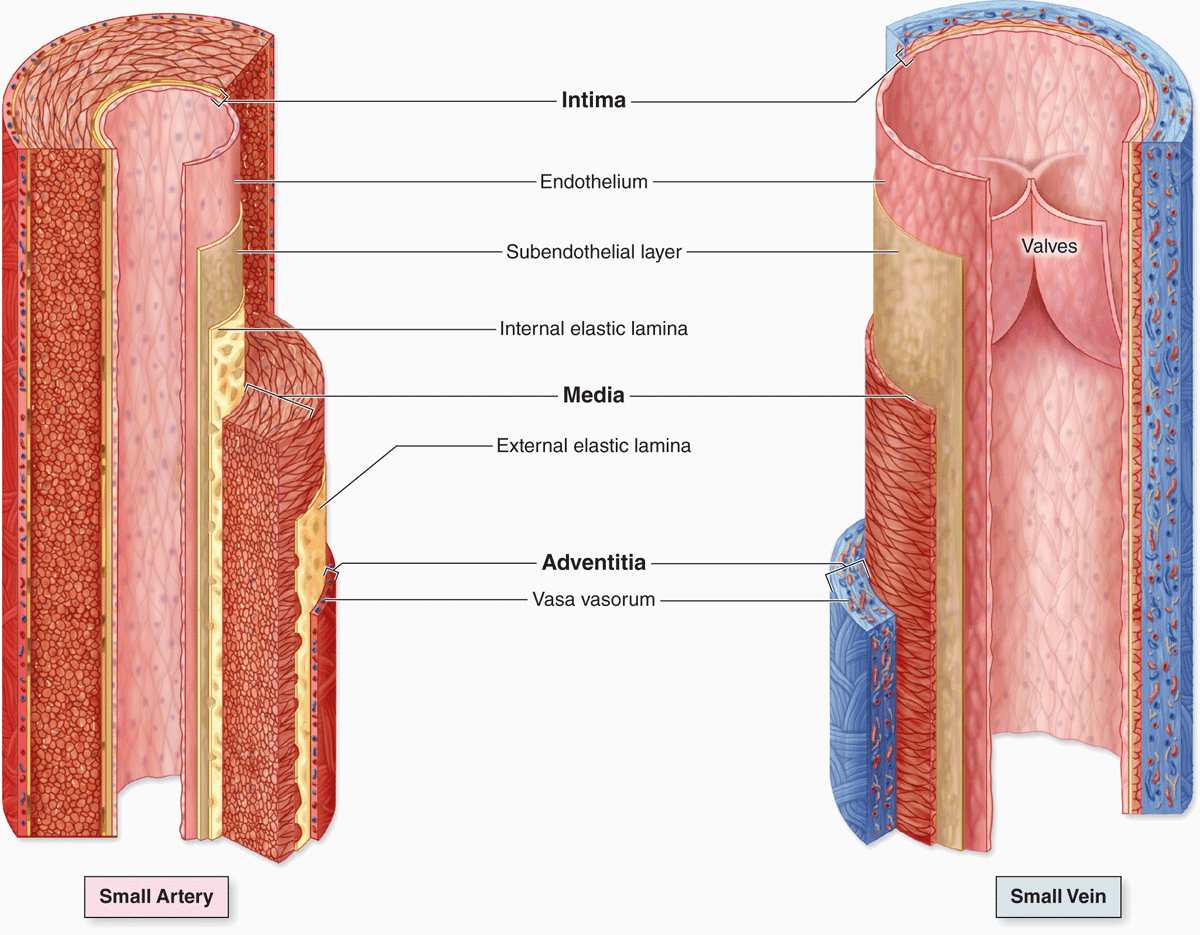
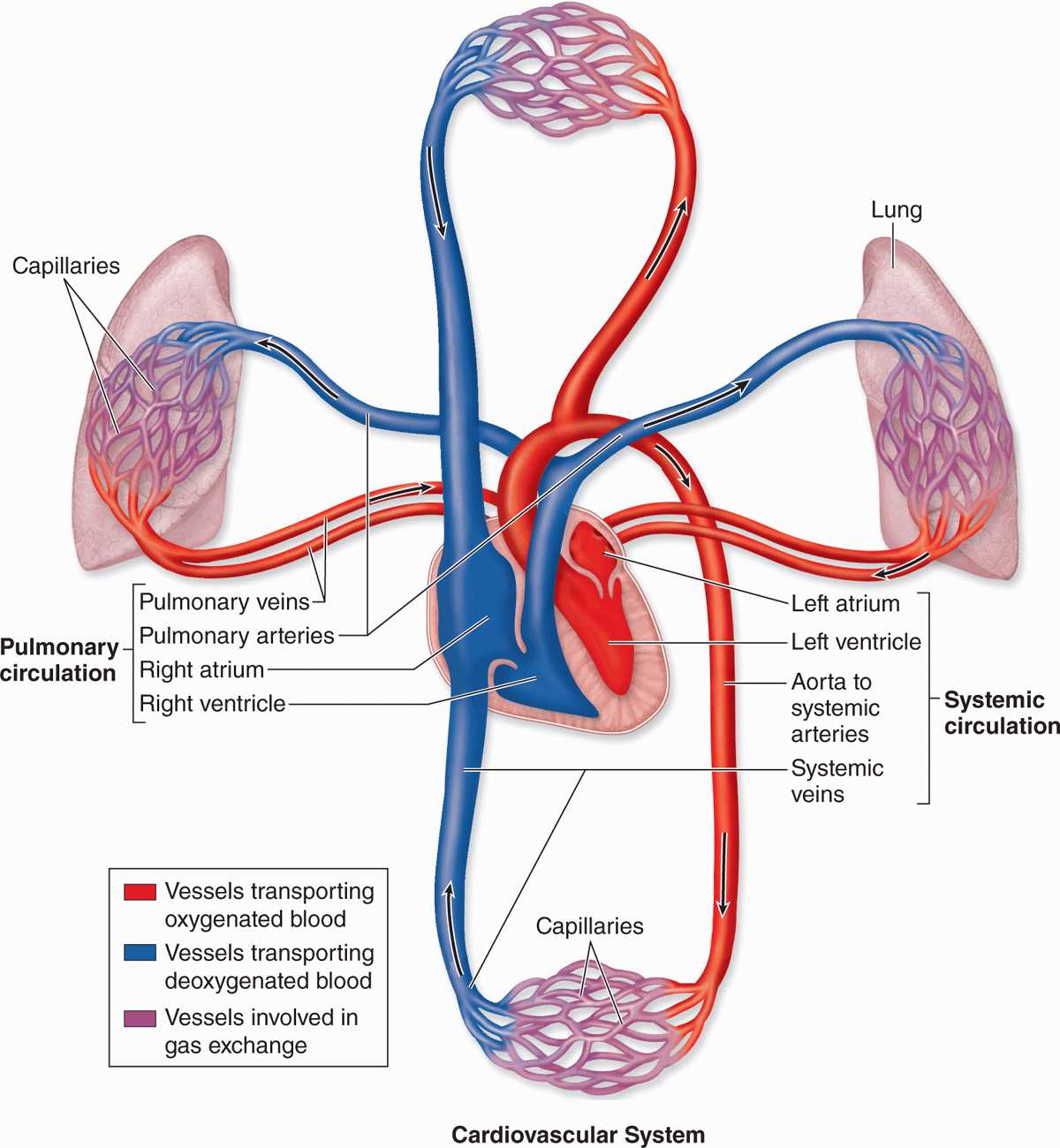
The circulatory system pumps and directs blood cells and substances carried in blood to all tissues of the body. It includes both the blood and lymphatic vascular systems, and in an adult the total length of its vessels is estimated at between 100,000 and 150,000 kilometers. The blood vascular system, or cardiovascular system (Figure 11–1), consists of the following structures:
FIGURE 11–1 Diagram of the cardiovascular system.
 The heart propels blood through the system.
The heart propels blood through the system.
 Arteries, a series of vessels efferent from the heart that become smaller as they branch into the various organs, carry blood to the tissues.
Arteries, a series of vessels efferent from the heart that become smaller as they branch into the various organs, carry blood to the tissues.
 Capillaries, the smallest vessels, are the sites of O2, CO2, nutrient, and waste product exchange between blood and tissues. Together with the smallest arterial and venous branches carrying blood to and from them, capillaries in almost every organ form a complex network of thin, anastomosing tubules called the microvasculature or microvascular bed.
Capillaries, the smallest vessels, are the sites of O2, CO2, nutrient, and waste product exchange between blood and tissues. Together with the smallest arterial and venous branches carrying blood to and from them, capillaries in almost every organ form a complex network of thin, anastomosing tubules called the microvasculature or microvascular bed.
 Veins result from the convergence of venules into a system of larger channels that continue enlarging as they approach the heart, toward which they carry the blood to be pumped again.
Veins result from the convergence of venules into a system of larger channels that continue enlarging as they approach the heart, toward which they carry the blood to be pumped again.
As shown in Figure 11–1, two major divisions of arteries, microvasculature, and veins make up the pulmonary circulation, where blood is oxygenated in the lungs, and the systemic circulation, where blood brings nutrients and removes wastes in tissues throughout the body.
The lymphatic vascular system, introduced with the discussion of interstitial fluid in Chapter 5, begins with the lymphatic capillaries, which are thin-walled, closed-ended tubules carrying lymph, that merge to form vessels of steadily increasing size. The largest lymph vessels connect with the blood vascular system and empty into the large veins near the heart. This returns fluid from tissue spaces all over the body to the blood.
The internal surface of all components of the blood and lymphatic systems is lined by a single layer of a squamous epithelium, called endothelium. As the interface between blood and the organs, cardiovascular endothelial cells have crucial physiologic and medical importance. Not only must endothelial cells maintain a selectively permeable, antithrombogenic (inhibitory to clot formation) barrier, they also determine when and where white blood cells leave the circulation for the interstitial space of tissues and secrete a variety of paracrine factors for vessel dilation, constriction, and growth of adjacent cells.
HEART
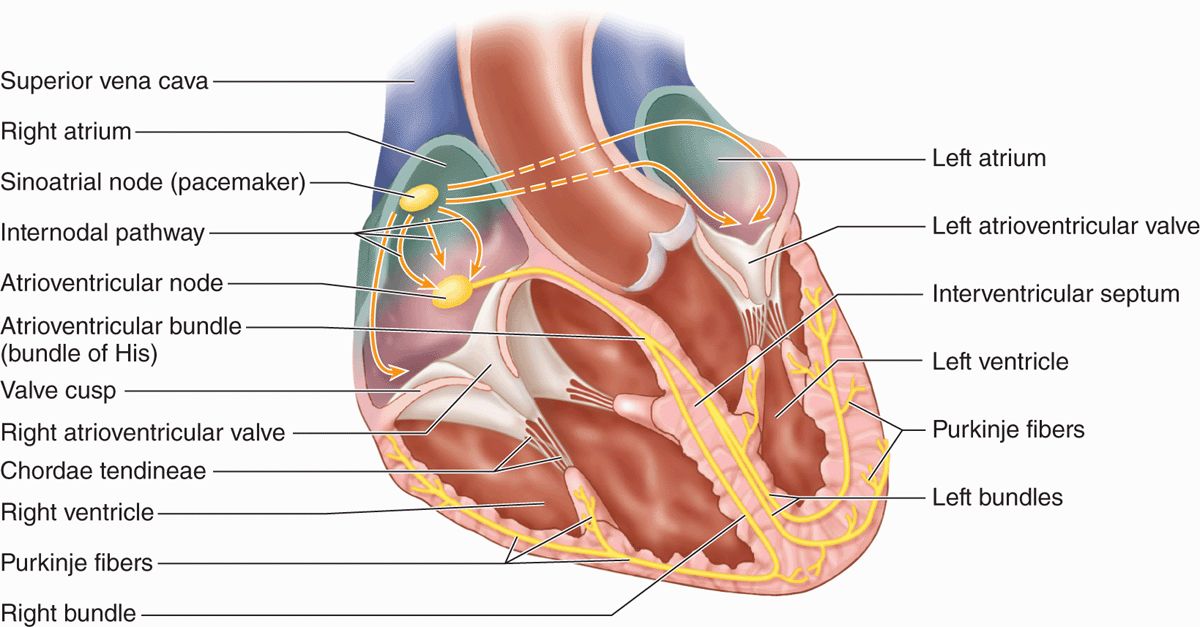
Cardiac muscle in the four chambers of the heart wall contracts rhythmically, pumping the blood through the circulatory system (Figure 11–2). The right and left ventricles propel blood to the pulmonary and systemic circulation, respectively; right and left atria receive blood from the body and the pulmonary veins, respectively. The walls of all four heart chambers consist of three major layers: the internal endocardium; the middle myocardium; and the external epicardium.
FIGURE 11–2 Important features of the heart.
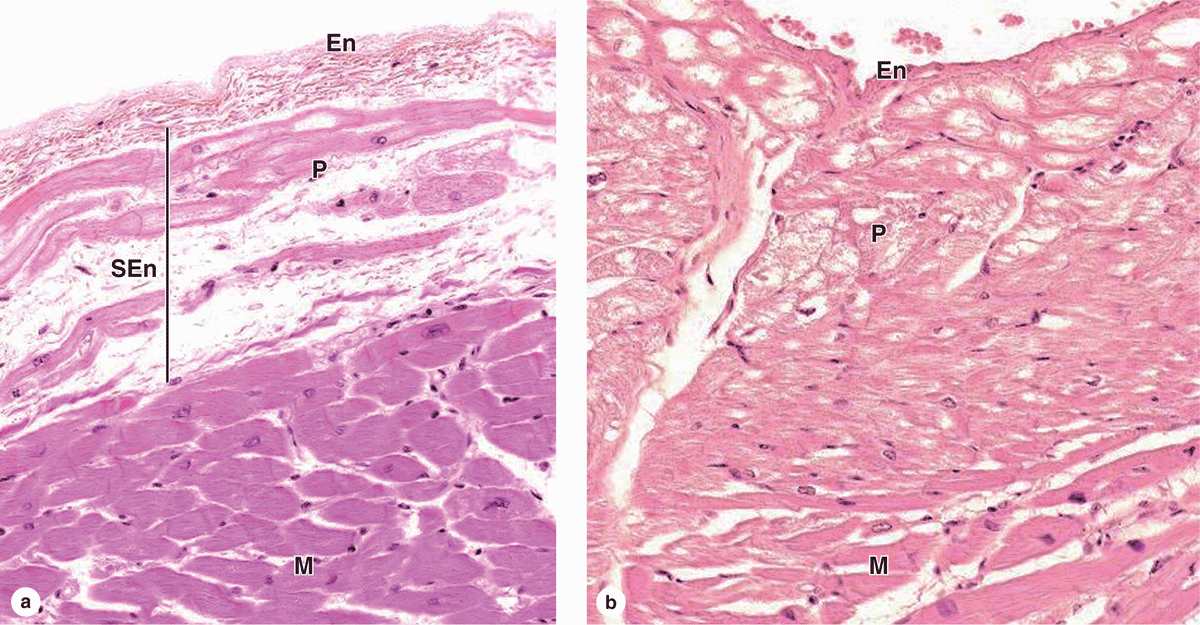
 The endocardium consists of a very thin inner layer of endothelium and supporting connective tissue, a middle myoelastic layer of smooth muscle fibers and connective tissue, and a deep layer of connective tissue called the subendocardial layer that merges with the myocardium Branches of the heart’s impulse-conducting system, consisting of modified cardiac muscle fibers, are also located in the subendocardial layer (Figure 11–3).
The endocardium consists of a very thin inner layer of endothelium and supporting connective tissue, a middle myoelastic layer of smooth muscle fibers and connective tissue, and a deep layer of connective tissue called the subendocardial layer that merges with the myocardium Branches of the heart’s impulse-conducting system, consisting of modified cardiac muscle fibers, are also located in the subendocardial layer (Figure 11–3).
FIGURE 11–3 Endocardium, myocardium, and fibers of the subendocardial conducting network.
 The thickest layer, the myocardium, consists mainly of cardiac muscle with its fibers arranged spirally around each heart chamber. Because strong force is required to pump blood through the systemic and pulmonary circulations, the myocardium is much thicker in the walls of the ventricles, particularly the left, than in the atrial walls (Figure 11–3).
The thickest layer, the myocardium, consists mainly of cardiac muscle with its fibers arranged spirally around each heart chamber. Because strong force is required to pump blood through the systemic and pulmonary circulations, the myocardium is much thicker in the walls of the ventricles, particularly the left, than in the atrial walls (Figure 11–3).
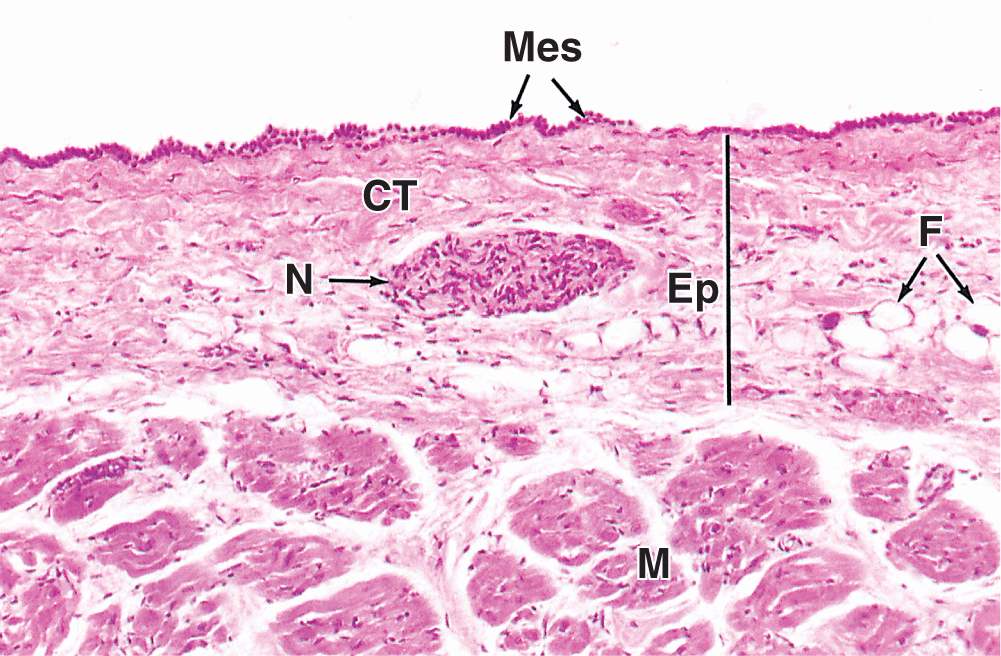
 The epicardium is a simple squamous mesothelium supported by a layer of loose connective tissue containing blood vessels and nerves (Figure 11–4). The epicardium corresponds to the visceral layer of the pericardium, the membrane surrounding the heart. Where the large vessels enter and leave the heart, the epicardium is reflected back as the parietal layer lining the pericardium. During heart movements, underlying structures are cushioned by deposits of adipose tissue in the epicardium and friction within the pericardium is prevented by lubricant fluid produced by both layers of serous mesothelial cells.
The epicardium is a simple squamous mesothelium supported by a layer of loose connective tissue containing blood vessels and nerves (Figure 11–4). The epicardium corresponds to the visceral layer of the pericardium, the membrane surrounding the heart. Where the large vessels enter and leave the heart, the epicardium is reflected back as the parietal layer lining the pericardium. During heart movements, underlying structures are cushioned by deposits of adipose tissue in the epicardium and friction within the pericardium is prevented by lubricant fluid produced by both layers of serous mesothelial cells.
FIGURE 11–4 Epicardium or visceral pericardium.
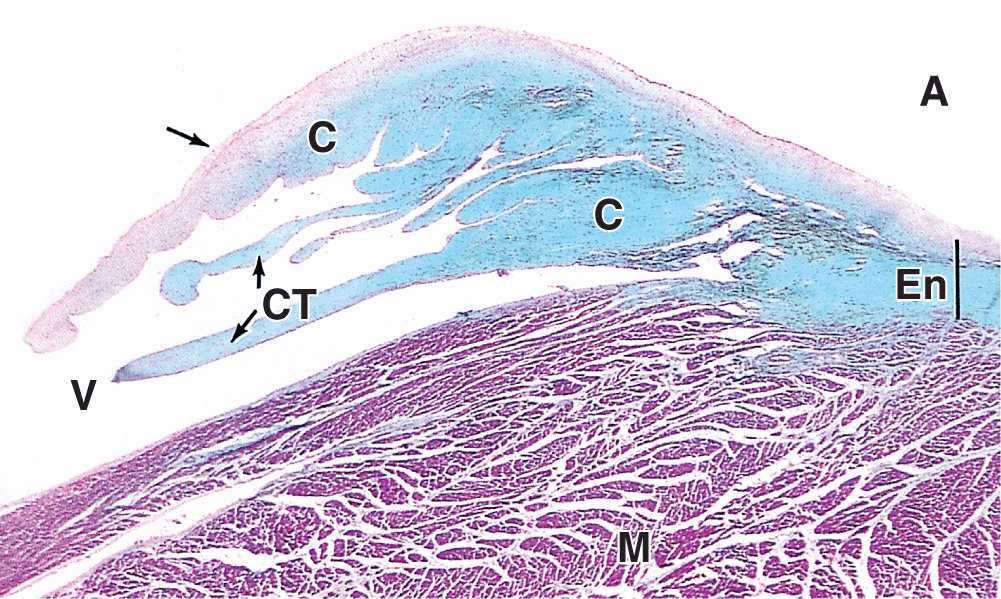
Within these major layers the heart contains other structures important for its overall function of moving blood. Dense fibrous connective tissue of the cardiac skeleton forms part of the interventricular and interatrial septa, surrounds all valves of the heart, and extends into the valve cusps and the chordae tendineae to which they are attached (Figures 11–2 and 11–5). These regions of dense irregular connective tissue perform the following functions:
FIGURE 11–5 Valve leaflet and cardiac skeleton.
 Anchoring and supporting the heart valves
Anchoring and supporting the heart valves
 Providing firm points of insertion for cardiac muscle
Providing firm points of insertion for cardiac muscle
 Helping coordinate the heartbeat by acting as electrical insulation between atria and ventricles
Helping coordinate the heartbeat by acting as electrical insulation between atria and ventricles
Within the subendocardial layer and adjacent myocardium, modified cardiac muscle cells make up the impulse conducting system of the heart, which generates and propagates waves of depolarization that spread through the myocardium to stimulate rhythmic contractions. This system (Figure 11–2) consists of two nodes of specialized myocardial tissue in the right atrium: the sinoatrial (SA) node (or pacemaker) and the atrioventricular (AV) node, followed by the AV bundle (of His) and the subendocardial conducting network.
Located in the right atrial wall near the superior vena cava, the SA node is a 6- to 7-mm3 mass of cardiac muscle cells with smaller size, fewer myofibrils, and fewer typical intercalated disks than the neighboring muscle fibers. Impulses initiated by these cells move along the myocardial fibers of both atria, stimulating their contraction. When the impulses reach the slightly smaller AV node, located in the floor of the right atrium near the AV valve and composed of cells similar to those of the SA node, they stimulate depolarization of those cells. Conducting muscle fibers from the AV node form the AV bundle, pass through an opening in the cardiac skeleton into the interventricular septum, and bifurcate into the wall of each ventricle.
At the apex of the heart, the bundles branch further into a subendocardial conducting network of myofibers, usually called Purkinje fibers. These are pale-staining fibers, larger than the adjacent contractile muscle fibers, with sparse, peripheral myofibrils and much glycogen (Figure 11–3). Purkinje fibers mingle distally with contractile fibers of both ventricles and trigger waves of contraction through both ventricles simultaneously.
Both parasympathetic and sympathetic neural components innervate the heart. Ganglionic nerve cells and nerve fibers are present in the regions close to the SA and AV nodes, where they affect heart rate and rhythm, such as during physical exercise and emotional stress. Stimulation of the parasympathetic division (vagus nerve) slows the heartbeat, whereas stimulation of the sympathetic nerve accelerates activity of the pacemaker. Between fibers of the myocardium are afferent free nerve endings that register pain, such as the discomfort called angina pectoris that occurs when partially occluded coronary arteries cause local oxygen deprivation.
TISSUES OF THE VASCULAR WALL
Walls of all blood vessels except capillaries contain smooth muscle and connective tissue in addition to the endothelial lining. The amount and arrangement of these tissues in vessels are influenced by mechanical factors, primarily blood pressure, and metabolic factors reflecting the local needs of tissues.
The endothelium is a specialized epithelium that acts as a semipermeable barrier between two internal compartments: the blood plasma and the interstitial tissue fluid. Vascular endothelial cells are squamous, polygonal, and elongated with the long axis in the direction of blood flow. Endothelium with its basal lamina is highly differentiated to mediate and actively monitor the bidirectional exchange of molecules by simple and active diffusion, receptor-mediated endocytosis, transcytosis, and other mechanisms discussed in Chapter 4.
Besides their key role in metabolite exchanges between blood and tissues, endothelial cells have several other functions:
 The endothelium presents a nonthrombogenic surface on which blood will not clot and actively secretes agents that control local clot formation (such as heparin, tissue plasminogen activator, and von Willebrand factor).
The endothelium presents a nonthrombogenic surface on which blood will not clot and actively secretes agents that control local clot formation (such as heparin, tissue plasminogen activator, and von Willebrand factor).
 The cells regulate local vascular tone and blood flow by secreting various factors that stimulate smooth muscle contraction (such as endothelin 1 and angiotensin-converting enzyme [ACE]) or relaxation (including nitric oxide [NO] and prostacyclin).
The cells regulate local vascular tone and blood flow by secreting various factors that stimulate smooth muscle contraction (such as endothelin 1 and angiotensin-converting enzyme [ACE]) or relaxation (including nitric oxide [NO] and prostacyclin).
 Endothelium has several roles in inflammation and local immune responses. In venules endothelial cells induce specific white blood cells to stop and undergo transendothelial migration at sites of injury or infection. Under those conditions P-selectin is expressed rapidly on the luminal surface when unique elongated granules, called Weibel-Palade bodies, fuse with the cell membrane. As described further in Chapter 12, adhesion to selectins is the first step in the activation of white blood cells specifically where they are needed. Endothelial cells also secrete various factors called interleukins that affect the activity of local white blood cells during inflammation.
Endothelium has several roles in inflammation and local immune responses. In venules endothelial cells induce specific white blood cells to stop and undergo transendothelial migration at sites of injury or infection. Under those conditions P-selectin is expressed rapidly on the luminal surface when unique elongated granules, called Weibel-Palade bodies, fuse with the cell membrane. As described further in Chapter 12, adhesion to selectins is the first step in the activation of white blood cells specifically where they are needed. Endothelial cells also secrete various factors called interleukins that affect the activity of local white blood cells during inflammation.
 Under various conditions endothelial cells secrete various growth factors, including proteins promoting proliferation of specific white blood cell lineages and cells that make up the vascular wall.
Under various conditions endothelial cells secrete various growth factors, including proteins promoting proliferation of specific white blood cell lineages and cells that make up the vascular wall.
Growth factors such as vascular endothelial growth factor (VEGF) stimulate formation of the vascular system from embryonic mesenchyme (vasculogenesis), help maintain the vasculature in adults, and promote capillary sprouting and outgrowth from small existing vessels (angiogenesis) during normal growth, during tissue repair and regeneration, and in tumors and other pathological conditions. In both processes other growth factors, called angiopoietins, stimulate endothelial cells to recruit smooth muscle cells and fibroblasts to form the other tissues of the vascular wall.
Smooth muscle fibers occur in the walls of all vessels larger than capillaries and are arranged helically in layers. In arterioles and small arteries, the smooth muscle cells are connected by many more gap junctions and permit vasoconstriction and vasodilation which are of key importance in regulating the overall blood pressure.
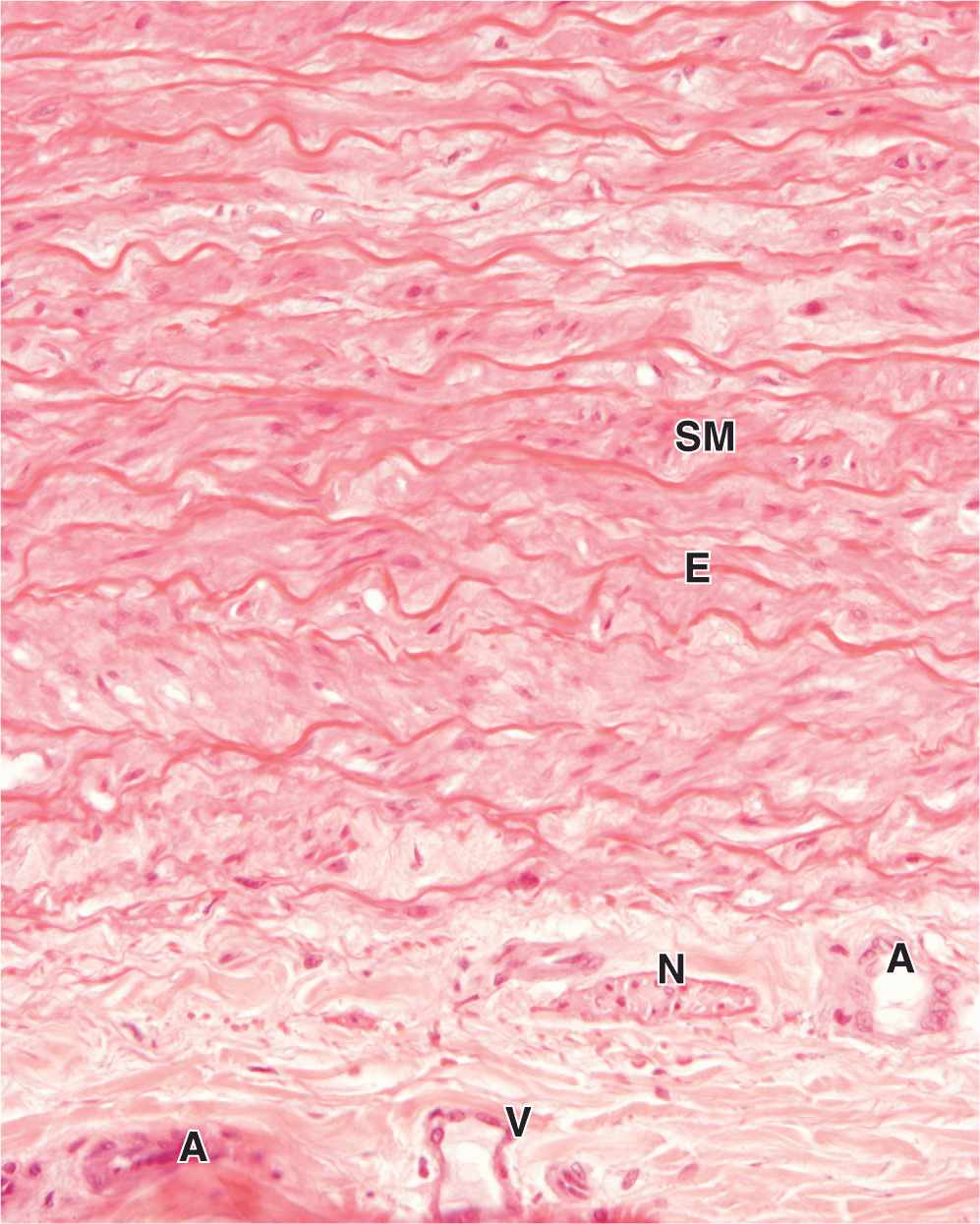
Connective tissue components are present in vascular walls in variable amounts and proportions based on local functional requirements. Collagen fibers are found in the subendothelial layer, between the smooth muscle layers, and in the outer covering. Elastic fibers provide the resiliency required for the vascular wall to expand under pressure. Elastin is a major component in large arteries where it forms parallel lamellae, regularly distributed between the muscle layers. Variations in the amount and composition of ground substance components such as proteoglycans and hyaluronate also contribute to the physical and metabolic properties of the wall in different vessels, especially affecting their permeability.
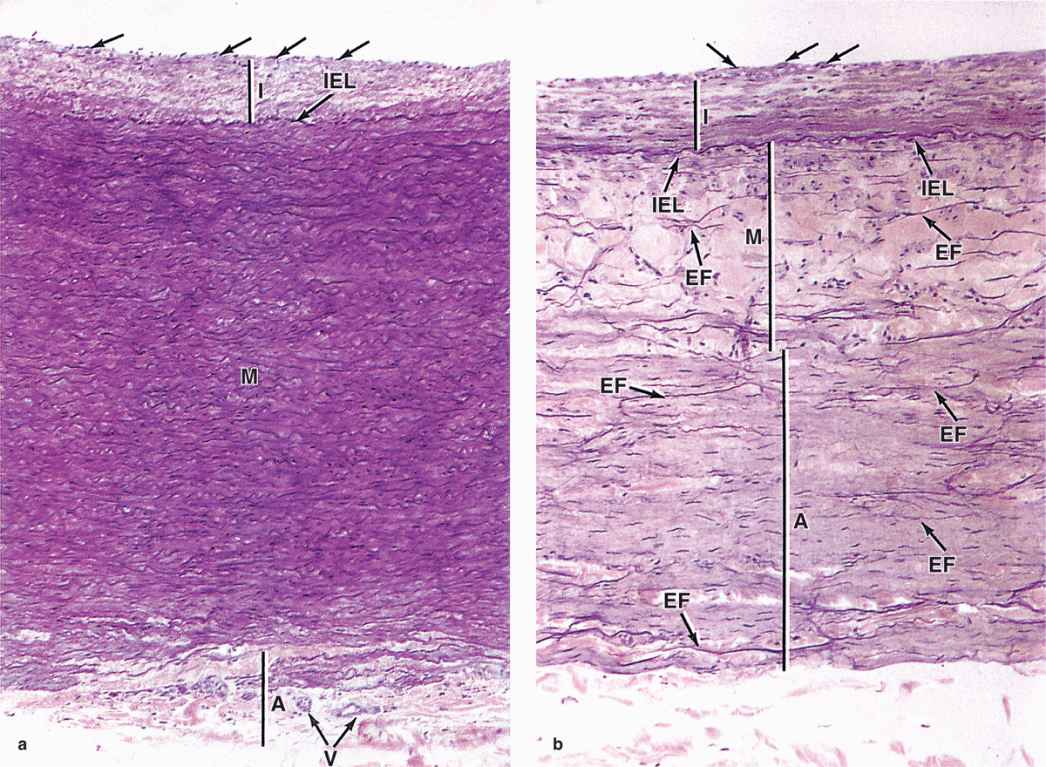
The walls of all blood vessels larger than the microvasculature have many components in common and similar organization. Branching of the vessels helps produce reductions in their size which are accompanied by gradual changes in the composition of the vascular wall. Transitions such as those from “small arteries” to “arterioles” are not clear-cut. However, all of these larger vessels have walls with three concentric layers, or tunics (L. tunica, coat), as shown in the diagram of Figure 11–6 and in the micrographs of Figures 11–7 through 11–9.
FIGURE 11–6 Walls of arteries and veins.
FIGURE 11–7 Tunics of the vascular wall.
FIGURE 11–8 Vasa vasorum.
 MEDICAL APPLICATION
MEDICAL APPLICATION