.
 Large Intestine: The large intestine is mainly a drying and storage organ. The large intestine is made up of three parts: (1) the cecum, a small sac-like section of bowel, at the end of which the appendix hangs; (2) the colon, which extends from the cecum, up the right side of the abdomen (ascending colon), across the upper abdomen (transverse colon), and then down the left side of the abdomen (descending and sigmoid colon); (3) the rectum, which is connected to the last part of the colon ultimately terminates at the anus. The cecum and colon are about five feet long, whereas the rectum is only five inches long. The anal sphincter controls flow out of the GI tract.
Large Intestine: The large intestine is mainly a drying and storage organ. The large intestine is made up of three parts: (1) the cecum, a small sac-like section of bowel, at the end of which the appendix hangs; (2) the colon, which extends from the cecum, up the right side of the abdomen (ascending colon), across the upper abdomen (transverse colon), and then down the left side of the abdomen (descending and sigmoid colon); (3) the rectum, which is connected to the last part of the colon ultimately terminates at the anus. The cecum and colon are about five feet long, whereas the rectum is only five inches long. The anal sphincter controls flow out of the GI tract.
 Liver: The liver is located beneath the ribcage in the right upper part of the abdomen. It is the center of metabolic activity in the body, and it also plays a large role in the digestion and absorption of nutrients by producing bile, which emulsifies dietary fat.
Liver: The liver is located beneath the ribcage in the right upper part of the abdomen. It is the center of metabolic activity in the body, and it also plays a large role in the digestion and absorption of nutrients by producing bile, which emulsifies dietary fat.
 Gallbladder: This is located near the liver and stores bile. When dietary fat passes into the small intestine, bile is released to emulsify fat and aid in the absorption of fat-soluble vitamins.
Gallbladder: This is located near the liver and stores bile. When dietary fat passes into the small intestine, bile is released to emulsify fat and aid in the absorption of fat-soluble vitamins.
 Pancreas: The pancreas is located beneath the stomach. It serves an important role because it provides a potent mixture of digestive enzymes to the small intestine, which are critical for digestion of food. The pancreas also serves as an endocrine organ by secreting hormones such as insulin and glucagon.
Pancreas: The pancreas is located beneath the stomach. It serves an important role because it provides a potent mixture of digestive enzymes to the small intestine, which are critical for digestion of food. The pancreas also serves as an endocrine organ by secreting hormones such as insulin and glucagon.
 The gastrointestinal tract functions to transfer energy from the food we eat to the cells in the internal environment of the body. This system also functions to eliminate undigested food residues to the external environment.
The gastrointestinal tract functions to transfer energy from the food we eat to the cells in the internal environment of the body. This system also functions to eliminate undigested food residues to the external environment.
Plants are capable of transforming the energy from the sun into usable forms of energy to survive; humans are not. Humans must rely on ingested food as an essential energy source for the cells of the body to use to carry out vital energy-dependent activities. The breakdown of food is accomplished through a combination of mechanical and chemical (enzymatic) processes. To accomplish this breakdown, the digestive “tube” requires considerable assistance from accessory digestive organs, such as the salivary glands, liver, and pancreas, which dump their secretions into the tube. The main function of the digestive tube is to break down the food we eat (proteins, fats, and carbohydrates), which cannot be absorbed whole, into smaller molecules (amino acids, fatty acids, and glucose) that can be absorbed across the tubular and into the circulatory system for distribution throughout the entire body. Some of the molecules are used for energy, some are used as building blocks for tissues and cells, and some are stored for future use.
The first step in the digestive process is the chewing and mixing of ingested food by the teeth. The purposes of chewing are (1) to tear, grind, and break down food particles into smaller pieces to facilitate swallowing, and (2) to mix food with saliva. Saliva is produced by salivary glands located outside of the mouth, and it is secreted into the mouth by small ducts. The mass of chewed, moistened food (known as a bolus) is moved to the back of the mouth by the tongue. In the pharynx, the bolus triggers an involuntary swallowing reflex that prevents food from entering the lungs and directs the bolus into the esophagus.
Muscles in the esophagus propel the bolus by waves of involuntary contractions (peristalsis) of the muscle lining the esophagus (see figure 9–16). The bolus passes through the lower esophageal sphincter (LES) into the stomach. The stomach provides four basic functions that assist in the early stages of digestion and prepare the ingested food materials for further processing in the small intestine: (1) it serves as a short-term storage site, allowing a rather large meal to be consumed quickly and dealt with over an extended period of time; (2) it is in the stomach that substantial chemical and enzymatic digestion is started; (3) vigorous contractions of the stomach muscles mix and grind food with acidic stomach secretions, resulting in liquefaction of food, which must occur before it can be delivered to the small intestine; and (4) once food is liquefied in the stomach, it is slowly released into the small intestine for further processing.
By the time food is ready to leave the stomach it has been processed into a thick liquid called chyme (see figure 9–17). The outlet of the stomach—a small sphincter muscle called the pylorus—keeps the chyme in the stomach until it reaches the right consistency to pass into the small intestine. Chyme is then forced down into the duodenum of the small intestine by the action of peristalsis. In the small intestine, where the majority of nutritional and drug absorption occurs, digestive chemicals work on the partially digested food.
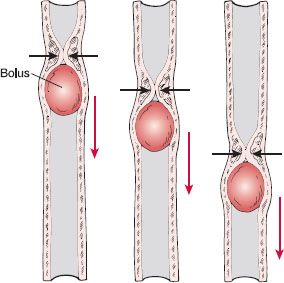
Figure 9–16. Peristalsis. Waves of involuntary muscular contractions propel boluses of food along the esophagus down toward the stomach.
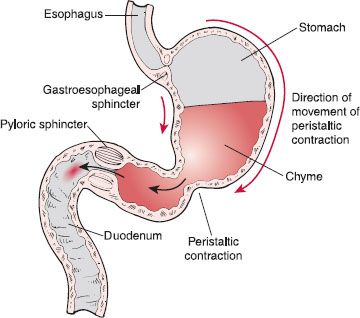
Figure 9–17. Gastric emptying. Peristaltic contractions originate in the upper portions of the stomach and gain strength as they near the pyloric sphincter. These contractions function to mix and propel chyme (liquid stomach contents) toward the pyloric sphincter and are responsible for pushing small quantities of chyme through the sphincter into the duodenum.
The pancreas and liver connect with the small intestine and send secretions into it to aid in the process of digestion. These include pancreatic juice, which contains enzymes that help digest carbohydrates, proteins, and fats; and bile, which breaks down and aids in the absorption of fat. Although bile is produced in the liver, it is stored in the gallbladder and sent into the small intestine through the bile duct. Once broken down, these now-soluble food products are dissolved and absorbed directly into the bloodstream through the walls of the small intestine, along with vitamins and minerals. This process is called absorption.
By the time the food reaches the large intestine, the work of digestion is almost finished. The main function of the large intestine is to remove water from the undigested matter and form it into stool, which will be eliminated from the body by excretion. Bacteria in the colon aid digestion of the remaining food products. The final waste product, the feces, is then stored in the rectum until it is released from the body through the anal sphincter. The elimination of feces is called a bowel movement (BM), because the intestinal tract is referred to as the bowel.
Common Diseases and Disorders
If the normal function of the gastrointestinal tract is disrupted, a number of different clinical situations may occur. They differ depending on the site of the malfunction or disease.
Ulcers. The stomach contains strong acids to aid in the breakdown of food products. Under normal conditions, the stomach and small intestines are extremely resistant to irritation by the strong acids they contain. A bacterium (most commonly helicobacter pylori), or the chronic use of certain medications or alcohol, may weaken the protective coating of the stomach and duodenum and allow acid to get through to the sensitive lining beneath. Both the acid and the bacteria can irritate and inflame the lining (a condition known as gastritis) or cause peptic ulcers, which are sores or holes that form in the lining of the stomach or the duodenum and cause pain or bleeding. Medications that block the production of acid are used to treat these conditions; a course of antibiotics may be given if helicobacter pylori is involved.
Esophageal Disorders. Inflammation of the esophagus (esophagitis) can be caused by complications of certain medications or infection. Esophagitis is also commonly caused by a condition in which the lower esophageal sphincter is weakened and thus allows the acidic contents of the stomach to move backwards, or reflux, up into the esophagus. The result is inflammation and tissue damage of the esophagus. This condition is known as gastroesophageal reflux disease (GERD). Medications that reduce the production of stomach acid are used to protect the tissue lining the esophagus.
Gastrointestinal Infections. Infections of the gastrointestinal tract are quite common and are caused most commonly by viruses (such as enterovirus or rotavirus), by bacteria (such as salmonella, shigella, or E. coli); or by parasites or protozoan organisms. The microorganisms that cause GI infections often increase the muscle contractions (peristaltic) activity of the gastrointestinal tract; this results in vomiting and diarrhea. When a gastrointestinal infection is present, vomiting and diarrhea often occur, a protective response to rid the body of the harmful organisms or toxins. GI infections may be treated with anti-infective medications, depending on the causative organism.
Inflammatory Bowel Disease. Inflammatory bowel disease is a chronic inflammation of the intestines. There are two primary types: ulcerative colitis, which affects just the rectum and the large intestine, and Crohn disease, which can affect the whole gastrointestinal tract, from the mouth to the anus. The most common symptoms of inflammatory bowel disease are chronic abdominal pain, and intermittent, severe diarrhea, which may be bloody, and weight loss. Flare-ups of inflammatory bowel disease can occur at any time, but they are especially common during times of stress. Drug therapy is aimed at reducing inflammation and preventing flare-ups of the disease.
Irritable Bowel Syndrome. Irritable bowel syndrome is a chronic condition in which the bowels are especially sensitive to certain foods and stress. It can also be triggered by anxiety. The cause is unknown. Symptoms include abdominal pain, bloating, and abdominal discomfort. Some people have constipation as the predominant symptom and mucous may cover the feces. Others have diarrhea as the predominant symptom, whereas others may alternate between the two. Treatment depends on the predominant symptoms and may include changes in diet in addition to drug therapy.
Diarrhea. Diarrhea is a condition in which bowel movements are abnormally frequent and feces are loose and watery. It occurs when the muscle contractions (peristalsis) of the intestines move the fecal material along too quickly and there is not enough time for the water content to be absorbed into the body. If diarrhea is severe, the body can lose too much water and electrolytes and become dehydrated. In addition to bacterial and viral infections, diarrhea can also be caused by food poisoning (when food is infested with harmful bacteria), drinking contaminated water, lactose intolerance, some medications, and stress. Anti-diarrheal drugs are commonly used if diarrhea is severe.
Constipation. In this condition, the contents of the intestines do not move along fast enough, and there is an infrequent and painful emptying of the intestines. Waste materials stay in the large intestine so long that too much water is removed and the feces become too hard and difficult to pass. Fiber and stool softeners are taken to prevent constipation.
The Urinary System
Overview of Structure and Function
The structures of the urinary system are the kidneys, ureters, the bladder, and the urethra. The kidneys are fist-sized, bean-shaped organs that produce urine and are located in the mid-abdominal cavity, toward the back (see figure 9–18). Each of the kidneys receives a large supply of blood which enters the organs via the renal arteries. The blood supplies oxygen to the kidney tissue and it is filtered by the kidneys to remove waste products (urine). Once the blood has been filtered, it leaves the kidneys via the renal veins and returns to the right side of the heart. Each kidney has a tube called a ureter that is responsible for transporting the urine to the bladder. The bladder is a small, muscular sac that can expand to a large volume to store urine until it is ready to be excreted from the body, via the urethra.
The kidney itself has highly specialized anatomy, which allows it to filter huge volumes of blood and produce urine. The outermost layer of the kidney is called the cortex, the inner layer is called the medulla, and the innermost region is called the renal pelvis. Contained in the cortex and medulla are the functioning units of the kidney, called nephrons; each kidney contains tens of thousands of nephrons. A tiny blood vessel called an arteriole delivers blood to each nephron to be filtered, with the end result being the formation of urine (see figure 9–19). All of the urine that has been formed by the nephrons is collected into the renal pelvis and then transported to the ureter.
The kidneys perform many important functions. One such function is to filter the blood as it passes through the nephrons and remove waste products, such as products from protein breakdown, while reabsorbing important substances, such as glucose and protein, and returning them to the circulation for use by the cells of the body. In the process of filtering the blood, urine is formed. The kidney also plays a critical role in regulating the volume of the plasma, and therefore the blood volume, which affects blood pressure. Another function is regulating the concentration of certain electrolytes (chemicals such as sodium, potassium, and bicarbonate) in the blood plasma, which are important for maintaining proper functioning of cells throughout the body. This is possible because the kidneys are able to selectively excrete, or reabsorb the electrolytes to maintain their appropriate balance in the blood. Additional functions of the kidney include maintaining the pH of the blood and the excretion of drugs and pesticides. Finally, the kidneys are involved in the production of erythropoietin, an important hormone that stimulates the production of red blood cells, and they also activate vitamin D3.
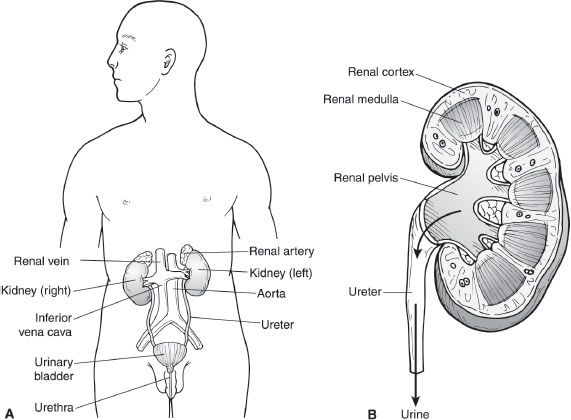
Figure 9–18. The anatomy of the urinary tract system. The urinary tract system is comprised of the right and left kidney and ureters, the bladder, and the urethra. The kidney has two major layers of tissue—renal cortex and renal medulla—and an inner structure—renal pelvis. Urine collects in the renal pelvis and flows from the kidneys, via the ureters, to the bladder, where it is stored until emptied outside the body by way of the urethra.
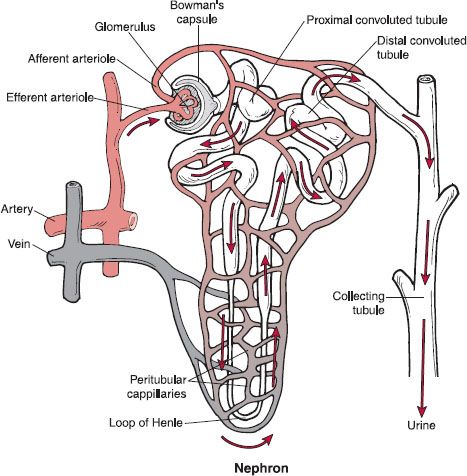
Figure 9–19. The nephron. The nephron is the basic functioning unit of the kidney. It processes blood plasma and produces urine. Fluid flows through the nephron in the following order: Bowman’s capsule, proximal convoluted tubule, loop of Henle, distal convoluted tubule, collecting duct.
Common Diseases and Disorders
Kidney Stones. In a condition known as nephrolithiasis, kidney stones are formed when the substances that are to be excreted in the urine instead crystallize in the pelvis of the kidney and form into small stones. They can be formed from substances such as calcium, phosphate, or uric acid. Many stones, if small enough in size, are excreted in the urine unnoticed. If the stones are too large, however, they can lodge themselves in the kidney or the bladder, and if they move they cause severe pain. In the majority of cases, the reasons for the formation of kidney stones are unknown. Certain diseases such as gout and urinary tract infections can precipitate the condition. Certain environments can promote kidney stones, for example, hot climates where dehydration can easily occur. Men are affected more than women, as are young people compared to the elderly. Narcotic analgesic and anti-inflammatory medications are commonly used to treat the severe pain that occurs with the passage of kidney stones.
Kidney Failure. There are many conditions that can seriously damage the kidneys and cause them to fail either acutely or chronically. Most kidney diseases attack the nephrons, causing them to lose their ability to filter the blood. Damage to the nephrons can happen quickly, with the kidney function recovering after a few weeks. For example, in acute nephritic syndrome, which can occur after tonsillitis or a certain type of streptococcal bacterial infection, damage to the filtering component of the nephron occurs. This can progress to acute failure of the kidneys if left untreated. However, most kidney diseases (such as diabetic nephropathy, uncontrolled high blood pressure, and polycystic kidney disease) destroy the nephrons slowly and, ultimately, the kidneys fail. This is known as chronic renal failure, and dialysis or kidney transplant is the only cure.
 Many drugs are removed by the kidneys; the dosage of these drugs usually needs to be reduced in the event of kidney failure to prevent harmful effects. Pharmacists often monitor kidney function and recommend dosage adjustments in these cases.
Many drugs are removed by the kidneys; the dosage of these drugs usually needs to be reduced in the event of kidney failure to prevent harmful effects. Pharmacists often monitor kidney function and recommend dosage adjustments in these cases.



