Systemic Disease
Diane C. Farhi
ENDOCRINE AND RENAL DISORDERS
Hyperthyroidism
Hyperthyroidism has been associated with diverse hematologic effects (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14). The peripheral blood may show erythrocytosis, microcytic or normocytic anemia, or pancytopenia. Anemia may be unresponsive to erythropoietin. Cytopenias are reversible with appropriate therapy for hyperthyroidism.
The bone marrow aspirate and biopsy may show hypercellularity, arrested hematopoiesis, ringed sideroblasts, and’or osteoporosis. Myelodysplastic changes may be present, reversible with therapy for hyperthryoidism.
Concomitant autoimmune disease may be present, including immune-mediated hemolytic anemia and thrombocytopenia and pernicious anemia.
Complications of antithyroid medications include agranulocytosis, granulocytic maturation arrest and aplasia, sideroblastic anemia, aplastic anemia, and reactive bone marrow plasmacytosis.
Hypothyroidism
Hypothyroidism has been associated with decreased red blood cell mass and plasma volume (15, 16, 17, 18, 19, 20, 21). The peripheral blood characteristically shows macrocytic anemia with acanthocytes; however, the red blood cells may be normocytic or microcytic in some cases. Maturation is not megaloblastic. The reticulocyte count is normal or decreased.
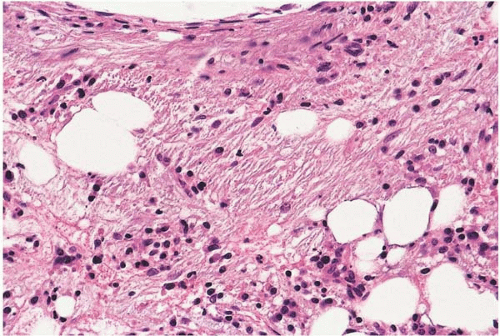
Severe hypothyroidism may be accompanied by pancytopenia, marrow hypoplasia, and myxedema or gelatinous transformation of the marrow (Fig. 14.1). Amyloidosis has been reported.
Hyperparathyroidism
Hyperparathyroidism, whether primary or secondary, produces effects on the bone marrow. Primary hyperparathyroidism is associated with anemia, marrow fibrosis, and osteosclerosis (22,23). Secondary hyperparathyroidism and its effects on bone are often seen in chronic renal failure, but may also be caused by aluminum accumulation, vitamin D deficiency, and tumor production of parathyroid-hormonerelated protein (see Fig. 12.9) (24, 25, 26, 27, 28, 29, 30, 31, 32).
Hypoparathyroidism
Chronic Renal Failure
Patients with chronic renal failure undergo numerous hematopoietic changes (37, 38, 39, 40, 41, 42, 43, 44, 45). Laboratory studies usually show anemia, the result of decreased renal erythropoietin production. The red blood cells are usually normocytic, but may be microcytic or macrocytic; they are usually normochromic or hypochromic. The mean hemoglobin level is 61 g’L. The reticulocyte count is decreased. The severity of anemia directly correlates with the degree of azotemia. Other specific causes of anemia include vitamin and iron deficiencies, blood loss, inflammation, and aluminum intoxication.
The bone marrow shows osteomalacia due to secondary hyperparathyroidism in uncontrolled renal failure (Fig. 12.9).
Other bone marrow changes due to renal failure and’or hemodialysis include β2-microglobulin-related amyloidosis, eosinophilia, histiocytic and giant cell reactions to silicone in dialysis tubing, and macrophage storage of aluminum.
IMMUNE AND RELATED DISORDERS
Common Variable Immunodeficiency
Common variable immunodeficiency (CVID) is associated with numerous hematopoietic abnormalities (46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58). Patients may present with infection. Laboratory studies show decreases in serum immunoglobulin levels, decreased circulating B cells, and abnormal T-cell function.
The peripheral blood may show anemia and T-γ-δ-cell lymphocytosis. Autoimmune anemia and’or autoimmune thrombocytopenia are frequently found. Cyclic neutropenia
and cyclic thrombocytopenia have been reported. The bone marrow may show noncaseating granulomas.
and cyclic thrombocytopenia have been reported. The bone marrow may show noncaseating granulomas.
Complications of CVID include systemic granulomatous disease, opportunistic infection, acute lymphoblastic leukemia, Hodgkin lymphoma, B-cell lymphoma, and T-cell lymphoma.
Connective Tissue Disease
Connective tissue disease is comprised of numerous disorders, including adult Still disease, rheumatoid arthritis, Sjögren syndrome, systemic lupus erythematosus, and others. These are accompanied by a wide variety of hematopoietic changes (Figs. 14.2 and 14.3) (59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree