Chapter Twenty-One. The gastrointestinal tract
Introduction
In general, the form in which we eat food is unsuitable for use by the body for growth, repair and energy production. A healthy digestive system is essential to maintaining life by converting the foods we eat into the raw materials necessary to build and fuel our body’s cells. The organs of the digestive system can be divided into two main groups: alimentary canal ( aliment = nourish) and the accessory digestive organs, which include teeth, tongue, salivary glands, liver, gall bladder and pancreas. The alimentary canal, also called the gastrointestinal tract, will be discussed in this chapter followed by significant changes in pregnancy. The accessory organs of salivary glands, liver, gall bladder and pancreas will be discussed fully in Chapter 22 and nutrition in Chapter 23.
Anatomy of the gastrointestinal tract
The adult gastrointestinal tract (GI tract) is a continuous, coiled, fibromuscular tube of variable diameter about 4.5 metres long, open to the external environment at both ends and extending from the mouth to the anus. It varies in structure and function throughout its length. The organs of the GI tract are the mouth, pharynx, oesophagus, stomach, small intestine and large intestine (Fig. 21.1). Readers are referred to a textbook such as Martini & Nath (2009) for detailed anatomy. A brief description is given below.
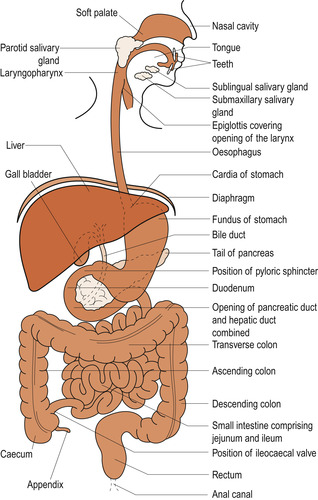 |
| Figure 21.1 Diagrammatic representation of the gastrointestinal tract. (From Hinchliff S M, Montague S E 1990, with permission.) |
The basic structure of the gastrointestinal tract is the same throughout its course. From the oesophagus to the anal canal, the walls of every organ consist of the same four basic layers (Fig. 21.2):
1. The mucosal layer is innermost and lines the tube. This layer is very variable along the length of the tube depending on the required function. The lumen is lined with stratified epithelial cells from which mucus-secreting cells develop. The turnover rate for the epithelial cells is high because of the amount of frictional damage. The epithelial cells are supported by a sheet of connective tissue called the lamina propria, and beneath that is a thin layer of smooth muscle called the muscularis mucosae. The mucosal layer also contains patches of lymphoid tissue, which defend the tract against micro-organisms.
2. The submucosa consists of loose connective tissue that supports blood vessels, lymphatics and nerves. The nerve fibres are called the submucosal or Meissner’s plexus.
3. The muscularis layer is formed of smooth involuntary muscle fibres, bound together in sheets called fasciculi. There are two sheets: an inner circular layer and an outer longitudinal layer. In the stomach there is an additional oblique layer. Between the two layers of muscle fibres is a network of nerve fibres called the myenteric or Auerbach’s plexus. The muscle fibres respond rhythmically to stimulation by the autonomic nervous system and some hormones. They respond slowly and less forcefully than striated muscle fibres and their contractions are not as finely controlled.
4. The adventitia or serosa (visceral peritoneum) is the outermost protective layer and is formed of connective tissue and squamous, serous epithelium. It is continuous with the mesentery of the abdominal cavity and supports blood vessels and nerves.
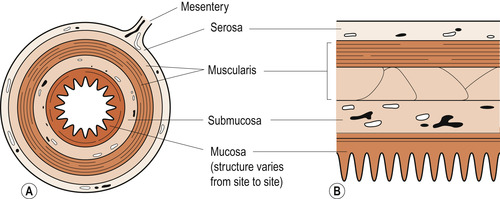 |
| Figure 21.2 Generalised structure of the gut wall. (A) Cross-section. (B) Longitudinal section. (From Hinchliff S M, Montague S E 1990, with permission.) |
The peritoneum
Most of the digestive organs lie in the abdominopelvic cavity. All body cavities contain friction-reducing serous membranes and the peritoneum of the abdominopelvic cavity is the largest of these membranes. The visceral peritoneum covers the external surface of most of the digestive organs and is continuous with the parietal peritoneum that lines the walls of the abdominopelvic cavity. Between the two layers is the peritoneal cavity containing fluid secreted by the serous membranes.
The mesentery
Connecting the visceral and parietal layers of the peritoneum is a fused double layer of peritoneum called the mesentery. This supports the blood vessels, lymphatics and nerves to the digestive organs and helps support the organs. It also stores fat and is able to wall off areas of infection and inflammation to prevent the spread of peritonitis. Another fold of peritoneum, the lesser omentum, runs from the liver to the stomach. The greater omentum is a fold of peritoneum that hangs in front of the intestines and is reflected off the stomach. In most places the mesentery is attached to the posterior abdominal wall. The peritoneum surrounding the small intestine is like a fan with the small intestine attached to its outer edge.
Blood supply
Branches of the abdominal aorta serve the digestive organs and the special hepatic portal circulation. These include the hepatic, splenic and left gastric branches of the coeliac trunk supplying the liver, spleen and stomach and the superior and inferior mesenteric arteries supplying the small and large intestines. The hepatic portal circulation collects nutrient-rich venous blood from the digestive organs and takes it to the liver, as discussed in Chapter 22.
Control of the gastrointestinal tract
Autonomic nervous system
Nerve fibres from the autonomic nervous system (ANS) control the function of the gastrointestinal tract. The submucosal and myenteric nerve plexi are the local tracts. In the submucosal plexus, parasympathetic nerve fibres synapse with ganglion cells present in small clusters in the submucosal tissue. Postganglionic fibres, accompanied by some sympathetic fibres, leave the ganglion cells and send impulses to the glands and smooth muscle of the tract.
In the myenteric plexus parasympathetic nerve fibres synapse with ganglion cells which lie in large clusters between the circular and longitudinal fibres of the muscularis layer. Postganglionic fibres leave the ganglion cells and send impulses to the smooth muscle. Sympathetic fibres also supply this muscle. Both plexi run the length of the gut and receive both sympathetic and parasympathetic nerve fibres. The two plexi are connected and activity in one can affect the other. Stimulation at the upper end of the gastrointestinal tract can be transmitted to more distal parts; for instance, stimulation of gastric and intestinal enzyme secretion follows entry of food into the oesophagus.
Parasympathetic activity leads to an increase in both the motility and secretory functions of the tract and to relaxation of the gut sphincters. The vagus nerve, which is the 10th cranial nerve, is the source of parasympathetic supply to the oesophagus, stomach, pancreas, bile duct, small intestine and proximal colon. The parasympathetic supply to the distal colon is via the nervi erigentes from the sacral outflow.
Sympathetic activity leads to a decrease in blood supply to the gut with a decrease in secretions and in gut motility. There is contraction of the gut sphincters. As in other parts of the body, there are two types of catecholamine receptors in the gut: α and β 2 receptors. Note that β 1 receptors are present only in cardiac muscle. Stimulation of α receptors causes contraction of the smooth muscle of the gastrointestinal tract whereas stimulation of the β 2 receptors causes relaxation.
Regulatory chemicals
Two chemicals produced by the tract help in neural regulation. These are substance P and serotonin:
1. Substance P, a small peptide of only 11 amino acids, is found in high concentrations in the gut and may be a chemical mediator. It acts like a neurotransmitter and is referred to as a regulatory peptide or neuropeptide. It is involved in the conduction of pain impulses but brings about vasodilation and contraction of non-vascular smooth muscle.
2. Serotonin (5-hydroxytryptamine or 5-HT) is synthesised in the myenteric plexus and may also act as an interneuronal transmitter substance.
Functions of the gastrointestinal tract
The role of the gastrointestinal (alimentary) tract is to alter food so that it can be utilised by the body cells. Six processes can be described:
1. Ingestion.
2. Propulsion.
3. Mastication.
4. Mechanical and chemical digestion.
5. Absorption.
6. Elimination of non-usable residues as faeces.
Ingestion and mastication
These two processes take place in the mouth. Food is mixed with saliva, broken into small pieces by the teeth and propelled backwards into the oesophagus by the tongue. The tongue allows us to taste food. On its superior surface are numerous peg-like projections called papillae. These contain most of the 10 000 taste buds, which allow differentiation between the four taste modalities: sweet, sour, salty and bitter (Marieb & Hoehn 2008). All taste buds have the potential for recognising the four tastes, although particular ones are associated with one taste. The four tastes result in different neural firing patterns, which are interpreted in the cerebral cortex. Taste is aided by the sense of smell, which sends impulses to the brain via the olfactory nerve. This is why any inflammation and hypersecretion of the nasal mucosa, which may occur in pregnancy, will result in a loss or alteration of taste.
Saliva
The salivary glands and the production of saliva are discussed more fully in Chapter 22. The three pairs of salivary glands—the parotid, submaxillary and sublingual glands—produce 1.5 L of saliva daily, consisting of 99% water and with a pH 6.75–7.0. Saliva contains the digestive enzyme α-amylase which acts upon cooked starch to convert polysaccharides into disaccharides. It facilitates the formation of a bolus of partly broken up food ready to swallow, once lubricated by salivary mucins. Saliva is produced in response to the cerebral perception of the thought, sight or smell of food or the presence of food in the mouth.
The ingested and masticated food is propelled down the oesophagus into the stomach for digestion of the food to continue. The process is called deglutition. The tongue contracts and presses the bolus of food against the hard palate in the roof of the mouth. It then arches backwards and the bolus of food is propelled into the oropharynx.
The stomach
Chemical breakdown of food by the secretion of enzymes begins in the stomach and is completed in the small intestine. The stomach is 25 cm long and lies in the left side of the abdominal cavity partly hidden by the diaphragm and liver. It is continuous with the oesophagus above and the duodenum below. When empty, it is J-shaped. Its mucosal layer has folds ( rugae) which allow distension. The rugae are further folded, providing a large absorptive surface, and contain millions of deep gastric pits with microscopic gastric glands that produce gastric juice.
Functions of the stomach
• A reservoir for food.
• Production of the intrinsic factor.
• Gastric absorption.
• A churn to mix food.
• Secretion of mucus, hormones and gastric juice.
A reservoir for food
At rest the stomach’s capacity is only 50 ml, but receptive relaxation of the stomach wall musculature can allow distension of up to 1.5 L. Under exceptional circumstances the stomach can hold 4 L of content. The pyloric sphincter prevents a too rapid transfer of food to the small intestine.
Production of the intrinsic factor
The intrinsic factor is a glycoprotein necessary for the absorption of vitamin B 12 (cyanocobalamin) produced by the gastric parietal cells, which also produce gastric acid. Intrinsic factor binds to vitamin B 12 in the terminal ileum of the small intestine to form a complex which appears to bind to receptors in the wall of the ileum and is transferred into the blood. Vitamin B 12 is required for the maintenance of healthy myelin sheaths around the nerves and also for the formation of red blood cells in the bone marrow. Lack of vitamin B 12 may lead to a megaloblastic anaemia. The resulting pernicious anaemia may lead to subacute combined degeneration of the spinal cord.
Gastric absorption
Food that has reached the stomach is only partly broken down there and many of the molecules are still too large to be absorbed. There are also no carrier systems present in the gastric mucosa. Water and some drugs such as aspirin (acetylsalicylic acid), which is a weak acid, can be absorbed from the stomach. Absorption of aspirin lowers intracellular pH and may cause damage, leading to gastric irritation and bleeding.
A churn to mix food
The stomach converts food to a thick soup consistency by mixing it with gastric secretions. This also dilutes the food and makes it compatible with the extracellular fluid in the duodenum. The semiliquid, formed by waves of peristalsis of the smooth muscle in the stomach wall, is called chyme.
Secretion of mucus
Mucus is produced by the cells in the necks of the deep gastric glands in both the cardiac and pyloric sphincters. It adheres to the gastric mucosa to protect the stomach from being digested by the proteolytic gastric enzyme pepsin. The layer of mucus that protects the mucosa must be 1 mm thick.
Secretion of hormones
Enteroendocrine cells release a variety of hormones, which diffuse into blood capillaries and are returned to the GI tract to influence digestive system target organs. These include gastrin, serotonin, cholecystokinin, somatostatin and endorphins. Histamine, produced by circulating mast cells and basophils, increases gastric acid secretion by binding to histamine receptors (H 2 receptors) on the gastric parietal cells (Table 21.1).
| Hormone | Stimulus | Target organ | Effect |
|---|---|---|---|
| Gastrin | Presence of food in the stomach | Stomach | Increased gastric gland secretions, most effect on HCl production |
| Small intestine | Causes contraction of intestinal muscle | ||
| Ileocaecal valve | Relaxes valve | ||
| Large intestine | Stimulates mass movements | ||
| Serotonin | Food in stomach | Stomach | Contraction of stomach musculature |
| Histamine | Food in stomach | Stomach | Release of HCl |
| Somatostatin | Food in stomach | Stomach | Inhibits gastric secretion, motility, emptying |
| Sympathetic nerve stimulus | Pancreas | Inhibits secretion | |
| Small intestine | Inhibits GI blood flow and intestinal absorption | ||
| Gall bladder | Inhibits contraction and bile release | ||
| Intestinal gastrin | Acidic/partly digested food in duodenum | Stomach | Stimulates gastric glands and motility |
| Secretin | Acidic or irritant chyme, partially digested fats and proteins | Stomach | Inhibits gastric secretion and motility during gastric phase |
| Pancreas | Increases bicarbonate-rich pancreatic juice Potentiates CCK action | ||
| Liver | Increases bile output | ||
| Cholecystokinin (CCK) | Fatty chyme or partially digested proteins | Liver/pancreas | Potentiates secretin’s action |
| Gall bladder | Increases enzyme-rich output | ||
| Sphincter of Oddi | Stimulates contraction with expulsion of bile Relaxes to allow bile and pancreatic juice to enter duodenum | ||
| Gastric inhibitory peptide (GIP) | Fatty and/or glucose-containing chyme | Stomach | Inhibits gastric gland secretion and motility during gastric phase |
Secretion of gastric juice
Two to three litres of gastric juice (a mixture of secretions from two types of cells present in the gastric pits but absent from the pylorus) is produced daily (Fig. 21.3). The gastric pit cells are:
1. Parietal or oxyntic cells, which secrete hydrochloric acid (HCl) and the intrinsic factor.
2. Chief or zygomen cells, which secrete the enzymes.
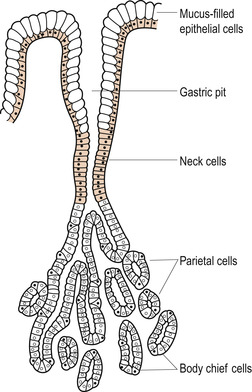 |
| Figure 21.3 Diagram of gastric pit. (From Hinchliff S M, Montague S E 1990, with permission.) |
There are about 1000 million parietal cells in the gastric pits of an adult stomach. Hydrogen ions (H +) are secreted into the lumen of the stomach against a concentration gradient, probably by an active pump mechanism in the cell membrane. Carbon dioxide (CO 2) diffuses into the parietal cells from arterial blood and combines with water to form H 2CO 3 (carbonic acid). Equal numbers of H + ions, formed by the dissociation of H 2CO 3 into H + and bicarbonate ions (HCO 3−), and chloride ions (Cl −) are secreted into the lumen of the gastric pits. They form HCl, which is then diluted by water. Histamine or the hormone gastrin stimulates the secretion of the HCl into the lumen of the stomach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


