Chapter 7 The abdomen
SYMPTOMS OF ABDOMINAL DISORDERS
Gastrointestinal diseases
DYSPHAGIA
Dysphagia caused by a carcinoma usually progresses rapidly over 6–10 weeks and is worse for solids than liquids. Profound weight loss results from reduced food intake and the wasting effect of the cancer.
NAUSEA
Nausea usually comes in waves and is often associated with belching. The symptom may be provoked by unpleasant sights, smells and tastes or by abnormal stimulation or the inner-ear labyrinths (motion sickness). It is a characteristic of the prodromal phase of viral hepatitis and often accompanies biliary disease. Drugs causing gastric irritation (e.g. non-steroidal analgesics) or those stimulating the vomiting centre (e.g. digoxin) cause nausea. Early-morning nausea commonly occurs during the first trimester of pregnancy.
VOMITING AND HAEMATEMESIS
 Differential diagnosis: Gastrointestinal bleeding
Differential diagnosis: Gastrointestinal bleeding
| Cause | Frequency (%) |
|---|---|
| Gastric ulcer | 30 |
| Duodenal ulcer | 21 |
| Gastritis or erosions | 9 |
| Oesophagitis or oesophageal ulcer | 8 |
| Duodenitis | 4 |
| Varices | 3 |
| Tumours | 2 |
| Mallory–Weiss tear | 1 |
| Others | 22 |
a Mallory–Weiss tear, which results from mechanical disruption of the mucosa at the gastro-oesophageal junction. Enquire about ingestion of alcohol or other gastric irritants (e.g. aspirin). If there is evidence of coincident liver disease, consider oesophageal varices to be the cause of bleeding. Weight loss may suggest bleeding from a gastric cancer, and a history of epigastric pain or heartburn suggests bleeding from a peptic ulcer or ulcerated oesophagus.
ABDOMINAL PAIN
Visceral pain is caused by stretching or inflammation of a hollow muscular organ (gut, gallbladder, bile duct, ureters, uterus). It is perceived near the midline, irrespective of the location of the organ (Fig. 7.1). Visceral pain may also radiate to specific sites and this helps to establish its origin (Fig. 7.2).
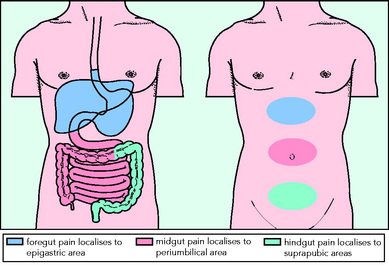
Fig. 7.1 Perception of visceral pain is localised to the epigastric, umbilical or suprapubic region according to the embryological origin of the diseased organ.
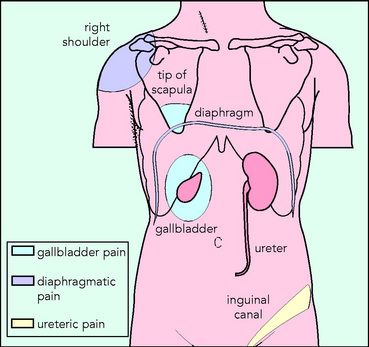
Fig. 7.2 Characteristic radiation of pain from the gallbladder, diaphragm and ureters. The pain is not always felt in the organ
WIND
Excessive belching (flatulence) or the passage of wind through the anus (flatus) are common symptoms. These symptoms are rather unspecific and occur in both functional and organic disorders of the gastrointestinal tract.
CHANGE IN BOWEL HABIT
Rectal bleeding
Bright-red rectal bleeding usually arises from the sigmoid colon or rectum and more proximal colonic bleeding is often a darker red or maroon colour. In haemorrhoidal bleeding the blood may be most noticeable on the toilet paper. Colon cancer and polyps often present with intermittent rectal bleeding, whereas patients with inflammatory bowel disease pass blood, often mixed with mucus, with each stool. Torrential haemorrhage may occur from diverticular disease and marked bleeding may occur in mesenteric vascular disease. Microscopic blood loss (occult bleeding) usually presents with symptoms of anaemia. Always consider a diagnosis of gastric, caecal or colon cancer in older patients with unexplained iron-deficiency anaemia.

 Questions to ask: Dysphagia
Questions to ask: Dysphagia Differential diagnosis: Dysphagia
Differential diagnosis: Dysphagia Questions to ask: Weight loss
Questions to ask: Weight loss Risk factors: Dyspepsia
Risk factors: Dyspepsia Differential diagnosis: Dyspepsia
Differential diagnosis: Dyspepsia Emergency: Assessment of patient presenting with haematemesis and melena
Emergency: Assessment of patient presenting with haematemesis and melena Questions to ask: Abdominal pain
Questions to ask: Abdominal pain Differential diagnosis: Constipation
Differential diagnosis: Constipation Questions to ask: Diarrhoea
Questions to ask: Diarrhoea Risk factors: Factors predisposing to hepatitis B
Risk factors: Factors predisposing to hepatitis B

