Chapter 4
The blood
Blood is a fluid connective tissue. It circulates constantly around the body, allowing constant communication between tissues distant from each other. It transports:
Blood is composed of a clear, straw-coloured, watery fluid called plasma in which several different types of blood cell are suspended. Plasma normally constitutes 55% of the volume of blood and the cell fraction 45%. Blood cells and plasma can be separated by centrifugation (spinning) or by gravity when blood is allowed to stand (Fig. 4.1A). The cells are heavier than plasma and sink to the bottom of any sample.
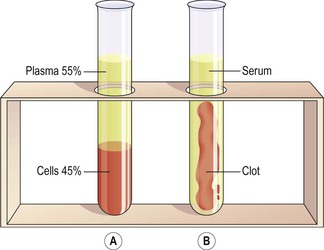
Figure 4.1 A. The proportions of blood cells and plasma in whole blood separated by gravity. B. A blood clot in serum.
Blood makes up about 7% of body weight (about 5.6 litres in a 70 kg man). This proportion is less in women and considerably greater in children, gradually decreasing until the adult level is reached.
Blood in the blood vessels is always in motion because of the pumping action of the heart. The continual flow maintains a fairly constant environment for body cells. Blood volume and the concentration of its many constituents are kept within narrow limits by homeostatic mechanisms. Heat produced from metabolically active organs, such as working skeletal muscles and the liver, is distributed around the body by the bloodstream, contributing to maintenance of core body temperature.
The first part of the chapter describes normal blood physiology, and the later sections are concerned with some disorders of the blood. Effects of ageing on white blood cell function are described in Chapter 15.
Plasma
The constituents of plasma are water (90–92%) and dissolved and suspended substances, including:
Plasma proteins
Plasma proteins, which make up about 7% of plasma, are normally retained within the blood, because they are too big to escape through the capillary pores into the tissues. They are largely responsible for creating the osmotic pressure of blood (p. 86), which keeps plasma fluid within the circulation. If plasma protein levels fall, because of either reduced production or loss from the blood vessels, osmotic pressure is also reduced, and fluid moves into the tissues (oedema) and body cavities.
Plasma viscosity (thickness) is due to plasma proteins, mainly albumin and fibrinogen. Plasma proteins, with the exception of immunoglobulins, are formed in the liver.
Albumins.
These are the most abundant plasma proteins (about 60% of total) and their main function is to maintain normal plasma osmotic pressure. Albumins also act as carrier molecules for free fatty acids, some drugs and steroid hormones.
Globulins.
Their main functions are:
• as antibodies (immunoglobulins), which are complex proteins produced by lymphocytes that play an important part in immunity. They bind to, and neutralise, foreign materials (antigens) such as micro-organisms (see also p. 381).
• inhibition of some proteolytic enzymes, e.g. α2 macroglobulin inhibits trypsin activity.
Electrolytes
These have a range of functions, including muscle contraction (e.g. Ca2+), transmission of nerve impulses (e.g. Ca2+ and Na+), and maintenance of acid–base balance (e.g. phosphate,  ). The pH of blood is maintained between 7.35 and 7.45 (slightly alkaline) by an ongoing buffering system (p. 25).
). The pH of blood is maintained between 7.35 and 7.45 (slightly alkaline) by an ongoing buffering system (p. 25).
Nutrients
The products of digestion, e.g. glucose, amino acids, fatty acids and glycerol, are absorbed from the alimentary tract. Together with mineral salts and vitamins they are used by body cells for energy, heat, repair and replacement, and for the synthesis of other blood components and body secretions.
Waste products
Urea, creatinine and uric acid are the waste products of protein metabolism. They are formed in the liver and carried in blood to the kidneys for excretion. Carbon dioxide from tissue metabolism is transported to the lungs for excretion.
Hormones (see Ch. 9)
These are chemical messengers synthesised by endocrine glands. Hormones pass directly from the endocrine cells into the blood, which transports them to their target tissues and organs elsewhere in the body, where they influence cellular activity.
Gases
Oxygen, carbon dioxide and nitrogen are transported round the body dissolved in plasma. Oxygen and carbon dioxide are also transported in combination with haemoglobin in red blood cells (p. 65). Most oxygen is carried in combination with haemoglobin and most carbon dioxide as bicarbonate ions dissolved in plasma (p. 260). Atmospheric nitrogen enters the body in the same way as other gases and is present in plasma but it has no physiological function.
Cellular content of blood  4.1
4.1
There are three types of blood cell (Fig. 4.2).
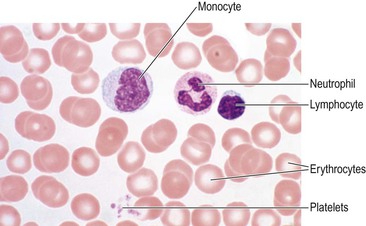
Figure 4.2 A blood smear, showing erythrocytes, a monocyte, a neutrophil, a lymphocyte and a platelet.
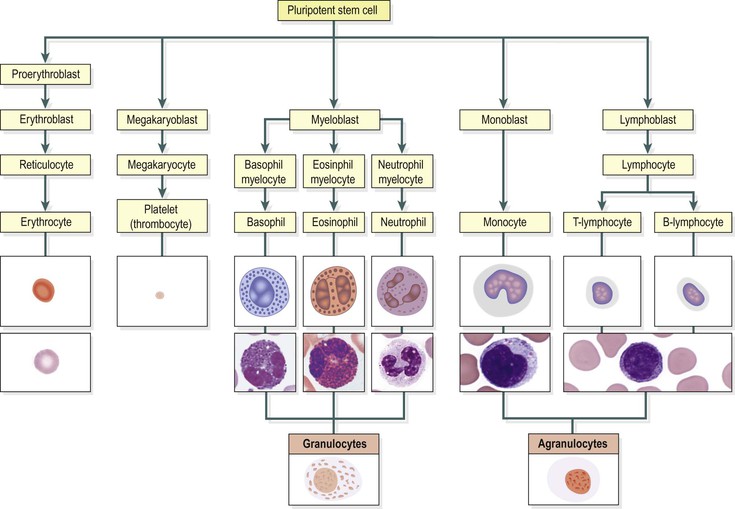
Blood cells are synthesised mainly in red bone marrow. Some lymphocytes, additionally, are produced in lymphoid tissue. In the bone marrow, all blood cells originate from pluripotent (i.e. capable of developing into one of a number of cell types) stem cells and go through several developmental stages before entering the blood. Different types of blood cell follow separate lines of development. The process of blood cell formation is called haemopoiesis (Fig. 4.3).
For the first few years of life, red marrow occupies the entire bone capacity and, over the next 20 years, is gradually replaced by fatty yellow marrow that has no haemopoietic function. In adults, haemopoiesis in the skeleton is confined to flat bones, irregular bones and the ends (epiphyses) of long bones, the main sites being the sternum, ribs, pelvis and skull.
Erythrocytes (red blood cells)  4.2
4.2
Red blood cells are by far the most abundant type of blood cell; 99% of all blood cells are erythrocytes (Fig. 4.2). They are biconcave discs with no nucleus, and their diameter is about 7 µm (Fig. 4.4). Their main function is in gas transport, mainly of oxygen, but they also carry some carbon dioxide. Their characteristic shape is suited to their purpose; the biconcavity increases their surface area for gas exchange, and the thinness of the central portion allows fast entry and exit of gases. The cells are flexible so they can squeeze through narrow capillaries, and contain no intracellular organelles, leaving more room for haemoglobin, the large pigmented protein responsible for gas transport.
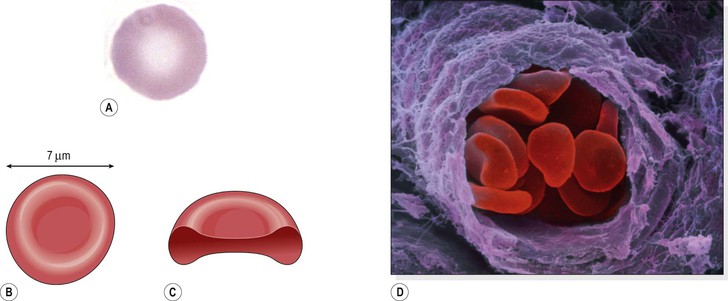
Figure 4.4 The red blood cell. A. Under the light microscope. B. Drawn from the front. C. Drawn in section. D. Coloured scanning electron micrograph of a group of red blood cells travelling along an arteriole.
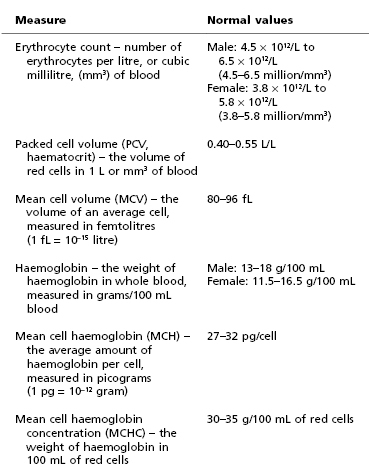
Measurements of red cell numbers, volume and haemoglobin content are routine and useful assessments made in clinical practice (Table 4.1). The symbols in brackets are the abbreviations commonly used in laboratory reports.
Life span and function of erythrocytes
Because they have no nucleus, erythrocytes cannot divide and so need to be continually replaced by new cells from the red bone marrow, which is present in the ends of long bones and in flat and irregular bones. They pass through several stages of development before entering the blood. Their life span in the circulation is about 120 days. There are approximately 30 trillion (1014) red blood cells in the average human body, about 25% of the body’s total cell count, and around 1%, mainly older cells, are cleared and destroyed daily.
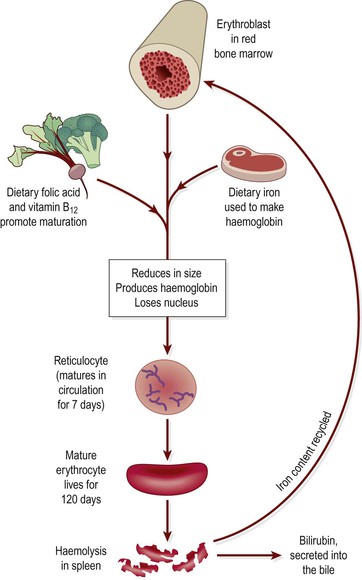
The process of development of red blood cells from stem cells takes about 7 days and is called erythropoiesis (Fig. 4.3). The immature cells are released into the bloodstream as reticulocytes, and mature into erythrocytes over a day or two within the circulation. During this time, they lose their nucleus and therefore become incapable of division (Fig. 4.5).
Both vitamin B12 and folic acid are required for red blood cell synthesis. They are absorbed in the intestines, although vitamin B12 must be bound to intrinsic factor (p. 300) to allow absorption to take place. Both vitamins are present in dairy products, meat and green vegetables. The liver usually contains substantial stores of vitamin B12, several years’ worth, but signs of folic acid deficiency appear within a few months. The life cycle of the erythrocyte is shown in Figure 4.5.
Haemoglobin
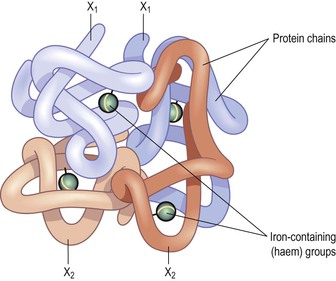
Haemoglobin is a large, complex molecule containing a globular protein (globin) and a pigmented iron-containing complex called haem. Each haemoglobin molecule contains four globin chains and four haem units, each with one atom of iron (Fig. 4.6). As each atom of iron can combine with an oxygen molecule, this means that a single haemoglobin molecule can carry up to four molecules of oxygen. An average red blood cell carries about 280 million haemoglobin molecules, giving each cell a theoretical oxygen-carrying capacity of over a billion oxygen molecules!
Iron is carried in the bloodstream bound to its transport protein, transferrin, and stored in the liver. Normal red cell production requires a steady supply of iron. Absorption of iron from the alimentary canal is very slow, even if the diet is rich in iron, meaning that iron deficiency can readily occur if losses exceed intake.
Oxygen transport
When all four oxygen-binding sites on a haemoglobin molecule are full, it is described as saturated. Haemoglobin binds reversibly to oxygen to form oxyhaemoglobin, according to the equation:
As the oxygen content of blood increases, its colour changes too. Blood rich in oxygen (usually arterial blood) is bright red because of the high levels of oxyhaemoglobin it contains, compared with blood with lower oxygen levels (usually venous blood), which is dark bluish in colour because it is not saturated.
The association of oxygen with haemoglobin is a loose one, so that oxyhaemoglobin releases its oxygen readily, especially under certain conditions.
Low pH
Metabolically active tissues, e.g. exercising muscle, release acid waste products, and so the local pH falls. Under these conditions, oxyhaemoglobin readily breaks down, giving up additional oxygen for tissue use.
Low oxygen levels (hypoxia)
Where oxygen levels are low, oxyhaemoglobin breaks down, releasing oxygen. In the tissues, which constantly consume oxygen, oxygen levels are always low. This encourages oxyhaemoglobin to release its oxygen to the cells. In addition, the lower the tissue oxygen level, the more oxygen is released, meaning that as tissue oxygen demand rises, so does the supply to match it. On the other hand, when oxygen levels are high, as they are in the lungs, oxyhaemoglobin formation is favoured.
Temperature
Actively metabolising tissues, which have higher than normal oxygen needs, are warmer than less active ones, which drive the equation above to the left, increasing oxygen release. This ensures that very active tissues receive a higher oxygen supply than less active ones. In the lungs, where the alveoli are exposed to inspired air, the temperature is lower, favouring oxyhaemoglobin formation.
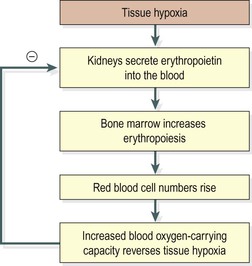
Control of erythropoiesis
Red cell numbers remain fairly constant, because the bone marrow produces erythrocytes at the rate at which they are destroyed. This is due to a homeostatic negative feedback mechanism. The hormone that regulates red blood cell production is erythropoietin, produced mainly by the kidney.
The primary stimulus to increased erythropoiesis is hypoxia, i.e. deficient oxygen supply to body cells.
Hypoxia can result from anaemia, low blood volume, poor blood flow, reduced oxygen content of inspired air (as at altitude) or lung disease. Each of these leads to erythropoietin production in an attempt to restore oxygen supplies to the tissues.
Erythropoietin stimulates an increase in the production of proerythroblasts and the release of more reticulocytes into the blood. It also speeds up reticulocyte maturation. These changes increase the oxygen-carrying capacity of the blood and reverse tissue hypoxia, the original stimulus. When the tissue hypoxia is overcome, erythropoietin production declines (Fig. 4.7). When erythropoietin levels are low, red cell formation does not take place even in the presence of hypoxia, and anaemia (the inability of the blood to carry adequate oxygen for body needs) develops.
Destruction of erythrocytes
The life span of erythrocytes (Fig. 4.5) is about 120 days and their breakdown, or haemolysis, is carried out by phagocytic reticuloendothelial cells. These cells are found in many tissues but the main sites of haemolysis are the spleen, bone marrow and liver. As erythrocytes age, their cell membranes become more fragile and so more susceptible to haemolysis. Iron released by haemolysis is retained in the body and reused in the bone marrow to form new haemoglobin molecules. Biliverdin is formed from the haem part of the haemoglobin. It is almost completely reduced to the yellow pigment bilirubin, before being bound to plasma globulin and transported to the liver (Fig. 4.5, see also Fig. 12.37, p. 311). In the liver it is changed from a fat-soluble to a water-soluble form to be excreted as a constituent of bile.
Blood groups  4.3
4.3
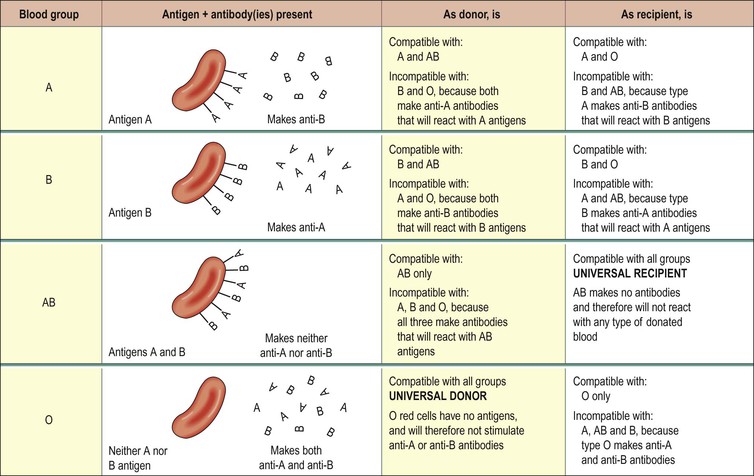
Early attempts to transfuse blood from one person to another or from animals to humans were only rarely successful, the recipient of the blood usually becoming very ill or dying. It is now known that the surface of red blood cells carries a range of different proteins (called antigens) that can stimulate an immune response if transferred from one individual (the donor) into the bloodstream of an incompatible individual. These antigens, which are inherited, determine the individual’s blood group. In addition, individuals can make antibodies to these antigens, but not to their own type of antigen, since if they did the antigens and antibodies would react, causing a potentially fatal transfusion reaction.
If individuals are transfused with blood of the same group, i.e. possessing the same antigens on the surface of the cells, their immune system will not recognise them as foreign and will not reject them. However, if they are given blood from an individual of a different blood type, i.e. with a different type of antigen on the red cells, their immune system will generate antibodies to the foreign antigens and destroy the transfused cells. This is the basis of the transfusion reaction; the two blood types, the donor and the recipient, are incompatible.
There are many different collections of red cell surface antigens, but the most important are the ABO and the Rhesus systems.
The ABO system
About 55% of the population has either A-type antigens (blood group A), B-type antigens (blood group B) or both (blood group AB) on their red cell surface. The remaining 45% have neither A nor B type antigens (blood group O). The corresponding antibodies are called anti-A and anti-B. Blood group A individuals cannot make anti-A (and therefore do not have these antibodies in their plasma), since otherwise a reaction to their own cells would occur; they can, however, make anti-B. Blood group B individuals, for the same reasons, can make only anti-A. Blood group AB make neither, and blood group O make both anti-A and anti-B (Fig. 4.8).
Because blood group AB people make neither anti-A nor anti-B antibodies, they are sometimes known as universal recipients: transfusion of either type A or type B blood into these individuals is likely to be safe, since there are no antibodies to react with them. Conversely, group O people have neither A nor B antigens on their red cell membranes, and their blood may be safely transfused into A, B, AB or O types; group O is sometimes known as the universal donor. The terms universal donor and universal recipient are misleading, however, since they imply that the ABO system is the only one that needs to be considered. In practice, although the ABO systems may be compatible, other antigen systems on donor/recipient cells may be incompatible, and cause a transfusion reaction (p. 76). For this reason, prior to transfusion, cross-matching is still required to ensure that there is no reaction between donor and recipient bloods. Inheritance of ABO blood groups is described in Chapter 17 (p. 444).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree