1 is generally recommended.
Examination
When it is done properly, the examination takes some time to perform (about 3 minutes per breast).
The examination is only just over 50% sensitive for carcinoma but specificity is as high as 90%. The likelihood ratio of a positive examination is 14.1 and the LR of a negative examination is 0.47.
Inspection
Ask the patient to sit up with her chest fully exposed. There is controversy about the value of inspection of the breasts as part of the examination, but advanced cancers may be obvious at this stage. Look at the nipples for retraction (due to cancer or fibrosis; in some patients retraction may be normal) and Paget’s disease of the breast (where underlying breast cancer causes a unilateral red, bleeding skin).
Next inspect the rest of the skin. Look for visible veins (which if unilateral suggest a cancer), skin dimpling, and for peau d’orange skin (where advanced breast cancer causes oedematous skin pitted by the sweat glands).
A persistent erythematous plaque in the areola area may be contact dermatitis or skin irrigation, but if asymmetric or it has not responded to treatment this may be the malignancy Paget disease of the breast.
Ask the patient to raise her arms above her head and then lower them slowly. Look for tethering of the nipples or skin, a shift in the relative position of the nipples or a fixed mass distorting the breast (

Figure 14.1 Carcinoma of the right breast, showing elevation of the breast, dimpling of skin, and retraction of the nipple
Note whether there are any obvious visible masses in the axillae.
Next ask her to rest her hands on her hips and then press her hands against her hips (the pectoral contraction manoeuvre). This accentuates areas of dimpling or fixation.
Palpation
Examine both the supraclavicular and axillary regions for lymphadenopathy. It may be difficult, however, to distinguish an axillary fat pad from an enlarged lymph node.
Then ask the patient to lie down. The examination can be performed only if the breast tissue is flattened against the chest wall. If the breasts are large, it can be helpful to have the patient place her hand on her forehead for the palpation of the lateral aspect of the breast and bring her elbow up level with the shoulder for the palpation of the medial side of the breast.
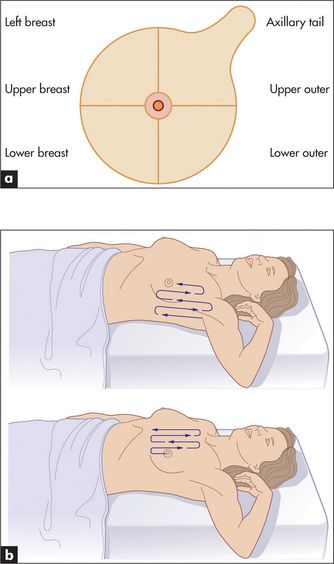
Palpation is performed gently with the pulps of the middle three fingers parallel to the contour of the breast. Feel the four quadrants of each breast systematically (
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree