Chapter 22 The Extremities and Peripheral Vascular Exam
A. Generalities
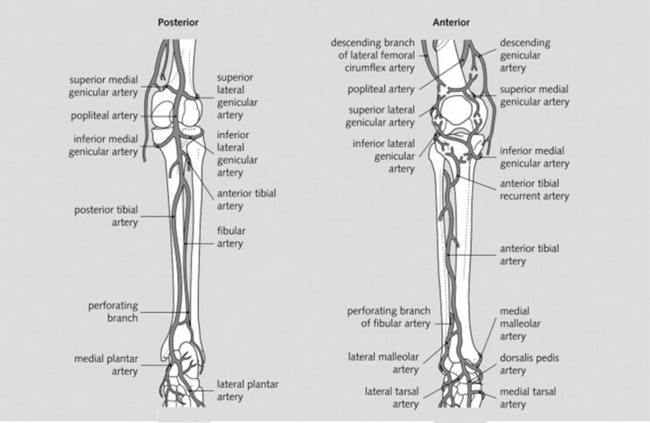
2 Which arteries should be examined in the upper and lower extremities?
The major branches of the brachial and femoral arteries (Figs. 22-1 and 22-2)
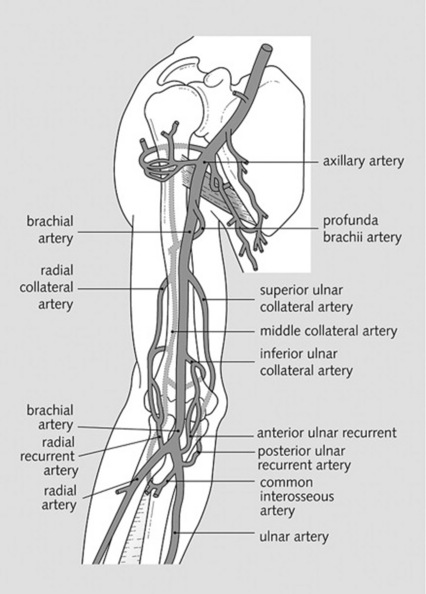
Figure 22-1 Brachial artery and its branches.
(From Granger N: Crash Course Anatomy. St. Louis, Mosby, 2007.)
3 Which veins should be examined?
 id=”u0010″/>For lower extremities, the tributaries of the saphenous system (draining into the femoral vein) (Fig. 22-3)
id=”u0010″/>For lower extremities, the tributaries of the saphenous system (draining into the femoral vein) (Fig. 22-3)
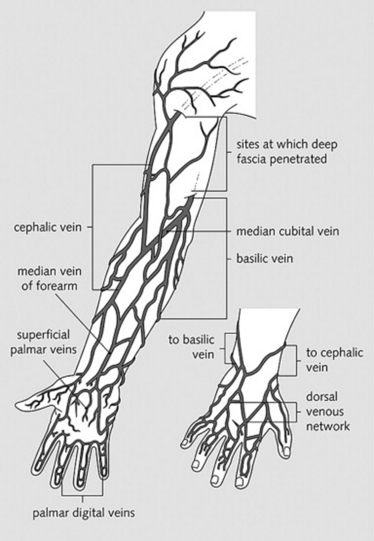
 For upper extremities, the branches of the brachial veins (deep system) and of the basilic and cephalic veins (superficial system), both draining into the axillary vein (Fig. 22-4)
For upper extremities, the branches of the brachial veins (deep system) and of the basilic and cephalic veins (superficial system), both draining into the axillary vein (Fig. 22-4)
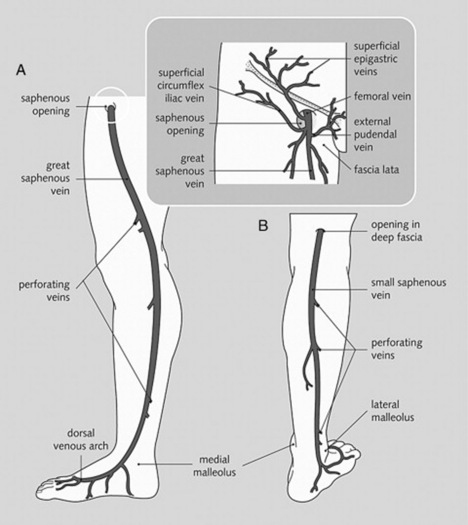
Figure 22-3 Great (A) and small (B) saphenous veins and their tributaries.
(From Granger N: Crash Course Anatomy. St. Louis, Mosby, 2007.)
B. The Peripheral Arteries
(1) Asymmetric Pulses
(2) Raynaud’s Phenomenon
8 What is the clinical significance of Raynaud’s phenomenon?
It can precede several important disorders, including:
 Connective tissue diseases (systemic lupus erythematosus [SLE], mixed connective tissue disease, rheumatoid arthritis, dermatomyositis, and polymyositis, but especially progressive systemic sclerosis, which is present in 17–28% of patients with Raynaud’s)
Connective tissue diseases (systemic lupus erythematosus [SLE], mixed connective tissue disease, rheumatoid arthritis, dermatomyositis, and polymyositis, but especially progressive systemic sclerosis, which is present in 17–28% of patients with Raynaud’s)
 Hematologic disorders (cryoglobulinemia, polycythemia, monoclonal gammopathy)
Hematologic disorders (cryoglobulinemia, polycythemia, monoclonal gammopathy)
 Arterial compression syndromes (thoracic outlet and carpal tunnel syndromes)
Arterial compression syndromes (thoracic outlet and carpal tunnel syndromes)
 Vasculitis and atherosclerotic arterial disease
Vasculitis and atherosclerotic arterial disease
 Recurrent trauma (use of percussion or vibratory tools)
Recurrent trauma (use of percussion or vibratory tools)
 Miscellaneous disorders (hypothyroidism, reflex sympathetic dystrophy, primary pulmonary hypertension, Prinzmetal angina, acromegaly, Addison’s disease). Still, one of five patients with Raynaud’s does not seem to have any underlying disorder (i.e., Raynaud’s disease).
Miscellaneous disorders (hypothyroidism, reflex sympathetic dystrophy, primary pulmonary hypertension, Prinzmetal angina, acromegaly, Addison’s disease). Still, one of five patients with Raynaud’s does not seem to have any underlying disorder (i.e., Raynaud’s disease).
(3) Allen’s Test
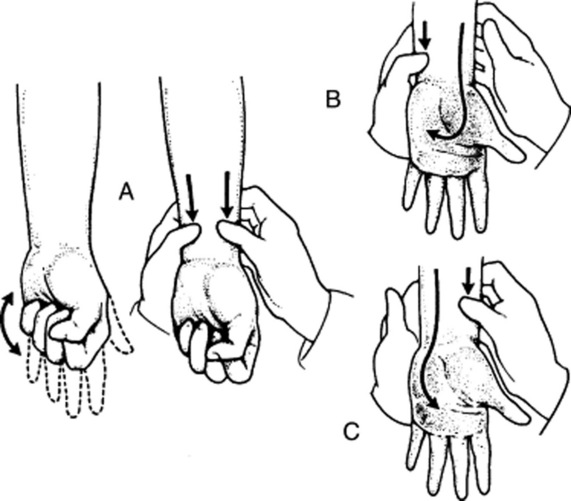
10 What is Allen’s test? What does it mean?
It is a bedside test for patency of the deep palmar arch and of radial/ulnar arteries (Fig. 22-5). Hence, a good way to learn about the risks of radial artery puncture and/or cannulation.
 Compress the patient’s radial artery until blood flow is stopped.
Compress the patient’s radial artery until blood flow is stopped.
 Have the patient clench and unclench the hand several times in sequence until there is a visible blanching of the hand.
Have the patient clench and unclench the hand several times in sequence until there is a visible blanching of the hand.
 When the patient finally relaxes the hand, there will be visible refilling of the capillary bed from the ulnar side, with return of the normal pink color within 5 seconds.
When the patient finally relaxes the hand, there will be visible refilling of the capillary bed from the ulnar side, with return of the normal pink color within 5 seconds.
 Absence of refilling (the pallor persists in spite of the hand’s relaxation) or delay in refilling (return of the color takes longer than 5 seconds) indicates a positive test. This reflects occlusion of either the ulnar artery or the deep palmar arch.
Absence of refilling (the pallor persists in spite of the hand’s relaxation) or delay in refilling (return of the color takes longer than 5 seconds) indicates a positive test. This reflects occlusion of either the ulnar artery or the deep palmar arch.
 Repeat the maneuver on the contralateral hand, comparing size of the refill area and length of refill time.
Repeat the maneuver on the contralateral hand, comparing size of the refill area and length of refill time.
 Finally, repeat the entire sequence, but this time compress the ulnar arteries, first on the right and then on the left.
Finally, repeat the entire sequence, but this time compress the ulnar arteries, first on the right and then on the left.
11 Isn’t the test conducted by simultaneously compressing the ulnar and radial arteries?
Yes, it may be. This is, in fact, a variant of the Allen’s test, conducted as follows (see Fig. 22–5):
 Compress both the radial and ulnar arteries.
Compress both the radial and ulnar arteries.
 Ask the patient to sequentially and vigorously clench/unclench the hand, so as to squeeze all blood out. When the palm finally blanches, ask the patient to relax the hand.
Ask the patient to sequentially and vigorously clench/unclench the hand, so as to squeeze all blood out. When the palm finally blanches, ask the patient to relax the hand.
 Release pressure only on the ulnar artery, and measure the time it takes for the palm to regain its color. This is the refill time for the ulnar artery.
Release pressure only on the ulnar artery, and measure the time it takes for the palm to regain its color. This is the refill time for the ulnar artery.
 If refill is delayed or absent (see question 12), do not attempt a radial puncture, but consider instead either a brachial stick or an arterial puncture on the contralateral hand (after similarly checking the arterial supply, of course).
If refill is delayed or absent (see question 12), do not attempt a radial puncture, but consider instead either a brachial stick or an arterial puncture on the contralateral hand (after similarly checking the arterial supply, of course).
 Repeat the test, but this time release pressure on the radial artery only, thus measuring refill time for that vessel only.
Repeat the test, but this time release pressure on the radial artery only, thus measuring refill time for that vessel only.
(4) Peripheral Vascular Disease
14 Can peripheral pulses be absent in normal individuals?
Yes. Dorsalis pedis and tibialis posterior are undetectable in 10% of healthy subjects. Congenital loss of one of the arteries usually leads to compensatory increases in the other. Still, only fewer than 2% of healthy subjects lack both pedal pulses. Hence, this is usually an important clue to the presence of peripheral vascular disease (see question 16).
16 What are the symptoms of PVD?
Mostly symptoms of arterial insufficiency, such as exertional limb weakness, resting limb pain (or paresthesia), and poor healing of sores or ulcerations. The classic symptom, however, is claudication (from the Latin term for limping)—i.e., intermittent limb pain, usually triggered by activity. This affects different parts of the lower extremity, depending on which artery is compromised. Yet, whether obstruction is high or low, both pedal pulses are absent in PVD, an important diagnostic clue (see Table 22-1).
Table 22-1 Symptoms of Peripheral Vascular Disease
| Above the Knee | Below the Knee |
| PVD of the distal aorta (from below the renal arteries to the common iliacs) will cause claudication of the buttocks, thigh, and calf. It may even compromise erection. Given its high location, all lower extremity pulses will be lost. | Peroneotibial PVD will cause either no symptoms or foot claudication. Only pedal pulses are lost. Except for patients with diabetes and thromboangiitis obliterans, this is the least common form of the disease. |
| Femoropopliteal | |
| PVD will cause calf claudication. Femoral pulses are present, but those beyond are absent. |
18 Can these findings predict severity of the disease?
No. Vascular bruits and other signs only indicate presence of disease; they do not correlate with severity. For severity, the standard assessment is the ankle-to-arm systolic pressure index (see Chapter 2, questions 117–119). Still, in diabetic patients with significantly abnormal ankle–brachial indexes, the following symptoms/signs predict more severe disease: (1) age greater than 65, (2) history of peripheral vascular disease or claudication in less than one block, (3) diminished foot pulses, and (4) venous filling time longer than 20 seconds.
19 What is an increased venous filling time?
It is the abnormally slow (re)filling of foot veins in peripheral vascular disease. To test for it:
1. Ask the patient to lie supine.
2. Identify a prominent vein on top of the foot, and then empty it by raising the patient’s leg to 45 degrees for 1 minute.
3. Ask the patient to sit up and lower the foot over the edge of the examining table.
4. Measure how many seconds it takes the vein to become turgid and visible again. Refill time >20 seconds is abnormal.
20 What is a capillary refill time (CRT)?
A generally accepted bedside method for assessing peripheral perfusion. To test for it:
1. Compress the patient’s skin for 5 seconds (usually over a digit—in cases of the lower extremity, compress the plantar skin of the distal great toe) and with sufficient pressure to cause blanching.
2. Release compression, and measure the time in seconds for the compressed area to regain the color of the surrounding skin. More than 2 seconds for the upper extremities (and 5 seconds for the great toe) are considered abnormal.
21 What is the Buerger’s test?
Another bedside maneuver for assessing arterial perfusion to the leg. It consists of examining the color of the patient’s leg: first when elevated and then when lowered. Hence, it consists of two stages (Table 22-2). The test is considered positive for PVD when it elicits excessive pallor with elevation and intense rubor with dependency.
| Stage I | Stage II |
|---|---|
| 1. Ask the patient to lie supine. | 1. Then ask the patient to sit up, and lower the leg over the edge of the examining table—also at an angle of 90 degrees, and also for 2 minutes. |
| 2. Elevate both legs to an angle of 90 degrees, and hold them up for 2 minutes. | 2. Gravity aids blood flow, so that color eventually returns to the ischemic leg, although the skin usually turns blue first (as blood is deoxygenated in its passage through the ischemic tissue), and then finally acquires a dusky red flush that spreads proximally from the toes as the post-hypoxic vasodilation takes place. |
| 3. Observe the feet. Pallor indicates ischemia (i.e., the inability of peripheral arterial pressure to overcome gravity). | 3. Examine both legs simultaneously because changes are most obvious when one leg has a normal circulation. |
| 4. The poorer the arterial supply, the less the angle to which the legs have to be raised in order to become pale (this was what Buerger originally described as the “angle of circulatory sufficiency”). |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree