Table 10.1)
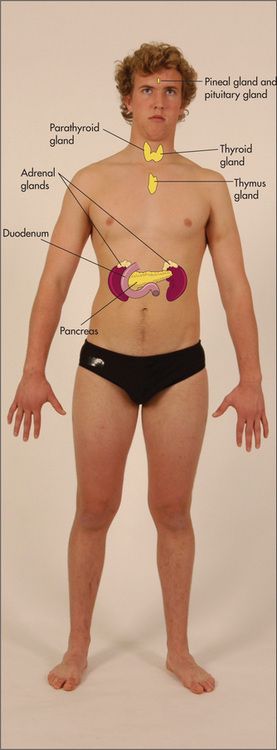
Hormones control so many aspects of body function that the manifestations of endocrine disease are protean. Symptoms can include changes in body weight, appetite, bowel habit, hair distribution, pigmentation, sweating, height and menstruation, galactorrhoea (unexpected breast-milk production—in men and women), as well as polydipsia, polyuria, lethargy, headaches and loss of libido and erectile dysfunction. Many of these symptoms have other causes as well and must be carefully evaluated. On the other hand, the patient may know which endocrine organ or group of endocrine organs has been causing a problem. In particular, there may be a history of a thyroid condition or diabetes mellitus. A list of common symptoms associated with various endocrine diseases is presented in
Changes in appetite and weight
An increased appetite associated with weight loss classically occurs in thyrotoxicosis or uncontrolled diabetes mellitus. An increased appetite with weight gain may occur in Cushing’s syndrome, hypoglycaemia or in hypothalamic disease. A loss of appetite with weight loss can occur with adrenal insufficiency but is also seen in anorexia nervosa and with gastrointestinal disease (particularly malignancy). A loss of appetite with weight gain can occur in hypothyroidism.
Changes in bowel habit
Diarrhoea and an increase in the frequency of bowel movements are associated with hyperthyroidism and adrenal insufficiency, while constipation may occur in hypothyroidism and hypercalcaemia.
Changes in sweating
Increased sweating is characteristic of hyperthyroidism, phaeochromocytoma, hypoglycaemia and acromegaly, but may also occur in anxiety states and at the menopause (
Changes in hair distribution
Hirsutism refers to an increased growth of body hair in women. The clinical evaluation and differential diagnosis are presented on
Lethargy
This common symptom can be due to a number of different diseases. Patients with hypothyroidism, Addison’s disease and diabetes mellitus can present with this problem. Anaemia, connective tissue diseases, chronic infection (e.g. HIV, infective endocarditis), drugs (e.g. sedatives, diuretics causing electrolyte disturbances), chronic liver disease, renal failure and occult malignancy may also result in lethargy. Importantly, depression is a common cause of this symptom (
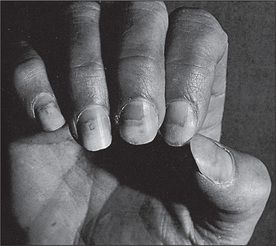
Changes in the skin and nails
The skin becomes coarse, pale and dry in hypothyroidism, and dry and scaly in hypoparathyroidism. Flushing of the skin of the face and neck occurs in the carcinoid syndrome (due to the release of vasoactive peptides from the tumour). Soft-tissue overgrowth occurs in acromegaly and skin tags may appear in the axillae. These are called molluscum fibrinosum. Acanthosis nigricans can also occur in acromegaly and in insulin-resistant states including Cushing’s syndrome and polycystic ovarian syndrome. Xanthelasma can be present in patients with diabetes or hypothyroidism.
Onycholysis occurs in Graves’ disease and Cushing’s syndrome is associated with spontaneous ecchymoses, thin skin and purple striae.
Changes in pigmentation
Increased pigmentation may be reported in primary adrenal insufficiency, Cushing’s syndrome or acromegaly. Decreased pigmentation occurs in hypopituitarism. Localised depigmentation is characteristic of vitiligo, which may be associated with certain endocrine diseases such as Hashimoto’s
Changes in stature
Tallness may occur in children for constitutional reasons (tall parents) or, rarely, may reflect growth hormone excess (leading to gigantism), gonadotrophin deficiency, Klinefelter’s syndrome
Erectile dysfunction (impotence)
A persistent inability to attain or sustain penile erections may occasionally be due to primary hypogonadism or to secondary hypogonadism due to hyperprolactinaemia or hypopituitarism. More often, it is related to emotional disorders. Vascular disease, autonomic neuropathy (e.g. in diabetes mellitus or alcoholism), spinal cord disease or testicular atrophy can also cause this problem.
Galactorrhoea
Hyperprolactinaemia (usually the result of pituitary adenoma) can cause galactorrhoea in up to 80% of women and 30% of men. Galactorrhoea in men occurs from a normal-appearing male breast.
Menstruation
Failure to menstruate is termed amenorrhoea.
Primary amenorrhoea is defined as a failure to start menstruating by 17 years of age. True primary amenorrhoea may result from ovarian failure (e.g. X chromosomal abnormalities such as Turner’s syndrome) or from pituitary or hypothalamic disease (e.g. tumour, trauma or idiopathic disease). Excess androgen production or systemic disease (e.g. malabsorption, chronic renal failure, obesity) can also result in primary amenorrhoea.
Apparent primary amenorrhoea can also occur if menstrual flow cannot escape: for example, if there is an imperforate hymen.
Secondary amenorrhoea is defined as the cessation of menstruation for 6 months or more. Pregnancy and menopause are common causes. The polycystic ovarian syndrome, hyperprolactinaemia, virilising syndromes or hypothalamic or pituitary disease can also result in this problem, as can use of the contraceptive pill or psychiatric disease.
Polyuria
Polyuria is defined as a urine volume of more than 3 litres/day. Patients who report urinary frequency may find it difficult to tell if large volumes of urine are being passed. Causes include diabetes mellitus (due to excessive filtration of glucose, a poorly resorbed solute); diabetes insipidus (due to inadequate renal water conservation from a central deficiency of antidiuretic hormone, or a lack of renal responsiveness to this hormone); primary polydipsia, where a patient drinks excessive water (due to psychogenic or hypothalamic disease or drugs such as chlorpromazine or thioridazine); hypercalcaemia; and tubulointerstitial or cystic renal disease.
Past history
A previous history of any endocrine condition must be uncovered. This includes surgery on the neck for a goitre. A partial thyroidectomy or radio-iodine (131I) treatment in the past can lead to eventual hypothyroidism. The same may apply to radiation of the thyroid for carcinoma. A woman may have been diagnosed with diabetes mellitus after the birth of a large baby. There may be a past history of hypertension, which is occasionally due to an endocrine condition (e.g. phaeochromocytoma, Cushing’s syndrome or Conn’s syndrome). Previous thyroid surgery can be associated with hypoparathyroidism because of surgical damage to the parathyroid glands.
Previous treatment of a patient’s thyroid problems may have included the use of antithyroid drugs, thyroid hormone or radioactive iodine. Surgery on the adrenals or pituitary may have been performed and this may leave the patient with decreased adrenal or pituitary function.
Patients with diabetes mellitus have an important chronic condition (
The patient should be aware of the need for care of the feet and eyes to help prevent complications. Most diabetics have regular ophthalmological review, often using retinal photography. There may be a history of laser treatment for proliferative diabetic retinopathy.
Patients with hypopituitarism or hypoadrenalism may be on glucocorticoid (steroid) replacement; the latter also require mineralocorticoid replacement. Details of the patient’s dosage schedule should be obtained.
Social history
Many of these conditions are chronic and their complications serious. How well the patient copes with various problems and the conditions at home and work will have an important effect on the success of treatment.
Family history
There may be a history in the family of thyroid conditions or diabetes mellitus. Occasionally a family history of a multiple endocrine neoplasia (MEN) syndrome may be obtained. These are rare autosomal-dominant conditions. They include pituitary tumours, medullary carcinoma of the thyroid, hyperparathyroidism, phaeochromocytoma and pancreatic islet cell tumours.
The endocrine examination
A formal examination of the whole endocrine system is set out on
The thyroid
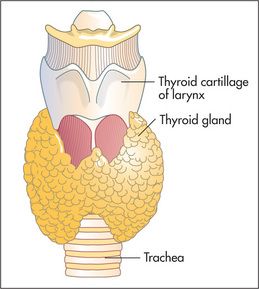
The thyroid gland
Examination anatomy
Even when it is not enlarged, the thyroid (
endocrine gland. Enlargement is common, occurring in 10% of women and 2% of men and more commonly in iodine-deficient parts of the world. The normal gland lies anterior to the larynx and trachea and below the laryngeal prominence of the thyroid cartilage. It consists of a narrow isthmus in the middle line (anterior to the second to fourth tracheal rings and 1.5 cm in size), and two larger lateral lobes each about 4 cm long. Although the position of the larynx varies, the thyroid gland is almost always about 4 cm below the larynx.
Inspection
The normal thyroid may be just visible below the cricoid cartilage in a thin young person (
TABLE 10.2 Causes of neck swellings
| Midline |
| Lateral |
* Aulus Celsus (
GOOD SIGNS GUIDE 10.1 Detection of a goitre (compared with ultrasound findings)
| Sign | Positive LR | Negative LR |
| No goitre on inspection or palpation | 0.4 | — |
| Goitre palpated and visible only on neck extension | NS | — |
| Goitre palpated and visible with neck in normal position | 26.3 | — |
NAS = not significant.
From McGee S, Evidence-based physical diagnosis, 2nd edn. St Louis: Saunders, 2007.
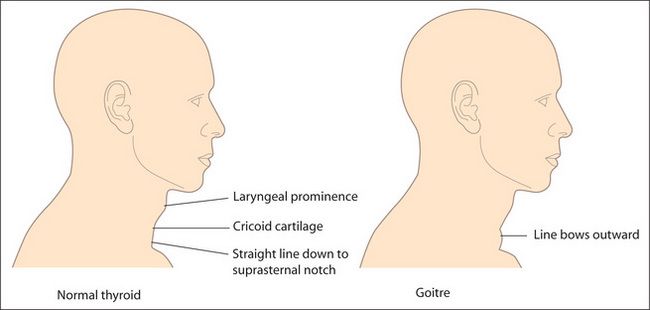
Figure 10.3 The thyroid and goitre
Adapted from McGee S, Evidence-based physical diagnosis, 2nd edition, St Louis, Saunders, 2007.
The temptation to begin touching a swelling as soon as it has been detected should be resisted until a glass of water has been procured. The patient takes sips from this repeatedly so that swallowing is possible without discomfort. Ask the patient to swallow, and watch the neck swelling carefully. Only a goitre or a thyroglossal cyst, because of attachment to the larynx, will rise during swallowing. The thyroid and trachea rise about 2 cm as the patient swallows; they pause for half a second and then descend. Some non-thyroid masses may rise slightly during swallowing but move up less than the trachea and fall again without pausing. A thyroid gland fixed by neoplastic infiltration may not rise on swallowing, but this is rare. Swallowing also allows the shape of the gland to be seen better.
It should be noted whether an inferior border is visible as the gland rises. The thyroglossal cyst is a midline mass that can present at any age. It is an embryological remnant of the thyroglossal duct. Characteristically it rises when the patient protrudes the tongue.
Inspect the skin of the neck for scars. A thyroidectomy scar forms a ring around the base of the neck in the position of a high necklace. Also look for prominent veins. Dilated veins over the upper part of the chest wall, often accompanied by filling of the external jugular vein, suggest retrosternal extension of the goitre (thoracic inlet obstruction). Rarely, redness of the skin over the gland occurs in cases of suppurative thyroiditis.
Palpation
Palpation is best begun from behind (
TABLE 10.3 Differential diagnosis of thyroid nodules
| 1 Carcinoma (5% of palpable nodules)—fixed to surrounding tissues, palpable lymph nodes, vocal cord paralysis, hard, larger than 4 cm (most are, however, smaller than this) |
| 2 Adenoma—mobile, no local associated features |
| 3 Big nodule in a multinodular goitre—palpable multinodular goitre |
Repeat the assessment while the patient swallows
Decide if a thrill is palpable over the gland, as occurs when the gland is unusually metabolically active as in thyrotoxicosis.
Palpate the cervical lymph nodes (
Move to the front. Palpate again. Localised swellings may be more easily defined here. Note the position of the trachea, which may be displaced by a retrosternal gland.
Percussion
The upper part of the manubrium can be percussed from one side to the other. A change from resonant to dull indicates a possible retrosternal goitre, but this is not a very reliable sign.
Auscultation
Listen over each lobe for a bruit (a swishing sound coinciding with systole). This is a sign of increased blood supply which may occur in hyperthyroidism, or occasionally from the use of antithyroid drugs. The differential diagnosis also includes a carotid bruit (louder over the carotid itself) or a venous hum (obliterated by gentle pressure over the base of the neck). If there is a goitre, apply mild compression to the lateral lobes and listen again for stridor.
Pemberton’s sign
Ask the patient to lift both arms as high as possible. Wait a few moments, then search the face eagerly for signs of congestion (plethora) and cyanosis. Associated respiratory distress and inspiratory stridor may occur. Look at the neck veins for distension (venous congestion). Ask the patient to take a deep breath in through the mouth and listen for stridor. This is a test for thoracic inlet obstruction due to a retrosternal goitre or any retrosternal mass.
Examination of the thyroid should be part of every routine physical examination. Causes of a goitre are listed in
| Causes of a diffuse goitre (patient often euthyroid) |
| Causes of a solitary thyroid nodule |
Hyperthyroidism (thyrotoxicosis)
This is a disease caused by excessive concentrations of thyroid hormones. The cause is usually overproduction by the gland but may sometimes be due to accidental or deliberate use of thyroid hormone (thyroxine) tablets; thyrotoxicosis factitia. Thyroxine is sometimes taken by patients as a way of losing weight. The cause may be apparent in these cases if a careful history is taken (

Questions box 10.1
Questions to ask the patient with suspected hyperthyroidism
! denotes symptoms for the possible diagnosis of an urgent or dangerous problem.

Many of the clinical features of thyrotoxicosis are characterised by signs of sympathetic nervous system overactivity such as tremor, tachycardia and sweating. The explanation is not entirely clear. Catecholamine secretion is usually normal in hyperthyroidism; however, thyroid hormone potentiates the effects of catecholamines, possibly by increasing the number of adrenergic receptors in the tissues.
The commonest cause of thyrotoxicosis in young people is Graves’ disease,
Examine a suspected case of thyrotoxicosis as follows (see
GOOD SIGNS GUIDE 10.2 Thyrotoxicosis
| Sign | Positive LR | Negative LR |
| Pulse | ||
| ≥90/min | 4.4 | 0.2 |
| Skin | ||
| Moist and warm | 6.7 | 0.7 |
| Thyroid | ||
| Enlarged | 2.3 | 0.1 |
| Eyes | ||
| Eyelid retraction | 31.5 | 0.7 |
| Lid lag | 17.6 | 0.8 |
| Neurological | ||
| Fine tremor | 11.4 | 0.3 |
From McGee S, Evidence-based physical diagnosis, 2nd edn. St Louis: Saunders, 2007.
General inspection
Look for signs of weight loss, anxiety and the frightened facies of thyrotoxicosis.
The hands
Ask the patient to put out his or her arms and look for a fine tremor (due to sympathetic overactivity). Laying a sheet of paper over the patient’s fingers may more clearly demonstrate this tremor, to the amazement of less-experienced colleagues.
Look at the nails for onycholysis (Plummer’s
Inspect for palmar erythema and feel the palms for warmth and sweatiness (sympathetic overactivity).
Take the pulse. Note the presence of sinus tachycardia (sympathetic overdrive) or atrial fibrillation (due to a shortened refractory period of atrial cells related to sympathetic drive and hormone-induced changes). The pulse may also have a collapsing character due to a high cardiac output.
Test for proximal myopathy and tap the arm reflexes for abnormal briskness, especially in the relaxation phase.
The eyes
Examine the eyes for exophthalmos, which is protrusion of the eyeball from the orbit (
TABLE 10.5 Causes of exophthalmos
| Bilateral |
| Unilateral |
The mechanism of exophthalmos is uncertain. It occurs only in Graves’ disease. It may precede the onset of thyrotoxicosis, or may persist after the patient has become euthyroid. It is characterised by an inflammatory infiltrate of the orbital contents, but not of the globe itself. The orbital muscles are particularly affected, and an increase in their size accounts for most of the increased volume of the orbital contents and therefore for protrusion of the globe. It is probably due to an autoimmune abnormality.
Next examine for the components of thyroid ophthalmopathy, which are related to sympathetic overactivity and are not specific for Graves’ disease. Look for the thyroid stare (a frightened expression) and lid retraction (Dalrymple’s sign
If ptosis is present, one should rule out myasthenia gravis, which can be associated with autoimmune disease.
The neck
Examine for thyroid enlargement, which is usually detectable (60%–90% of patients). In Graves’ disease the gland is classically diffusely enlarged and is smooth and firm. An associated thrill is usually present but this finding is not specific for thyrotoxicosis caused by Graves’ disease. Absence of thyroid enlargement makes Graves’ disease unlikely, but does not exclude it. Possible thyroid abnormalities in patients who are thyrotoxic but do not have Graves’ disease include a toxic multinodular goitre, a solitary nodule (toxic adenoma), and painless, postpartum or subacute (de Quervain’s
If a thyroidectomy scar is present, assess for hypoparathyroidism (Chvostek’s
The chest
Gynaecomastia (
The legs
Look first for pretibial myxoedema. This takes the form of bilateral firm, elevated dermal nodules and plaques, which can be pink, brown or skin-coloured. They are caused by mucopolysaccharide accumulation. Despite the name, this occurs only in Graves’ disease and not in hypothyroidism. Test now for proximal myopathy and hyperreflexia in the legs which is present in only about a quarter of cases.
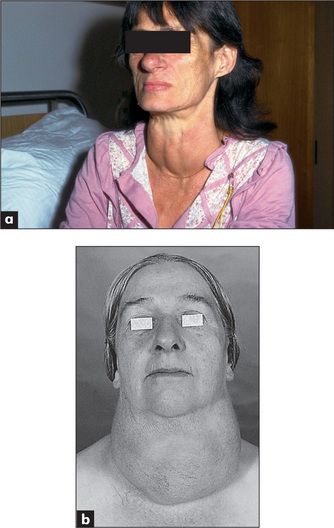
Hypothyroidism (myxoedema)
Hypothyroidism (deficiency of thyroid hormone) is due to primary disease of the thyroid or, less commonly, is secondary to pituitary or hypothalamic failure (
TABLE 10.6 Thyrotoxicosis and hypothyroidism
| Causes of thyrotoxicosis |
| Causes of hypothyroidism |
TSH = thyroid stimulating hormone. HCG = human chorionic gonadotrophin.
* Carl von Basedow (1799–1854), German general practitioner, described this in 1840 (Jod = iodine in German).
The symptoms of hypothyroidism are insidious but patients or their relatives may have noticed cold intolerance, muscle pains, oedema, constipation, a hoarse voice, dry skin, memory loss, depression or weight gain (

Questions box 10.2
Questions to ask the patient with suspected hypothyroidism
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree