Chapter 9
The endocrine system
Pituitary gland and hypothalamus
Organs with secondary endocrine functions
The effects of ageing on endocrine function
Disorders of the pituitary gland
Disorders of the thyroid gland
Disorders of the parathyroid glands
Disorders of the adrenal cortex
Disorders of the adrenal medulla
Disorders of the pancreatic islets
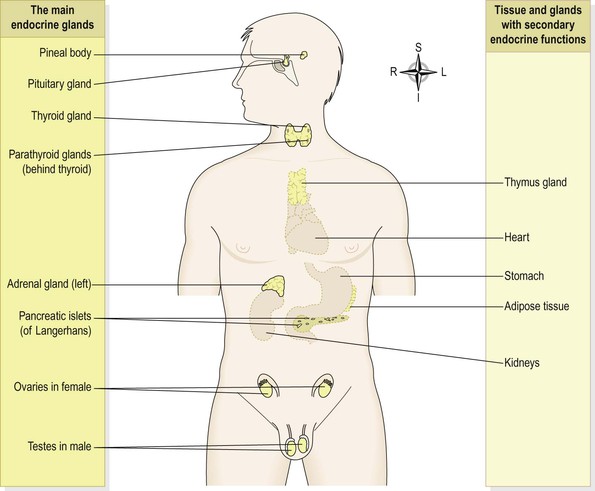
The endocrine system consists of glands widely separated from each other with no physical connections (Fig. 9.1). Endocrine glands are groups of secretory cells surrounded by an extensive network of capillaries that facilitates diffusion of hormones (chemical messengers) from the secretory cells into the bloodstream. They are also referred to as ductless glands because hormones diffuse directly into the bloodstream. Hormones are then carried in the bloodstream to target tissues and organs that may be quite distant, where they influence cell growth and metabolism.
Homeostasis of the internal environment is maintained partly by the autonomic nervous system and partly by the endocrine system. The autonomic nervous system is concerned with rapid changes, while endocrine control is mainly involved in slower and more precise adjustments.
Although the hypothalamus is classified as a part of the brain rather than an endocrine gland, it controls the pituitary gland and indirectly influences many others.
The ovaries and the testes secrete hormones associated with the reproductive system after puberty; their functions are described in Chapter 18. The placenta that develops to nourish the developing fetus during pregnancy also has an endocrine function, which is outlined in Chapter 5. In addition to the main endocrine glands shown in Figure 9.1 many other organs and tissues also secrete hormones as a secondary function e.g. adipose tissue produces leptin (p. 284), involved in the regulation of appetite; the heart secretes atrial natriuretic peptide (ANP, p. 99) that acts on the kidneys. Other hormones do not travel to remote organs but act locally e.g. prostaglandins.
The endocrine glands are explored in the early sections of the chapter. Some local hormones are considered briefly on page 229. Changes in endocrine functions that accompany ageing are explored. Problems that arise when abnormalities occur are usually caused by the over- or under-activity of endocrine glands and are explained in the final sections of this chapter.
Overview of hormone action
When a hormone arrives at its target cell, it binds to a specific receptor, where it acts as a switch influencing chemical or metabolic reactions inside the cell. Receptors for peptide hormones are situated on the cell membrane and those for lipid-based hormones are located inside cells. Examples are shown in Box 9.1. ![]() 9.1
9.1
The level of a hormone in the blood is variable and self-regulating within its normal range. A hormone is released in response to a specific stimulus and usually its action reverses or negates the stimulus through a negative feedback mechanism (see p. 6). This may be controlled either indirectly through the release of hormones by the hypothalamus and the anterior pituitary gland, e.g. steroid and thyroid hormones, or directly by blood levels of the stimulus, e.g. insulin and glucagon and determined by plasma glucose levels.
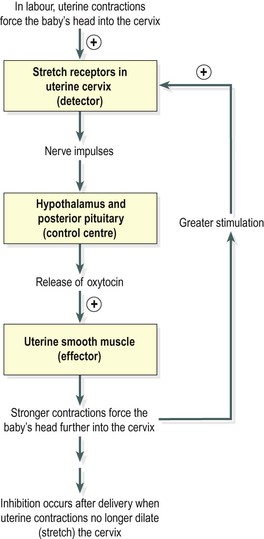
The effect of a positive feedback mechanism is amplification of the stimulus and increasing release of the hormone until a particular process is complete and the stimulus ceases, e.g. release of oxytocin during labour (p. 7).
Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus act as a unit, regulating the activity of most of the other endocrine glands. The pituitary gland lies in the hypophyseal fossa of the sphenoid bone below the hypothalamus, to which it is attached by a stalk (Fig. 9.2). It is the size of a pea, weighs about 500 mg and consists of two main parts that originate from different types of cells. The anterior pituitary (adenohypophysis) is an upgrowth of glandular epithelium from the pharynx and the posterior pituitary (neurohypophysis) a downgrowth of nervous tissue from the brain. There is a network of nerve fibres between the hypothalamus and the posterior pituitary.
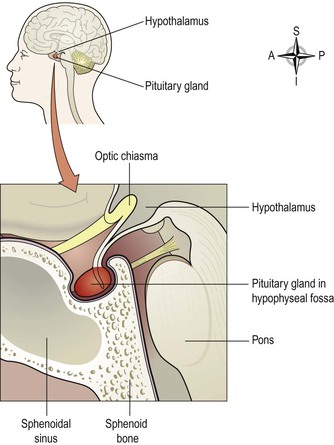
Figure 9.2 Median section showing the position of the pituitary gland and its associated structures.
Blood supply
Arterial blood.
This is from branches of the internal carotid artery. The anterior lobe is supplied indirectly by blood that has already passed through a capillary bed in the hypothalamus but the posterior lobe is supplied directly.
Venous drainage.
Containing hormones from both lobes, venous blood leaves the gland in short veins that enter the venous sinuses between the layers of dura mater.
The influence of the hypothalamus on the pituitary gland
The hypothalamus controls release of hormones from both the anterior and posterior pituitary but in different ways (see below).
Anterior pituitary
The anterior pituitary is supplied indirectly with arterial blood that has already passed through a capillary bed in the hypothalamus (Fig. 9.3A). This network of blood vessels forms part of the pituitary portal system, which transports blood from the hypothalamus to the anterior pituitary where it enters thin-walled sinusoids that are in close contact with the secretory cells. As well as providing oxygen and nutrients, this blood transports releasing and inhibiting hormones secreted by the hypothalamus. These hormones specifically influence secretion and release of other hormones formed in the anterior pituitary (Table 9.1).
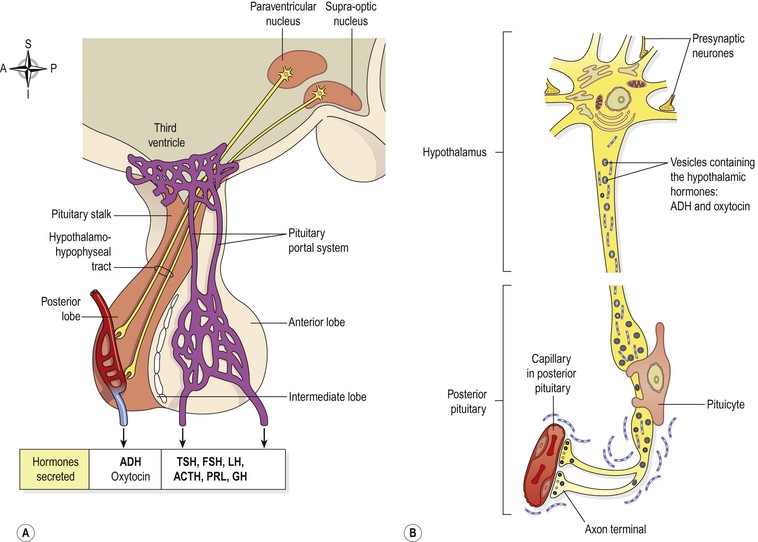
Figure 9.3 The pituitary gland. A. The lobes of the pituitary gland and their relationship with the hypothalamus. B. Synthesis and storage of antidiuretic hormone and oxytocin.
Table 9.1
Hormones of the hypothalamus, anterior pituitary and their target tissues
| Hypothalamus | Anterior pituitary | Target gland or tissue |
| GHRH | GH | Most tissues |
| Many organs | ||
| GHRIH | GH inhibition | Thyroid gland |
| TSH inhibition | Pancreatic islets | |
| Most tissues | ||
| TRH | TSH | Thyroid gland |
| CRH | ACTH | Adrenal cortex |
| PRH | PRL | Breast |
| PIH | PRL inhibition | Breast |
| LHRH or | FSH | Ovaries and testes |
| GnRH | LH | Ovaries and testes |
GHRH = growth hormone releasing hormone
GH = growth hormone (somatotrophin)
GHRIH = growth hormone release inhibiting hormone (somatostatin)
TRH = thyrotrophin releasing hormone
TSH = thyroid stimulating hormone
CRH = corticotrophin releasing hormone
ACTH = adrenocorticotrophic hormone
PRH = prolactin releasing hormone
PRL = prolactin (lactogenic hormone)
PIH = prolactin inhibiting hormone (dopamine)
LHRH = luteinising hormone releasing hormone
GnRH = gonadotrophin releasing hormone
FSH = follicle stimulating hormone
LH = luteinising hormone
Some of the hormones secreted by the anterior lobe stimulate or inhibit secretion by other endocrine glands (target glands) while others have a direct effect on target tissues. Table 9.1 summarises the main relationships between the hormones of the hypothalamus, the anterior pituitary and target glands or tissues.
Secretion of an anterior pituitary hormone follows stimulation of the gland by a specific releasing hormone produced by the hypothalamus and carried to the gland through the pituitary portal system (see above). The whole system is controlled by a negative feedback mechanism (Ch. 1). That is, when the level of a hormone in the blood supplying the hypothalamus is low it produces the appropriate releasing hormone that stimulates release of a trophic hormone by the anterior pituitary. This in turn stimulates the target gland to produce and release its hormone. As a result the blood level of that hormone rises and inhibits secretion of its releasing factor by the hypothalamus (Fig. 9.4).
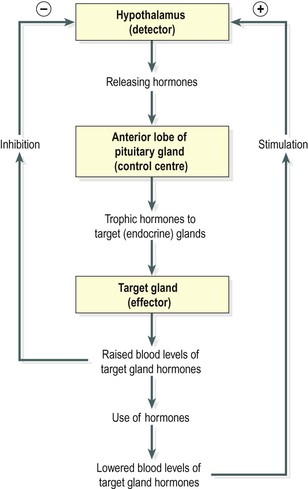
Figure 9.4 Negative feedback regulation of secretion of hormones by the anterior lobe of the pituitary gland.
Growth hormone (GH)
This is the most abundant hormone synthesised by the anterior pituitary. It stimulates growth and division of most body cells but especially those in the bones and skeletal muscles. Body growth in response to the secretion of GH is evident during childhood and adolescence, and thereafter secretion of GH maintains the mass of bones and skeletal muscles. It also regulates aspects of metabolism in many organs, e.g. liver, intestines and pancreas; stimulates protein synthesis, especially tissue growth and repair; promotes breakdown of fats and increases blood glucose levels (see Ch. 12).
Its release is stimulated by growth hormone releasing hormone (GHRH) and suppressed by growth hormone release inhibiting hormone (GHRIH), also known as somatostatin, both of which are secreted by the hypothalamus. Secretion of GH is greater at night during sleep and is also stimulated by hypoglycaemia (low blood sugar), exercise and anxiety. Secretion peaks in adolescence and then declines with age.
GH secretion is controlled by a negative feedback system; it is inhibited when the blood level rises and also when GHRIH is released by the hypothalamus. GHRIH also suppresses secretion of TSH and gastrointestinal secretions, e.g. gastric juice, gastrin and cholecystokinin (see Ch. 12).
Thyroid stimulating hormone (TSH)
The release of this hormone is stimulated by thyrotrophin releasing hormone (TRH) from the hypothalamus. It stimulates growth and activity of the thyroid gland, which secretes the hormones thyroxine (T4) and tri-iodothyronine (T3). Release is lowest in the early evening and highest during the night. Secretion is regulated by a negative feedback mechanism, i.e. when the blood level of thyroid hormones is high, secretion of TSH is reduced, and vice versa (Fig. 9.4).
Adrenocorticotrophic hormone (ACTH, corticotrophin)
Corticotrophin releasing hormone (CRH) from the hypothalamus promotes the synthesis and release of ACTH by the anterior pituitary. This increases the concentration of cholesterol and steroids within the adrenal cortex and the output of steroid hormones, especially cortisol.
ACTH levels are highest at about 8 a.m. and fall to their lowest about midnight, although high levels sometimes occur at midday and 6 p.m. This circadian rhythm is maintained throughout life. It is associated with the sleep pattern and adjustment to changes takes several days, e.g. following changing work shifts, travelling to a different time zone (jet lag).
Secretion is also regulated by a negative feedback mechanism, being suppressed when the blood level of ACTH rises (Fig. 9.4). Other factors that stimulate secretion include hypoglycaemia, exercise and other stressors, e.g. emotional states and fever.
Prolactin
This hormone is secreted during pregnancy to prepare the breasts for lactation (milk production) after childbirth. The blood level of prolactin is stimulated by prolactin releasing hormone (PRH) released from the hypothalamus and it is lowered by prolactin inhibiting hormone (PIH, dopamine) and by an increased blood level of prolactin. Immediately after birth, suckling stimulates prolactin secretion and lactation. The resultant high blood level is a factor in reducing the incidence of conception during lactation.
Gonadotrophins
Just before puberty two gonadotrophins (sex hormones) are secreted in gradually increasing amounts by the anterior pituitary in response to luteinising hormone releasing hormone (LHRH), also known as gonadotrophin releasing hormone (GnRH). Rising levels of these hormones at puberty promotes mature functioning of the reproductive organs. In both males and females the hormones responsible are:
In both sexes.
FSH stimulates production of gametes (ova or spermatozoa) by the gonads.
In females.
LH and FSH are involved in secretion of the hormones oestrogen and progesterone during the menstrual cycle (see Figs 18.9 and 18.10, pp. 456 and 457). As the levels of oestrogen and progesterone rise, secretion of LH and FSH is suppressed.
In males.
LH, also called interstitial cell stimulating hormone (ICSH) stimulates the interstitial cells of the testes to secrete the hormone testosterone (see Ch. 18).
Table 9.2 summarises the hormonal secretions of the anterior pituitary.
Table 9.2
Summary of the hormones secreted by the anterior pituitary gland and their functions
| Hormone | Function |
| Growth hormone (GH) | Regulates metabolism, promotes tissue growth especially of bones and muscles |
| Thyroid stimulating hormone (TSH) | Stimulates growth and activity of thyroid gland and secretion of T3 and T4 |
| Adrenocorticotrophic hormone (ACTH) | Stimulates the adrenal cortex to secrete glucocorticoids |
| Prolactin (PRL) | Stimulates growth of breast tissue and milk production |
| Follicle stimulating hormone (FSH) | Stimulates production of sperm in the testes, stimulates secretion of oestrogen by the ovaries, maturation of ovarian follicles, ovulation |
| Luteinising hormone (LH) | Stimulates secretion of testosterone by the testes, stimulates secretion of progesterone by the corpus luteum |
Posterior pituitary
The posterior pituitary is formed from nervous tissue and consists of nerve cells surrounded by supporting glial cells called pituicytes. These neurones have their cell bodies in the supraoptic and paraventricular nuclei of the hypothalamus and their axons form a bundle known as the hypothalamohypophyseal tract (Fig. 9.3A). Posterior pituitary hormones are synthesised in the nerve cell bodies, transported along the axons and stored in vesicles within the axon terminals in the posterior pituitary (Fig. 9.3B).
Nerve impulses from the hypothalamus trigger exocytosis of the vesicles, releasing their hormones into the bloodstream.
The structure of the posterior pituitary gland and its relationship with the hypothalamus is explained on page 217. Oxytocin and antidiuretic hormone (ADH, vasopressin) are the hormones released from axon terminals within the posterior pituitary (Fig. 9.3B). These hormones act directly on non-endocrine tissue.
Oxytocin
Oxytocin stimulates two target tissues during and after childbirth (parturition): uterine smooth muscle and the muscle cells of the lactating breast.
During childbirth increasing amounts of oxytocin are released from the posterior pituitary into the bloodstream in response to increasing stimulation of sensory stretch receptors in the uterine cervix as the baby’s head progressively dilates it. Sensory impulses are generated and travel to the control centre in the hypothalamus, stimulating the posterior pituitary to release more oxytocin. In turn this stimulates more forceful uterine contractions and greater stretching of the uterine cervix as the baby’s head is forced further downwards. This is an example of a positive feedback mechanism which stops soon after the baby is delivered when distension of the uterine cervix is greatly reduced (Fig. 9.5).
The process of milk ejection also involves a positive feedback mechanism. Suckling generates sensory impulses that are transmitted from the breast to the hypothalamus. The impulses trigger release of oxytocin from the posterior pituitary. On reaching the lactating breast, oxytocin stimulates contraction of the milk ducts and myoepithelial cells around the glandular cells, ejecting milk. Suckling also inhibits the release of prolactin inhibiting hormone (PIH), prolonging prolactin secretion and lactation.
Oxytocin levels rise during sexual arousal in both males and females. This increases smooth muscle contraction which is associated with glandular secretion and ejaculation in males. In females, contraction of smooth muscle in the vagina and uterus promotes movement of sperm towards the uterine tubes. It is believed that the smell of oxytocin may be involved in social recognition and bonding (between mother and newborn baby).
Antidiuretic hormone (ADH, vasopressin)
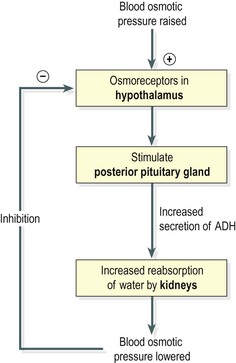
The main effect of antidiuretic hormone is to reduce urine output (diuresis is the production of a large volume of urine). ADH acts on the distal convoluted tubules and collecting ducts of the nephrons of the kidneys (Ch. 13). It increases their permeability to water and more of the glomerular filtrate is reabsorbed. ADH secretion is determined by the osmotic pressure of the blood circulating to the osmoreceptors in the hypothalamus.
As osmotic pressure rises, for example as a result of dehydration, secretion of ADH increases. More water is therefore reabsorbed and the urine output is reduced. This means that the body retains more water and the rise in osmotic pressure is reversed. Conversely, when the osmotic pressure of the blood is low, for example after a large fluid intake, secretion of ADH is reduced, less water is reabsorbed and more urine is produced (Fig. 9.6).
At high concentrations, for example after severe blood loss, ADH causes smooth muscle contraction, especially vasoconstriction in small arteries. This has a pressor effect, raising systemic blood pressure; the alternative name of this hormone, vasopressin, reflects this effect.
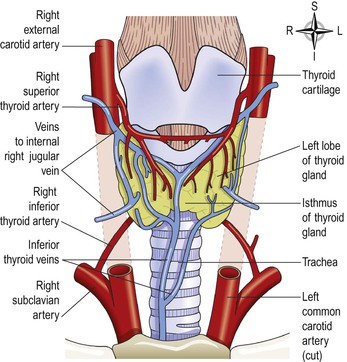
Thyroid gland (Fig. 9.7)
The thyroid gland is situated in the neck in front of the larynx and trachea at the level of the 5th, 6th and 7th cervical and 1st thoracic vertebrae. It is a highly vascular gland that weighs about 25 g and is surrounded by a fibrous capsule. It resembles a butterfly in shape, consisting of two lobes, one on either side of the thyroid cartilage and upper cartilaginous rings of the trachea. The lobes are joined by a narrow isthmus, lying in front of the trachea.
The lobes are roughly cone shaped, about 5 cm long and 3 cm wide.
The arterial blood supply to the gland is through the superior and inferior thyroid arteries. The superior thyroid artery is a branch of the external carotid artery and the inferior thyroid artery is a branch of the subclavian artery.
The venous return is by the thyroid veins, which drain into the internal jugular veins.
The recurrent laryngeal nerves pass upwards close to the lobes of the gland and, especially on the right side, lie near the inferior thyroid artery (see Fig. 9.10).
The gland is composed of largely spherical follicles formed from cuboidal epithelium (Fig. 9.9). These secrete and store colloid, a thick sticky protein material. Between the follicles are other cells found singly or in small groups: parafollicular cells, also called C-cells, which secrete the hormone calcitonin.
Thyroxine and tri-iodothyronine
Iodine is essential for the formation of the thyroid hormones, thyroxine (T4) and tri-iodothyronine (T3), so numbered as these molecules contain four and three atoms of the element iodine respectively. The main dietary sources of iodine are seafood, vegetables grown in iodine-rich soil and iodinated table salt. The thyroid gland selectively takes up iodine from the blood, a process called iodine trapping.
Thyroid hormones are synthesised as large precursor molecules called thyroglobulin, the major constituent of colloid. The release of T3 and T4 into the blood is stimulated by thyroid stimulating hormone (TSH) from the anterior pituitary.
Secretion of TSH is stimulated by thyrotrophin releasing hormone (TRH) from the hypothalamus and secretion of TRH is stimulated by exercise, stress, malnutrition, low plasma glucose levels and sleep. TSH secretion depends on the plasma levels of T3 and T4 because it is these hormones that control the sensitivity of the anterior pituitary to TRH. Through the negative feedback mechanism, increased levels of T3 and T4 decrease TSH secretion and vice versa (Fig. 9.8). Dietary iodine deficiency greatly increases TSH secretion causing proliferation of thyroid gland cells and enlargement of the gland (goitre, see Fig. 9.16). Secretion of T3 and T4 begins about the third month of fetal life and increases at puberty and in women during the reproductive years, especially during pregnancy. Otherwise, it remains fairly constant throughout life. Of the two thyroid hormones, T4 is much more abundant. However it is less potent than T3, which is more physiologically important. Most T4 is converted into T3 inside target cells. ![]() 9.2
9.2
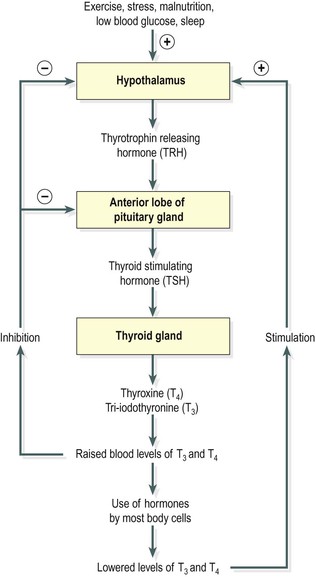
Figure 9.8 Negative feedback regulation of the secretion of thyroxine (T4) and tri-iodothyronine (T3).
Thyroid hormones enter the cell nucleus and regulate gene expression, i.e. they increase or decrease protein synthesis (see Ch. 17). They enhance the effects of other hormones, e.g. adrenaline (epinephrine) and noradrenaline (norepinephrine). T3 and T4 affect most cells of the body by:
• increasing the basal metabolic rate and heat production
• regulating metabolism of carbohydrates, proteins and fats.
T3 and T4 are essential for normal growth and development, especially of the skeleton and nervous system. Most other organs and systems are also influenced by thyroid hormones. Physiological effects of T3 and T4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree