Table 9.1)
Peripheral joints
Pain and swelling
The underlying aetiology of joint pain can often be determined by establishing the distribution and duration of joint involvement. Remember, arthralgia is the presence of joint pain without swelling, while with arthritis there is usually pain and swelling. Determine whether one or many joints are involved.
TABLE 9.1 Rheumatological history—major symptoms
It is often useful to ask the patient to point to the painful place or area. For example, pain said to affect the knee may be in the popliteal fossa, the knee joint itself, or in the supra- or infra-patellar bursa. Remember also that pain in the knee or lower thigh may be referred from the hip (
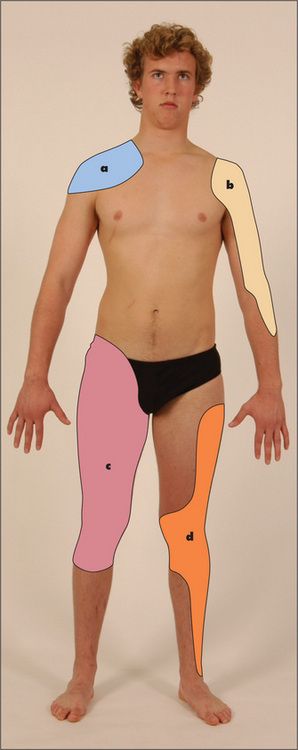
Figure 9.1 Map of referral patterns for different joints
Adapted from Epstein O et al, Clinical Examination, 4th edn. Edinburgh: Mosby, 2008.
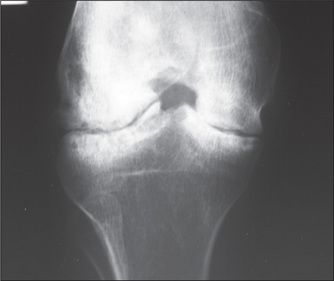
X-ray of the knee showing loss of joint space and some deformity of the adjacent bone. Although the tibia and femur are sclerotic adjacent to the destructive change, the bones are generally osteopenic with mild overgrowth of the epiphysis.
Courtesy Canberra Hospital X-ray library.
Find out if the symptoms are of an acute or chronic nature and whether they are getting better or worse. The effect of rest and exercise on the joint pain should be determined. Patients with rheumatoid arthritis have joint symptoms which are worse after rest, while those with osteoarthritis have pain which is worse after exercise. Ask about the sequence of onset of joint involvement. Precipitating factors such as trauma should be noted. The causes of monoarthritis (single joint) and polyarthritis (more than one joint), and the patterns of polyarthritis in various diseases, are presented in
TABLE 9.2 Causes of monoarthritis
| A single hot red swollen joint (acute monoarthritis) |
| A single chronic inflamed joint (chronic monoarthritis) |
TABLE 9.3 Causes of polyarthritis
TABLE 9.4 Patterns of polyarthropathy
Fingers: distal (Heberden’s nodes) and proximal (Bouchard’s nodes) interphalangeal joints, and metacarpophalangeal joints of the thumbs |
Morning stiffness
Ask about the presence of early-morning stiffness and the length of time that this stiffness lasts. Morning stiffness classically occurs in rheumatoid arthritis and other inflammatory arthropathies, and the duration of stiffness is a guide to its severity. Stiffness after inactivity, such as sitting, is characteristic of osteoarthritis of the hip or knee.
Deformity
The patient may have noticed deformity of a joint or bone. If there has been progressive change in the shape of the area this is more likely to be significant.
Instability
Joint instability may be described by the patient as a ‘giving way’, or occasionally ‘coming out’, of the joint in certain conditions. This may be due to true dislocation (for example, with the shoulder or the patella) or alternatively to muscle weakness or ligamentous problems.
Change in sensation
Change in sensation may occur as a result of nerve entrapment or injury, and sometimes as a result of ischaemia. Ask about numbness or paraesthesiae (pins and needles). The distribution of the change of sensation should help to distinguish nerve damage or entrapment (a specific distribution) from ischaemia.
Back pain
This is a very common symptom. It is most often a consequence of local musculoskeletal disease.
Ask where the pain is situated, whether it began suddenly or gradually, whether it is localised or diffuse, whether it radiates to the limbs or elsewhere, and whether the pain is aggravated by movement, coughing or straining. Musculoskeletal pain is characteristically well localised and is aggravated by movement. If there is a spinal nerve root irritation there may be pain that occurs in a dermatomal distribution. This helps to localise the level of the lesion. Diseases such as osteoporosis (with crush fractures), infiltration of carcinoma, leukaemia or myeloma may cause progressive and unremitting back pain, which is often worse at night (
TABLE 9.6 Alarm features for back pain
| Age > 50 years |
| Cancer history |
| Weight loss (unexplained) |
| Pain on waking from sleep |
| Pain for longer than one month and unresponsive to simple analgesics |
| Fever |
| History of drug use by injection |
| Bowel or bladder dysfunction |
Limb pain
This can occur from disease of the musculoskeletal system, the skin, the vascular system or the nervous system.
Musculoskeletal pain may be due to trauma or inflammation. Muscle disease such as polymyositis can present with an aching pain in the proximal muscles around the shoulders and hips, associated with weakness. Pain and stiffness in the shoulders and hips in patients over the age of 50 years may be due to polymyalgia rheumatica. The acute or subacute onset of symptoms in multiple locations suggests an inflammatory process. Bone disease
TABLE 9.5 Functional assessment in rheumatoid arthritis
| Class | Assessment |
| Class 1 | Normal functional ability |
| Class 2 | Ability to carry out normal activities, despite discomfort or limited mobility of one or more joints |
| Class 3 | Ability to perform only a few of the tasks of the normal occupation or of self-care |
| Class 4 | Complete or almost complete incapacity with the patient confined to wheelchair or to bed |
such as osteomyelitis, osteomalacia, osteoporosis or tumours can cause limb pain. Inflammation of tendons (tenosynovitis) can produce local pain over the affected area.
Vascular disease may also produce pain in the limbs. Acute arterial occlusion causes severe pain of sudden onset, often with coolness or pallor. Chronic peripheral vascular disease can result in calf pain on exercise that is relieved by rest. This is called intermittent claudication. Venous thrombosis can also cause diffuse aching pain in the legs associated with swelling.
Spinal stenosis can cause pseudo-claudication—pain on walking but relieved by leaning forward.
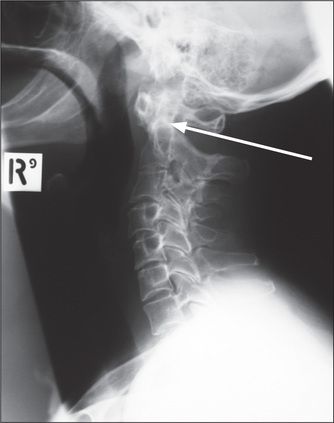
Nerve entrapment and neuropathy can both cause limb pain which is often associated with paraesthesiae or weakness. The usual cause is synovial thickening or joint subluxation—especially for patients with rheumatoid arthritis. The vasculitis associated with the inflammatory arthropathies can also cause neuropathy leading to diffuse peripheral neuropathy or mononeuritis multiplex. Patients with chronic rheumatoid arthritis often develop subluxation of the cervical spine at the atlanto-axial joint. This is caused by erosion of the transverse ligament around the posterior aspect of the odontoid process (dens). The patient may describe shooting paraesthesiae down the arms and an occipital headache. Neck flexion leads to indentation of the cord by the dens and can cause tetraplegia or sudden death. The abnormality may be obvious on lateral X-rays of the cervical spine (
Raynaud’s phenomenon
Raynaud’s phenomenon
TABLE 9.7 Causes of Raynaud’s phenomenon (white-blue-red fingers and toes in response to cold)
Dry eyes and mouth
Dry eyes and dry mouth are characteristic of Sjögren’s syndrome (
TABLE 9.8 Clinical features of Sjögren’s syndrome
| In this syndrome mucus-secreting glands are infiltrated by lymphocytes and plasma cells, which cause atrophy and fibrosis of glandular tissue. |
| 1 Dry eyes: conjunctivitis, keratitis, corneal ulcers (rarely vascularisation of the cornea) |
| 2 Dry mouth |
| 3 Chest: infection secondary to reduced mucus secretion or interstitial pneumonitis |
| 4 Kidneys: renal tubular acidosis or nephrogenic diabetes insipidus |
| 5 Genital tract: atrophic vaginitis |
| 6 Pseudolymphoma: lymphadenopathy and splenomegaly, which may rarely progress to a true (usually non-Hodgkin’s) lymphoma |
Note: This syndrome occurs in rheumatoid arthritis and with the connective tissue diseases.
Red eyes
The seronegative spondyloarthropathies and Behçet’s
Systemic symptoms
A number of other symptoms may occur with specific rheumatological diseases. Fatigue is common with connective tissue disease. Weight loss and diarrhoea may occur with scleroderma, because of small-bowel bacterial overgrowth. Mucosal ulcers are common in some connective tissue diseases such as systemic lupus erythematosus (SLE). Specific rashes can also occur. Generalised stiffness can be due to rheumatoid arthritis or scleroderma, but other causes include systemic infection (e.g. influenza), excessive exercise, polymyalgia rheumatica, neuromuscular disease (e.g. extrapyramidal disease, tetanus, myotonia, dermatomyositis) and hypothyroidism. Finally, on occasion fever may be associated with the connective tissue diseases, especially SLE, but infection should always be excluded.
Treatment history
Document current and previous anti-arthritic medications (e.g. aspirin, other non-steroidal anti-inflammatory drugs, gold, methotrexate, penicillamine, chloroquine, steroids, anti-tumour necrosis factor α therapy, or other biological agents). Any side-effects of these drugs (e.g. gastric ulceration or haemorrhage, from aspirin) also need to be identified. Ask about physiotherapy and joint or tendon surgery in the past.
Past history
It is important to inquire about any history of trauma or surgery in the past. Similarly, a history of recent infection, including hepatitis, streptococcal pharyngitis, rubella, dysentery, gonorrhoea and tuberculosis, may be relevant to the onset of arthralgia or arthritis. A history of tick bite may indicate that the patient has Lyme disease. Inflammatory bowel disease can be associated with arthritis, as described on
Social history
Determine the patient’s domestic set-up and occupation. This is particularly relevant if a chronic disabling arthritis has developed. Any history of sexually transmitted disease in the past is important, but non-specific urethritis and gonorrhoea are especially relevant.
Family history
Some diseases associated with chronic arthritis run in families. These include rheumatoid arthritis, gout and primary osteoarthritis, haemochromatosis, the seronegative spondyloarthropathies and inflammatory bowel disease. A family history of bleeding disorder may explain an acutely swollen tender joint in a boy (haemophilia).
Examination anatomy
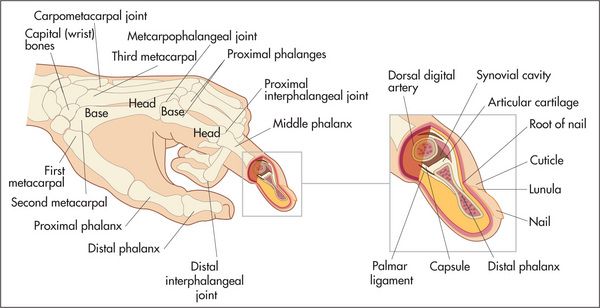
Joint structures (
Inflammatory arthritis affects first the joint synovium. Thickening of this may be palpable and is called pannus. Later, destruction of surrounding structures including tendons, articular cartilages and the bone itself occur.
Joint pain may be well localised if there is inflammation close to the skin, but deeper joint abnormalities may cause pain to be referred. The areas where joint pain is felt correspond to the innervation of the muscle attached to that joint—the myotome. For example, the glenohumeral joint of the shoulder and the posterior scapular muscles are supplied from C5 and C6, so pain over the shoulder or scapula may arise from any structure supplied from these nerve roots—including the shoulder muscles and joints but also the C5 and C6 segments of the spine.
The extra-articular structures that surround a joint—the ligaments, tendons and nerves—may also be the source of joint pain. Disease of the joint itself tends to limit movement of the joint in all directions, both active movement (moved by the patient) and passive movement (moved by the examiner). Extra-articular disease causes variable limitation of movement in different directions, and tends to cause more limitation of active than of passive movement.
The rheumatological examination
There are certain established ways of examining the joints and related structures
General inspection
This is important for two reasons: first, it gives an indication of the patient’s functional disability, which is essential in all rheumatological assessments; and second, certain conditions can be diagnosed by careful inspection. Look at the patient as he or she walks into the room. Does walking appear to be painful and difficult? What posture is taken? Does the patient require assistance such as a stick or walking frame? Is there obvious deformity, and what joints does it involve? Note the pattern of joint involvement, which gives a clue about the likely underlying disease (
For a more detailed examination the patient should be undressed as far as practical, usually to the underclothes. Depending on the patient’s condition and the parts of the body to be examined, the examination may best be begun with the patient in bed, or sitting over the side of the bed or in a chair, or standing. The opportunity of watching the patient remove the clothes should not be lost because arthritis can interfere with this essential daily task.
Principles of joint examination
Certain general rules apply to the examination of all the joints and they can be summarised as: look, feel, move, measure, and compare with the opposite side.
Look
The first principle is always to compare right with left. Remember that joints are three-dimensional structures and need to be inspected from the front, the back and the sides. The skin is inspected for erythema indicating underlying inflammation and suggesting active, intense arthritis or infection, atrophy suggesting chronic underlying disease, scars indicating previous operations such as tendon repairs or joint replacements, and rashes. For example, psoriasis is associated with a rash and polyarthritis (inflammation of more than one joint). The psoriatic rash consists of scaling erythematous plaques on extensor surfaces. The nails are often also affected (
A small, firm, painless swelling over the back (dorsal surface) of the wrist is usually a synovial cyst—a ganglion.
Note any swelling over the joint. There are a number of possible causes: these include effusion into the joint space, hypertrophy and inflammation of the synovium (e.g. rheumatoid arthritis), or bony overgrowths at the joint margins (e.g. osteoarthritis). It may also occur when tissues around the joints become involved, as with the tendinitis or bursitis of rheumatoid arthritis. Swelling of the lower legs may be due to fluid retention, which is painless and can occur in association with inflammation anywhere in the leg. Painful swelling may result from inflammation of the ankle joints or tendons, or of the fascia, or from inflammatory oedema of the skin and subcutaneous tissue.
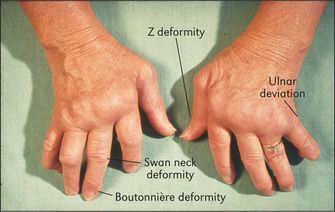
Deformity is the sign of a chronic, usually destructive, arthritis, and ranges from mild ulnar deviation of the metacarpophalangeal joints in early rheumatoid arthritis to the gross destruction and disorganisation of a denervated (Charcot’s
Look for abnormal bone alignment. Subluxation is said to be present when displaced parts of the joint surfaces remain partly in contact. Dislocation is used to describe displacement where there is loss of contact between the joint surfaces.
Muscle wasting results from a combination of disuse of the joint, inflammation of the surrounding tissues and sometimes nerve entrapment. It tends to affect muscle groups adjacent to the diseased joint (e.g. quadriceps wasting with active arthritis of the knee) and is a sign of chronicity.
Feel
Palpate for skin warmth. This is done traditionally with the backs of the fingers where temperature appreciation is said to be better. A cool joint is unlikely to be involved in an acute inflammatory process. A swollen and warm joint may be affected by active synovitis (see below), infection (e.g. Staphylococcus) or crystal arthritis (e.g. gout).
Tenderness is a guide to the acuteness of the inflammation, but may be present over the muscles of patients with fibromyalgia. The patient must be told to let the examiner know if the examination is becoming uncomfortable. Tenderness can be graded as follows:
This may result from joint inflammation or from lesions outside the joints (periarticular tissues), including inflamed tendons, bursae, or attachments (entheses). Infected joints are extremely tender and patients will often not let the examiner move the joint at all. Palpation of a joint or area for tenderness must be performed gently, and the patient’s face rather than the joint itself should be watched for signs that the examination is uncomfortable.
Palpate the joint deliberately now, if possible, for evidence of synovitis, which is a soft and spongy (boggy) swelling. This must be distinguished from an effusion, which tends to affect large joints but can occur in any joint. Here the swelling is fluctuant and can be made to shift within the joint. Bony swelling feels hard and immobile, and suggests osteophyte formation or subchondral bone thickening.
Move
Much information about certain joints is gained by testing the range of passive movement. (Passive movement is obviously contraindicated in cases of recent injury to the limb or joint, such as a suspected fracture.) The patient is asked to relax and let the examiner move the joint. This must be attempted gently and will be limited if the joint is painful (secondary to muscle spasm), if a tense effusion is present, if there is capsular contraction or if there is a fixed deformity. The joints may have limited extension (called fixed flexion deformity) or limited flexion (fixed extension deformity). Passive movement of the spine is not a practical manoeuvre (unless the examiner is very strong), and active movement is tested here. Active movement is more helpful in assessing integrated joint function. Hand function and gait are usually applied as tests of function. Pain on motion indicates a joint or periarticular problem.
Stability of the joint is important and depends largely on the surrounding ligaments. This is tested by attempting to move the joint gently in abnormal directions to its usual limits, set by ligaments and muscular tone.
Joint crepitus, which is a grating sensation or noise from the joint, indicates irregularity of the articular surfaces. Its presence suggests chronicity.
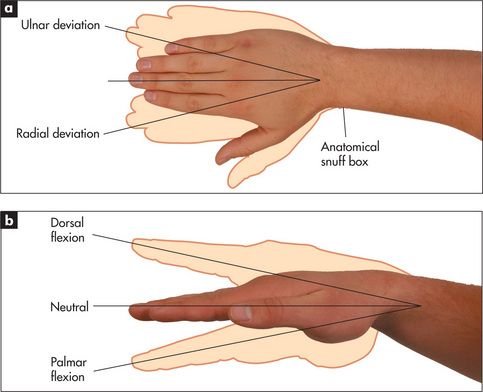
Measure
Accurate measurement of the range of movement of a joint is possible with a goniometer, which is a hinged rod with a protractor in the centre. The jaws are opened and lined up with the joint. Measurement of joint movements is performed from the zero starting position. For most joints this is the anatomical position in extension—e.g. the straightened knee. Movement is then recorded as the number of degrees of flexion from this position. A knee with a fixed flexion deformity may be recorded as ‘30 to 60 degrees’, which indicates that there is 30 degrees of fixed flexion deformity and that flexion is limited to 60 degrees. At some joints both flexion and extension from the anatomical position can be measured, as at the wrists. The goniometer is not routinely used by non-rheumatologists and there is a wide range of normal values for joint movement. Most clinicians estimate the approximate joint angles.
A tape measure is useful for measuring and following serially the quadriceps muscle bulk and in examination of spinal movements.
Assessment of individual joints
The hands and wrists (
Examination anatomy
The articulations between the phalanges are synovial hinge joints. The eight bones of the wrist (carpal bones) form gliding joints which allow wrist movements—flexion/extension and abduction/adduction as they slide over each other.

Figure 9.5 Examination of the hands and wrists
Sitting up (hands on a pillow)

Figure 9.6 (right) X-ray of normal hand
Courtesy M Thomson, National Capital Diagnostic Imaging, Canberra.

Figure 9.7 Rheumatoid arthritis, early findings
X-ray of the hands of a patient with early rheumatoid arthritis. Note erosions of the heads of the metacarpophalangeal joints and of the ulnar styloid, and reduced amounts of cartilage in the joint spaces.
Courtesy Canberra Hospital X-ray library.

Figure 9.8 Rheumatoid arthritis, late findings
X-ray of the hands of a patient with advanced rheumatoid arthritis. Note loss of joint space and destruction of the right carpal joints, subluxation of metacarpophalangeal and poximal interphalangeal (PIP) joints, and Z deformity of the thumb. There are erosions of the PIP joints, a sign of active disease.
Courtesy Canberra Hospital X-ray library.

Figure 9.9 Osteoarthritis arthritis
X-ray of the hands showing the typical findings of osteoarthritis with joint-space narrowing and proliferative changes in the distal joints. Also note erosive and destructive changes at multiple proximal interphalangeal joints.
Courtesy Canberra Hospital X-ray library.
History
Pain may be present in some or all of the joints. It is more likely to be vague or diffuse if it has radiated from the shoulder or neck or is due to carpal tunnel syndrome, and to be localised if it is due to arthritis. Stiffness is typically worse in the mornings in rheumatoid arthritis. Swelling of the wrist may indicate arthritis or tendon sheath inflammation. Swelling of individual joints suggests arthritis. Deformity of the fingers and hand due to rheumatoid arthritis or of the fingers as a result of arthritis or gouty tophi may be the presenting complaint. The sudden onset of deformity suggests tendon rupture. Locking or snapping of a finger (trigger finger) is typical of inflammation of a flexor tendon sheath (tenovaginitis). Loss of function is a serious problem when it involves the numerous functions of the hand and wrist. The history should include an assessment of the difficulties the patient has in using the hands and wrists. Neurological symptoms as a result of nerve compression may cause paraesthesiae or limitation of strength or of complicated hand functions.
Examination
First sit the patient over the side of the bed and place the hands on the pillow with palms down. Often examination of the hands alone will give enough information for the examiner to make a diagnosis. As a result this is quite a popular test in viva voce examinations.
Look
Start the examination at the wrists and forearms. Inspect the skin for erythema, atrophy, scars and rashes. Look for swelling and its distribution. Next look at the wrist for swelling, deformity, ulnar and hyloid prominence. Then look for muscle wasting of the intrinsic muscles of the hand. This results in the appearance of hollow ridges between the metacarpal bones. It is especially obvious on the dorsum of the hand.
Go on to the metacarpophalangeal joints. Again note any skin abnormalities, swelling or deformity. Look especially for ulnar deviation and volar (palmar) subluxation of the fingers. Ulnar deviation is deviation of the phalanges at the metacarpophalangeal joints towards the medial (ulnar) side of the hand. It is usually associated with anterior (Volar) subluxation of the fingers (
TABLE 9.9 Differential diagnosis of a deforming polyarthropathy
| Rheumatoid arthritis |
| Seronegative spondyloarthropathy, particularly psoriatic arthritis, ankylosing spondylitis or Reiter’s disease |
| Chronic tophaceous gout (rarely symmetrical) |
| Primary generalised osteoarthritis |
| Erosive or inflammatory osteoarthritis |
Next inspect the proximal interphalangeal and distal interphalangeal joints. Again note any skin changes and joint swelling. Look for the characteristic deformities of rheumatoid arthritis. These include swan neck and boutonnière deformity of the fingers and Z deformity of the thumb (
Now look for the characteristic changes of osteoarthritis (
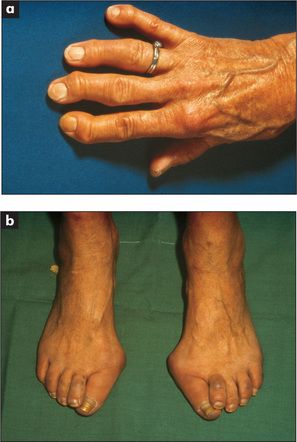
Figure 9.11 The hands (a) and the feet (b) of a patient with osteoarthritis
Showing Heberden’s nodes (distal interphalangeal joints), Bouchard’s nodes (proximal interphalangeal joints) and bunions.
Look also to see if the phalanges appear sausage-shaped. This is characteristic of psoriatic arthropathy, but can also occur in patients with Reiter’s disease. It is due to interphalangeal arthritis and flexor tendon sheath oedema. Finger shortening due to severe destructive arthritis also occurs in psoriatic disease and is called arthritis mutilans. The hand may take up a main en lorgnette (‘hand holding long-handled opera glasses’) appearance due to a combination of shortening and telescoping of the digits.
Now examine the nails. Characteristic psoriatic nail changes may be visible: these include pitting (small depressions in the nail), onycholysis (
The hands should now be turned over and the palmar surfaces revealed. Look at the palms for scars (from tendon repairs or transfers), palmar erythema, and muscle wasting of the thenar or hypothenar eminences (due to disuse, vasculitis or peripheral nerve entrapment). Telangiectasia here would support the diagnosis of scleroderma.
Feel and move
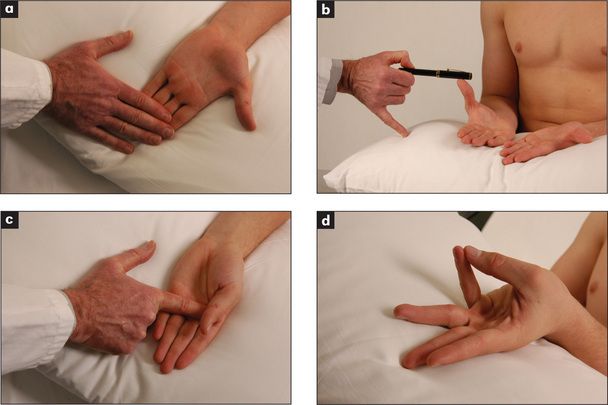
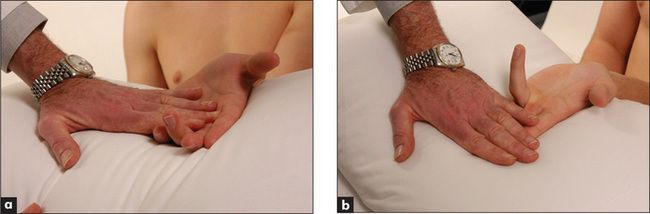
Turn the hands back again to the palm-down position. Palpate the wrists with both thumbs placed on the dorsal surface by the wrists, supported underneath by the index fingers (
Test for tenderness at the tip of the radial styloid. This suggests de Quervain’s
Feel for tenderness in the anatomical snuff box if scaphoid injury is suspected (
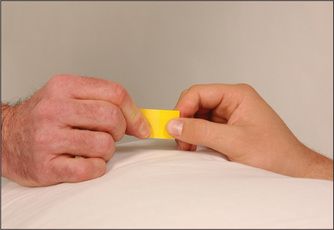
Go on now to the metacarpophalangeal joints, which are palpated in a similar way with the two thumbs. Again passive movement is tested. Volar subluxation can be demonstrated by flexing the metacarpophalangeal joint with the proximal phalanx held between the thumb and forefinger. The metacarpophalangeal joint is then rocked backwards and forwards (
Palpate the proximal and distal interphalangeal joints for tenderness, swelling and osteophytes.
Next test for palmar tendon crepitus. The palmar aspects of the examiner’s fingers are placed against the palm of the patient’s hand while he or she flexes and extends the metacarpophalangeal joints. Inflamed palmar tendons can be felt creaking in their thickened sheaths and nodules can be palpated. This indicates tenosynovitis.
A trigger finger may also be detected by this manoeuvre. Here the thickening of a section of digital flexor tendon is such that it tends to jam when passing through a narrowed part of its tendon sheath. Rheumatoid arthritis is an important cause. Typically, flexion of the finger occurs freely up to a certain point where it sticks and cannot be extended (as flexors are more powerful than extensors). The application of greater force overcomes the resistance with a snap.
If the carpal tunnel syndrome is suspected, ask the patient to flex both wrists for 30 seconds—paraesthesiae will often be precipitated in the affected hand if the syndrome is present (Phalen’s
TABLE 9.10 Causes of carpal tunnel syndrome
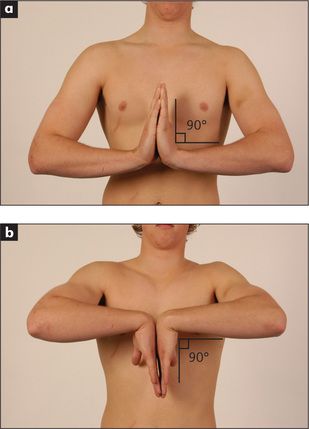
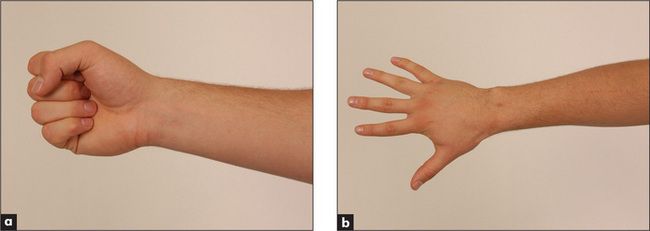
Now test active movements. First assess wrist flexion and extension as shown in
Function
It is important to test the function of the hand. Grip strength is tested by getting the patient to squeeze two of the examiner’s fingers. Even an angry patient will rarely cause pain if given only two fingers. Serial measurements of grip strength can be made by asking the patient to squeeze a partly inflated sphygmomanometer cuff and noting the pressure reached. Key grip (
Tests of hand function should be completed by formally assessing for neurological changes (
Examination of the hands is not complete without feeling for the subcutaneous nodules of rheumatoid arthritis near the elbows (
TABLE 9.11 Causes of arthritis plus nodules
| Rheumatoid arthritis |
| Systemic lupus erythematosus (rare) |
| Rheumatic fever (Jaccoud’s |
| Granulomas—e.g. sarcoidosis (very rare) |
* Gouty tophi and xanthomata from hyperlipidaemia may cause confusion.
† François Jaccoud (1830–1913), professor of medicine, Geneva.
The elbows
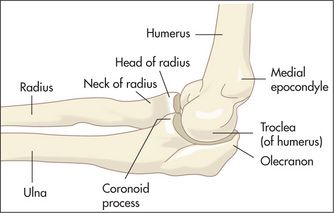
Examination anatomy (
The humerus, radius and ulna meet at the elbow, which is a hinge and a pivot joint. Pivoting occurs between the radius and ulna, and the articulation between all three bones forms a hinge joint.
History
Pain from the elbow is usually diffuse and may radiate down the forearm. It may occur over the lateral or medial epicondyle if the patient has tendinitis (tennis or golfer’s elbow). The patient may have noticed some swelling as a result of inflammation. Swelling over the back suggests olecranon bursitis. Stiffness may interfere with elbow movements and the patient may complain of difficulty combing the hair. When supination and pronation are affected the patient may complain of difficulty with carrying and holding. If the patient is aware of the elbow moving abnormally this suggests instability of the joint and may be a result of rheumatoid arthritis or trauma. Ulnar nerve trauma at the elbow may lead to a complaint of numbness or paraesthesiae in the distribution of that nerve.
Examination
Watch as the patient undresses, for difficulty disentangling the arms from clothing. The upper arms should be exposed completely. Note any deformity or difference in the normal 5–10 degree valgus position (carrying angle) as the patient stands with the palms facing forward.
Look for a joint effusion, which appears as a swelling on either side of the olecranon. Discrete swellings over the olecranon or over the proximal subcutaneous border of the ulna may be due to rheumatoid nodules, gouty tophi, an enlarged olecranon bursa or, rarely, to other types of nodules (
Feel for tenderness, particularly over the lateral and medial epicondyles which may indicate tennis or golfer’s elbow, respectively. Palpate any discrete swellings. Rheumatoid nodules are quite hard, may be tender and are attached to underlying structures. Gouty tophi have a firm feeling and often appear yellow under the skin, but are sometimes difficult to distinguish from rheumatoid nodules. A fluid collection in the olecranon bursa is softly fluctuant and may be tender if inflammation is present. These collections are associated with rheumatoid arthritis and gout, but often occur independently of these diseases.
Small amounts of fluid or synovitis of the elbow joint may be detected by the examiner, facing the patient, placing the thumb of the opposite hand along the edge of the ulnar shaft just distal to the olecranon where the synovium is closest to the surface. Full extension of the elbow joint will cause a palpable bulge in this area if fluid is present.
Move the elbow joints passively. The elbow is a hinge joint. The zero position is when the arm is fully extended (0 degrees). Normal flexion is possible to 150 degrees. Limitation of extension is an early sign of synovitis.
If lateral epicondylitis is suspected, ask the patient to extend the wrist actively against resistance (see
The shoulders
Examination anatomy (
The shoulder joint includes the clavicle, scapula and humerus. The acromioclavicular joint is formed by the acromion of the scapula and the clavicle. Movements of the shoulder are a result of a combination of ball-and-socket articulation at the glenohumeral joint (between the glenoid cavity of the scapula and the ball-shaped end of the humerus) and motion between the scapula and the thorax. It is the most mobile joint in the body. The joint is encased in a capsule and is lined with synovium.
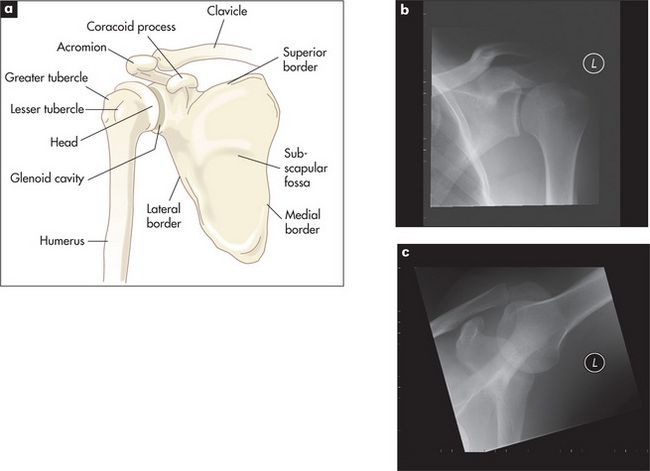
Figure 9.25 Examination of the shoulders
(a) Anatomy of the shoulder. (b) X-ray of left shoulder in the neutral position; the relative positions of the humeral head, clavicle and scapulae can be seen. (c) X-ray of left shoulder in abduction. Abduction of the arm rotates the head of the humerus and the clavicle moves upwards.
X-rays courtesy M Thomson, National Capital Diagnostic Imaging, Canberra.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree