Systemic B-cell Lymphomas Involving the Skin
Aaron Auerbach, MD, PhD
Key Facts
Terminology
B-cell lymphoma that has spread to skin as a secondary site of disease
Clinical Issues
Systemic B-cell lymphoma more often involves skin, compared to systemic T-cell lymphoma
Single or multiple lesions, usually tumors or nodules
May present at diagnosis or develop during disease progression
Often requires aggressive chemotherapy
Higher stage than primary cutaneous lymphomas
Generally, much worse prognosis than primary cutaneous lymphoma
Top Differential Diagnoses
Hodgkin lymphoma
Direct extension to chest by tumor cells in patients with mediastinal disease
Reed-Sternberg cells CD30(+), CD15(+), pax-5(+), EBER(+)
Mantle cell lymphoma
CD5(+), cyclin-D1(+), CD43(+), Bcl-2(+), t(11;14)(+)
Burkitt lymphoma
CD10(+), Bcl-6(+), Bcl-2(−), t(8;14)(+)
SLL/CLL
CD5(+), CD23(+), cyclin-D1(−)
Follicular lymphoma
CD10(+), Bcl-6(+)
Often Bcl-2(+), unlike primary cutaneous follicle center lymphoma
Often t(14;18)(+), unlike primary cutaneous follicle center lymphoma
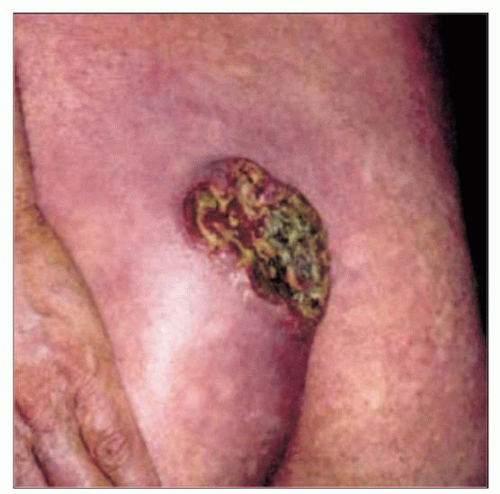 This clinical photograph of cutaneous Hodgkin lymphoma shows a solitary ulcerating skin lesion. The lesion in the left gluteal area enlarged from 2-10 cm over several months. (Courtesy C. Hsai, MD.) |
TERMINOLOGY
Synonyms
Secondary cutaneous B-cell lymphoma
Definitions
B-cell lymphoma that has spread to skin as a secondary site of disease
ETIOLOGY/PATHOGENESIS
Infectious Agents
EBV infection in some lymphomas
Radiation
Can be therapy related
CLINICAL ISSUES
Epidemiology
Incidence
Systemic B-cell lymphoma more often involves skin, compared to systemic T-cell lymphoma
25% of systemic peripheral T-cell lymphomas also have skin lesions
Age
Any age, but mostly adults
Gender
Occurs in both males and females
Presentation
Single or multiple lesions, usually tumors or nodules
Any cutaneous site; no site of predilection
Skin involvement may present at diagnosis or develop later
Treatment
Adjuvant therapy
Frequently aggressive chemotherapy, unlike most primary cutaneous B-cell lymphomas
Prognosis
Higher stage than primary cutaneous lymphoma
Usually much worse prognosis than primary cutaneous lymphoma
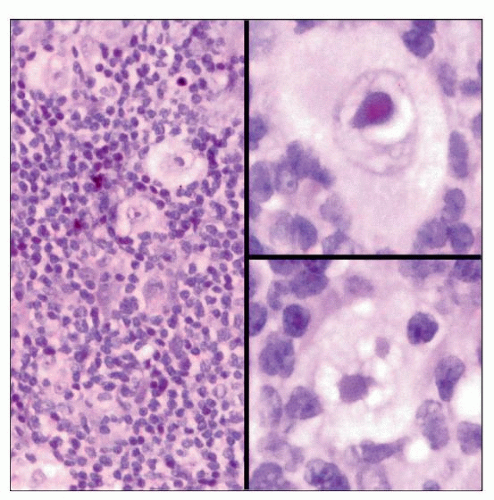
MICROSCOPIC PATHOLOGY
Histologic Features
Depend on type of lymphoma
Morphology and immunophenotype often identical to systemic disease
DIFFERENTIAL DIAGNOSIS
Hodgkin Lymphoma
Rare skin involvement, unlike non-Hodgkin B-cell lymphoma
Skin lesion in < 5% of cases and < 1% at presentation, more common in immunosuppressed
Extremely poor prognosis
Microscopic features
Scattered Reed-Sternberg cells with multinucleated giant cells, enlarged nuclei, and > 1 nucleoli sitting within lacunae
Many small lymphocytes, eosinophils, and plasma cells
Sometimes collagen bands
Most common subtype is nodular sclerosing Hodgkin lymphoma
Lymphocyte predominant Hodgkin lymphoma not reported in skin
Immunohistochemistry
Reed-Sternberg cells positive for CD15, CD30, pax-5, LMP, CD20 (weak), and EBER
Rarely (+) for T-cell antigens and show T-cell receptor gene rearrangement
Must differentiate from anaplastic large cell lymphoma, which is CD30(+), CD15(−), pax-5(−), LMP(−), EBER(−)
Presentation
Single or multiple dermal or subcutaneous nodules
Usually direct extension to skin (chest) by tumor cells in patients with mediastinal disease
Rare primary skin cases
Sometimes pruritus, hyperpigmentation, or urticaria, may be due to paraneoplastic syndrome, and not tumor
Non-Hodgkin B-cell Lymphoma
Mantle cell lymphoma
Involves skin ≤ 2% of cases
Primary to skin, extremely rare
Presentation
Often multiple macules, papules, plaques, or nodules on trunk or extremities
Microscopic features
Nodular, diffuse, mantle zone or follicular growth pattern
B cells in dermis with grenz zone, often perivascular, sometimes surrounds reactive germinal center
Irregular nuclear contours, inconspicuous nucleoli
Scattered single epithelioid histiocytes
Blastoid variant may be more common in skin; has cells with dispersed chromatin, resembling lymphoblasts, or more atypia, similar to diffuse large B-cell lymphoma
Immunohistochemistry
B-cell marker positive CD5(+), cyclin-D1(+), CD23(−), CD43(+), Bcl-2(+)
Burkitt lymphoma
12% of Burkitt lymphoma at autopsy have skin lesions
Sometimes direct invasion from underlying lesion
Can relapse with cutaneous lesions
Presentation
Often in Africa (jaw tumors), in immunosuppressed, and in gastrointestinal tract
Often infection with Epstein-Barr virus
Microscopic features
Patchy dermal and subcutaneous infiltrate with grenz zone
Medium to large size B cells with squared-off borders (i.e., cobblestone or jigsaw puzzle)
Dispersed chromatin with multiple medium-sized nucleoli
Can have basophilic cytoplasm, especially on touch preparation
↑ mitosis and apoptosis
Tingible body macrophages creates “starry sky” appearance
Immunohistochemistry
B-cell markers including CD20(+), CD10(+), Bcl-6(+), Bcl-2(−) (usually)
Small lymphocytic lymphoma/chronic lymphocytic leukemia (SLL/CLL)
2% show skin lesions, usually already peripheral blood involvement
No apparent worse prognosis with skin involvement
Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree