Patient Story
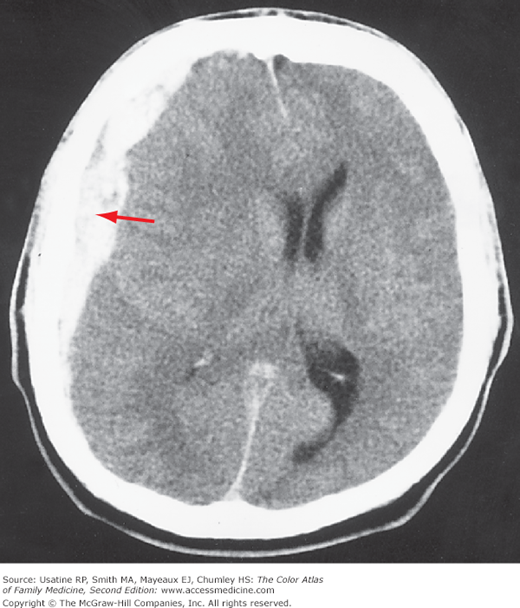
A 34-year-old driver was hit from behind at approximately 25 mph. He hit his head, but did not lose consciousness and did not seek care. Approximately 12 hours later, he developed a headache and confusion, and was taken to the emergency department by a family member. He was found to have an acute subdural hematoma (Figure 231-1). He was hospitalized, and a neurosurgeon was consulted for surgical management.
Figure 231-1
CT scan of an acute subdural hematoma (arrow) seen as a hyperdense clot with an irregular border. There is a midline shift from the mass effect of the accumulated blood. (Courtesy of Kasper DL, Braunwald E, Fauci, AS, Hauser SL, Longo DL, Jameson JL. Harrison’s Principles of Internal Medicine, 16th ed. New York, NY: McGraw-Hill; 2005:2450.)
Introduction
Subdural hematomas (SHs) can occur at any age, but are most common in infants and older adults. Most SHs are caused by trauma. Symptoms are generally nonspecific such as irritability or poor feeding in infants and confusion or headaches in adults. Treatment is prompt consultation with a neurosurgeon.
Epidemiology
- SHs occur at all ages. In adults, SHs are more common in men.1
- Eight percent of asymptomatic newborns can have an SH.2
- Twenty-four of 100,000 infants ages 0 to 1 year in United Kingdom population studies.3
- Less than 1 in 100,000 adults per year have a traumatic SH.1
- Forty-two of 100,000 hospitalizations for adult patients.4
- Cost is $1.6 billion per year in 2007 dollars.4
- Mortality rates in treated older adults are approximately 8% for patients younger than age 65 years and 33% for patients older than age 65 years.5
Etiology and Pathophysiology
- Most SHs are caused by trauma, either accidental or intentional, from a direct injury to the head or shaking injury in an infant.
- Falls, motor vehicle accidents, and assault are the most common causes of traumatic SH.1
- SHs have been reported from chronic jarring from rapid walking in older patients and can occur during a nontraumatic birth.
- Motion of the brain within the skull causes a shearing force to the cortical surface and interhemispheric bridging veins.3
- This force tears the weakest bridging veins as they cross the subdural space, resulting in an acute SH as seen in Figure 231-1.3
- Three days to 3 weeks after the injury, the body breaks down the blood in an SH; water is drawn into the collection causing hemodilution, which appears less white and more gray on noncontrast CT.3
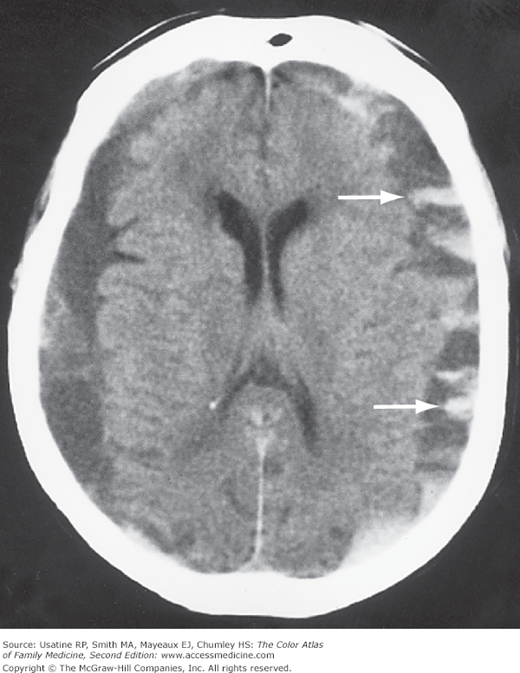
- If the hematoma fails to resolve, the collection has an even higher content of water and appears darker on a noncontrast CT; it may have fresh bleeding or may calcify (chronic SH; Figure 231-2).3 This is often of the same color as brain parenchyma on noncontrast CT.
- Nontraumatic causes reported in the literature include spontaneous bleeding because of bleeding disorders or anticoagulation, meningitis, and complications of neurologic procedures, including spinal anesthesia.
Figure 231-2
CT scan of chronic bilateral subdural hematomas. As subdural hematomas age, these become isodense gray and then hypodense (darker gray to black) compared to the brain. Some resolving blood is still visible on the left (arrows). (Courtesy of Kasper DL, Braunwald E, Fauci, AS, Hauser SL, Longo DL, Jameson JL. Harrison’s Principles of Internal Medicine, 16th ed. New York, NY: McGraw-Hill; 2005:2450.)
Risk Factors
Diagnosis
The clinical features are often nonspecific, making the diagnosis difficult in the absence of known trauma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree