Patient Story
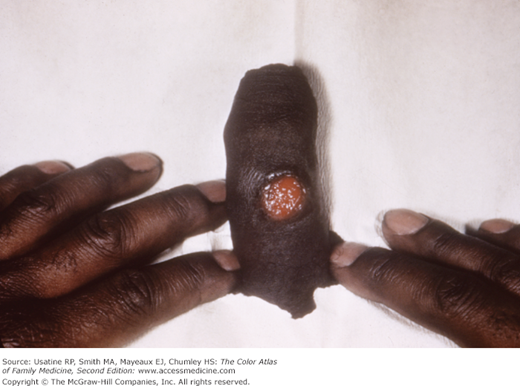
A 39-year-old woman presents with a nonhealing ulcer over her upper lip for 1 week and a new-onset rash on her trunk (Figures 216-1 and 216-2). The ulcer on her upper lip was misdiagnosed as herpes simplex by the previous physician. Sexual history revealed that the patient had oral sex with a boyfriend who had a lesion on his penis and she suspected that he had been having sex with other women. The examining physician recognized the nonpainful ulcer and rash as a combination of primary and secondary (P&S) syphilis. An RPR (rapid plasma reagin) was drawn and the patient was treated immediately with IM benzathine penicillin. The RPR came back as 1:128 and the ulcer was healed within 1 week.
Figure 216-2
A nonpruritic rash of secondary syphilis on the abdomen of the patient shown in Figure 216-1. (Courtesy of Richard P. Usatine, MD.)
Introduction
Syphilis, caused by Treponema pallidum, is a systemic disease characterized by multiple overlapping stages: primary syphilis (ulcer), secondary syphilis (skin rash, mucocutaneous lesions or lymphadenopathy), tertiary syphilis (cardiac or gummatous lesions), and early or late latent syphilis (positive serology without clinical manifestations). Neurosyphilis can occur at any stage. Diagnosis is made using treponemal and nontreponemal tests. Treatment is penicillin; the dose and duration depend on the stage.
Synonyms and Acronyms
Epidemiology
- Primary and secondary (P&S) syphilis cases reported to CDC decreased from 13,997 in 2009 to 13,774 in 2010, a decrease of 1.6%. The rate of P&S syphilis in the US in 2010 (4.5 cases per 100,000 population) was 2.2% lower than the rate in 2009 (4.6 cases). This is the first overall decrease in P&S syphilis in 10 years.1
- The rate of P&S syphilis increased 1.3% among men (from 7.8 to 7.9 cases per 100,000 men) during 2009-2010. During this same period, the rate decreased 21.4% among women (from 1.4 to 1.1 cases per 100,000 women).1
- In 2010, the rate of P&S syphilis was highest among persons aged 20-24 years and 25-29 years (13.5 and 11.3 cases per 100,000 population, respectively).1
- The distribution of primary and secondary syphilis reported in 2010 differed by gender and sexual preferences: among men who have sex with women only (MSW), 35.8% had primary syphilis, and 64.2% had secondary syphilis. Among women, 16.0% had primary syphilis, and 84.0% had secondary syphilis. Among men who have sex with men (MSM), 25.0% had primary syphilis, and 75.0% had secondary syphilis.1
- Syphilis by races/ethnicities varied in 2010: Among women with P&S syphilis, 16.8% were white, 72.8% were black, 6.6% were Hispanic. Among MSW, 14.8% were white, 67.0% were black, 13.8% were Hispanic. Among MSM, 38.1% were white, 37.0% were black, 19.8% were Hispanic.1
- In 2008, 63% of the reported cases of P&S were in men who have sex with men (MSM).2
- HIV-infected patients were found to have syphilis rates of 62.3 per 1000 compared to 0.8 per 1000 in HIV-uninfected patients in a population study in California.3
Etiology and Pathophysiology
Risk Factors
Diagnosis
- Primary syphilis is associated with a chancre—Usually a nonpainful ulcer (Figures 216-1, 216-3, and 216-4). The presence of pain does not rule out syphilis, and the patient with a painful genital ulcer should be tested for both syphilis and herpes.
- Secondary syphilis occurs when the spirochetes become systemic and may present as a rash with protean morphologies, condyloma lata, and/or mucous patches (Figures 216-2 and 216-5, 216-6, 216-7, 216-8, 216-9, 216-10, and 216-11).
- Tertiary syphilis may be visualized with gummas on the skin, but many of the manifestations are internal such as the cardiac and neurologic diseases that occur (e.g., aortitis, tabes dorsalis, and iritis). Figure 216-12 shows a gumma of the scrotum.
- Neurosyphilis can occur at any stage. Clinical symptoms include cognitive dysfunction, vision or hearing loss, uveitis or iritis, motor or sensory abnormalities, cranial nerve palsies, or symptoms of meningitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree