Superficial Malignant Peripheral Nerve Sheath Tumor
David R. Lucas, MD
Key Facts
Terminology
Superficial sarcoma arising from cutaneous nerve or benign nerve sheath tumor, or showing nerve sheath differentiation
Etiology/Pathogenesis
40% associated with NF1
Clinical Issues
Mostly adults, but wide age range (4-79 years)
Local recurrence: 60%
Metastasis: 25%
Microscopic Pathology
Mostly intermediate and high-grade sarcomas
Spindle cell pattern most common
Long fascicles of closely spaced hyperchromatic spindle cells
Wavy nuclei with tapered ends
Small round blue cells
Pleomorphic cells
Extensive necrosis with perivascular preservation
Epithelioid MPNST
Heterologous differentiation
Ancillary Tests
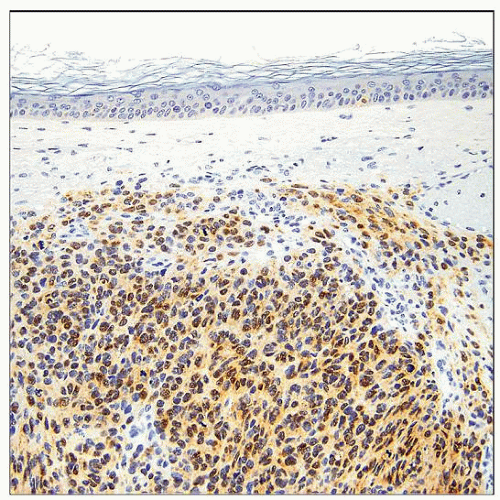
S100 protein (+) in about 60% of cases (more often in well-differentiated and epithelioid MPNST), usually focal
Top Differential Diagnoses
Malignant melanoma
Atypical neurofibroma
Dermatofibrosarcoma protuberans
Clear cell sarcoma
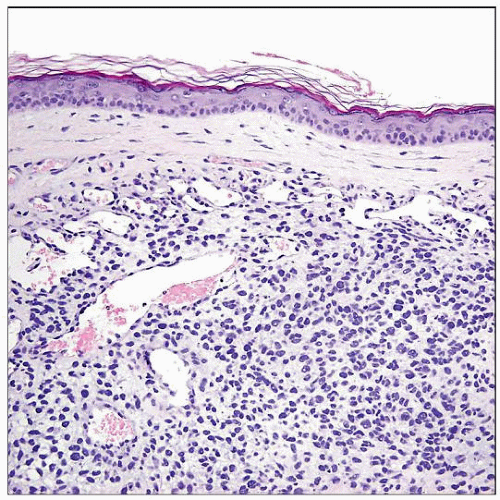 MPNST can rarely present as a primary skin tumor, such as this scalp tumor excised from a 90-year-old woman. Superficial MPNST typically occurs in mid-to-deep dermis or as a subcutaneous primary. |
TERMINOLOGY
Abbreviations
Malignant peripheral nerve sheath tumor (MPNST)
Synonyms
Neurofibrosarcoma, “malignant schwannoma” (older terms)
Definitions
Superficial sarcoma arising from cutaneous nerve or benign nerve sheath tumor, or showing nerve sheath differentiation
Diagnostic criteria
Arises from nerve or benign nerve sheath tumor
Or shows histological evidence of nerve sheath differentiation in a NF1 patient
Or shows histological plus immunohistochemical or ultrastructural evidence of nerve sheath differentiation in non-NF1 patient
ETIOLOGY/PATHOGENESIS
Genetic Predisposition
40% associated with neurofibromatosis type 1 (NF1)
Lifetime incidence: 2-16%
Molecular Pathogenesis
NF1 caused by germline mutation of NF1 tumor suppressor gene
Somatic loss of 2nd NF1 allele required for tumorigenesis
Malignant transformation in both NF1-associated and sporadic MPNST often involves INK4A and P53 and their downstream pathways
CLINICAL ISSUES
Epidemiology
Incidence
MPNST accounts for 5-10% of soft tissue sarcomas
Superficial MPNST very rare
Age
Mostly adults (20-50 years)
Average: 40 years
Wide range: 4-79 years
Gender
Women and men roughly equal
Site
Head and neck (60%), trunk, upper and lower extremities
Dermis &/or subcutis
Mid- or deep dermis in most cases
May invade deeper structures
Presentation
Painful or painless mass
Treatment
Surgical approaches
Wide excision/resection
Adjuvant therapy
Radiation
Drugs
Generally MPNST shows poor response to chemotherapy
Prognosis
Local recurrence: 60%
Metastasis: 25%
Lung, lymph node, bone
30% die of disease
Average survival: 3.3 years
IMAGE FINDINGS
General Features
Morphology
Cutaneous nodule
Superficial soft tissue mass
MACROSCOPIC FEATURES
General Features
Epidermal alterations absent
Coexisting neurofibroma in some cases
Size
Average: 3 cm (range: 2-16 cm)
MICROSCOPIC PATHOLOGY
Histologic Features
Wide spectrum of cytoarchitectural patterns
Mostly intermediate or high-grade sarcomas
High mitotic rate and necrosis
Only around 15% are low grade
Nerve sheath differentiation
Nuclear palisading uncommon, usually focal
Tactoid differentiation with whorling or Wagner-Meissner body-like features
Intraneural tumors
Plexiform architecture
Microscopic extension within nerve fascicle
Tumors arising from preexisting benign nerve sheath tumor
Neurofibroma most common, transitional areas, usually in NF1 patients
Diffuse infiltrative sarcomatous proliferation without evidence of nerve or nerve sheath tumor origin
Spindle cell MPNST (most common pattern)
Long fascicles of uniform, closely spaced, hyperchromatic spindle cells
Alternating cellular fascicles and hypocellular areas (“tapestry” or “marbled” pattern)
Myxoid matrix, focal
Storiform arrays
Wavy nuclei with tapered ends
Small round blue cells
Pleomorphic cells
Multinucleated giant cells
Extensive necrosis with perivascular preservation
Epithelioid MPNST
Multinodular architecture
Cords and clusters in some
Large epithelioid cells
Abundant eosinophilic cytoplasm
Large vesicular nuclei with macronucleoli
Clear cytoplasm in some
Often mixed with spindle cells
Heterologous differentiation (15% of MPNSTs)
Osseous and osteosarcomatous
Chondroid and chondrosarcomatous
Rhabdomyosarcomatous (Triton tumor)
Angiosarcomatous
Glandular
Cytologic Features
Spindle cells
Ill-defined cytoplasm
Hyperchromatic nucleus with dispersed coarse chromatin
Tapered and wavy nuclei in well-differentiated tumors
Very brisk mitotic activity in high-grade tumors
Epithelioid cells
Abundant eosinophilic or clear cytoplasm
Vesicular nucleus with prominent inclusion-like nucleolus
ANCILLARY TESTS
Immunohistochemistry
S100 protein (+) in about 60% of cases (more often in well-differentiated and epithelioid MPNST), usually focal