Surgically Assisted Endoscopic Retrograde Cholangiopancreatoscopy
Kfir Ben-David
Steven J. Hughes
DEFINITION
Surgical assistance to successfully perform endoscopic retrograde cholangiopancreatoscopy (ERCP) is necessary when intestinal continuity has been surgically modified such that the ampulla of Vater cannot be accessed via the mouth.
Previous gastric bypass with a long Roux-en-Y limb is the surgical procedure that leads to the need for surgically assisted ERCP.
The presence of a gastric remnant is essential to the performance of surgically assisted endoscopic retrograde cholangiopancreatoscopy (SA-ERCP).
Rarely, a clinical scenario may arise where surgical access to a gastric remnant may be indicated to facilitate endoscopic ultrasound (EUS).
As magnetic resonance cholangiopancreatography (MRCP) provides a noninvasive means to assess the pancreaticobiliary duct systems in most patients, ERCP is generally not indicated merely as a diagnostic modality—therapeutic intent is the indication for ERCP; this concept must be emphasized when considering SA-ERCP.
DIFFERENTIAL DIAGNOSIS
Choledocholithiasis
Sphincter of Oddi dysfunction
Ampulla of Vater pathology
Intraductal papillary mucinous neoplasm (IPMN)
Chronic pancreatitis
Disrupted pancreatic duct syndrome
PATIENT HISTORY AND PHYSICAL FINDINGS
Historically, the most common indication for SA-ERCP was for the diagnosis and treatment of sphincter of Oddi dysfunction (SOD)—a condition thought to be elicited by gastric bypass surgery. However, results from a recent study have led to serious concerns about the value of therapeutic intervention for symptoms attributed to SOD.1
A history of prior cholecystectomy must be obtained. If the gallbladder is in situ, a cholecystectomy is likely warranted as part of the SA-ERCP.
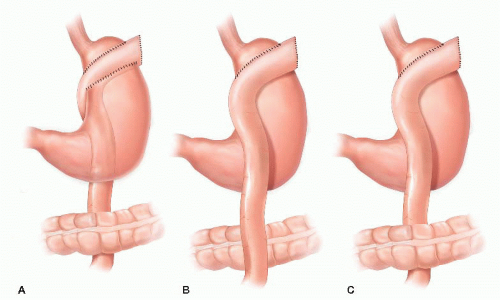
The gastric bypass operative note must be reviewed. The location of the Roux limb with respect to the gastric remnant and transverse colon must be known preoperatively and this information factored into the counseling the patient as to the risks of the procedure—an antegastric and/or an antecolic Roux limb will increase the technical complexity and thus risk (FIG 1).
Specifically review any potential allergy to iodinated contrast agents. Medical preparation to mitigate an allergic reaction may be indicated.
SURGICAL MANAGEMENT
Preoperative Planning
The potential need for serial ERCP procedures should be determined. A gastrostomy tube (G-tube) can be placed at the index procedure to facilitate subsequent endoscopic interventions. Potentially affected patients should be prepared for this possibility.
These operations require significant coordination between multidisciplinary teams. The authors highly recommend that these procedures be scheduled as the first case of the day.
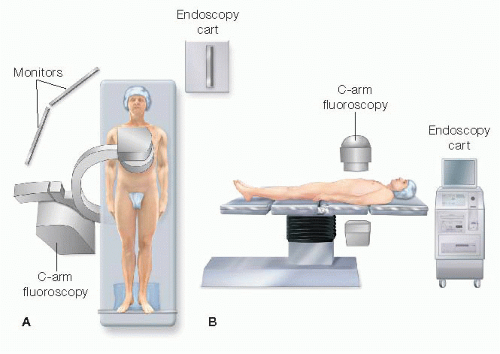
The procedure needs to be scheduled in a room that can accommodate two teams, a C-arm fluoroscopy unit, and a mobile endoscopy cart.
Positioning
The operative table should be configured so that C-arm fluoroscopy can be readily performed of the upper abdomen (FIG 2).
After induction of general anesthesia, a urinary bladder catheter is placed. An orogastric tube is rarely necessary.
The patient is positioned supine, ideally with both arms tucked to facilitate access for both C-arm fluoroscopy and the endoscopy team. A footboard is placed. A fixed liver retractor can be positioned on either side of the patient if needed.
Venous thromboembolism prophylaxis (both mechanical and pharmacologic) should be used. Antibiotics are administered within the guidelines of Surgical Care Improvement Program (SCIP) criteria for a clean-contaminated procedure.
TECHNIQUES
TROCAR PLACEMENT
Trocar placement is depicted in FIG 3. Four trocars will be required for placement of stay sutures in the stomach, and one of these can be subsequently used for clamping of the small bowel. A subxiphoid, transgastric trocar is also necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree