Subcutaneous Panniculitis-like T-cell Lymphoma
Aaron Auerbach, MD, PhD
Key Facts
Terminology
T-cell lymphoma of αβ cells usually involving subcutaneous tissue with prominent karyorrhexis and cytotoxic phenotype
Cases composed of γδ cells are reclassified as cutaneous γδ T-cell lymphomas
Clinical Issues
20% hemophagocytic syndrome
Excellent prognosis
Microscopic Pathology
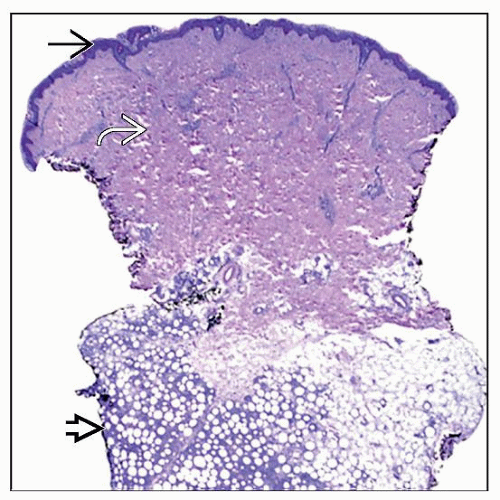
Atypical lobular panniculitic T-cell infiltrate confined to subcutis
Malignant T cells rim around adipocytes
Prominent necrosis/apoptosis and angioinvasion
Vacuolated histiocytes
Ancillary Tests
Immunohistochemistry, TCR-βF1(+), TCR-δ(−), CD8(+), CD4(−), CD56(−), EBER(−)
(+) for cytotoxic markers
T-cell receptor gene rearrangement
Top Differential Diagnoses
Cutaneous γ/δ T-cell lymphoma
Panniculitis, but also in dermis &/or epidermis with ulceration, TCR-βF1(−), TCR-δ(+)
Worse prognosis than SPTCL
Lupus profundus panniculitis
Similar inflammation in subcutis in panniculitic pattern
Lobular panniculitis, but shows plasma cells and germinal centers unlike SPTCL
 This clinical photograph shows a single nonulcerated subcutaneous nodule on the arm of a 35-year-old patient. Upon excision, the nodule was diagnosed as SPTCL. (Courtesy M. Tomaszewsky, MD.) |
TERMINOLOGY
Abbreviations
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL)
Definitions
T-cell lymphoma of αβ cells involving subcutaneous tissue with prominent karyorrhexis and cytotoxic phenotype
Cases composed of γδ cells are reclassified as cutaneous γδ T-cell lymphoma in the WHO Classification of Hematopoietic and Lymphoid Tumors
Subcutaneous T-cell lymphomas of γδ type are more aggressive than αβ cases
ETIOLOGY/PATHOGENESIS
Autoimmune Disease
Autoimmune disease present in ˜ 20% of patients
Systemic lupus erythematosus (SLE) most common
Microscopic findings of SPTCL overlap with lupus profundus panniculitis
Viral Infection
Rarely, SPTCL is seen with Epstein-Barr virus infection
May be due to immunosuppression
CLINICAL ISSUES
Epidemiology
Incidence
< 1% of all non-Hodgkin lymphoma
Presents sporadically without familial involvement
Age
Median: ˜ 35 years (range: 5 months to 84 years)
20% < 20 years old
Rarely, children < 2 years old
Gender
Men = women
Ethnicity
No ethnic predisposition
Site
Extremities and trunk most common
Uncommonly disseminates
Can involve lymph nodes, but not at initial diagnosis
Presentation
Single or multiple erythematous subcutaneous nodules or plaques
Painless mass, rarely ulcerates
Symptoms due to mass effects
B symptoms in up to 50%
Diagnosis often not discovered until months to years after onset of symptoms
Hemophagocytic syndrome (HPS) in up to 20%
Related to release of cytotoxic molecules
May occur up to 5 years after presenting diagnosis
Laboratory Tests
Cytopenias (anemia, leukopenia, thrombocytopenia)
↑ liver function tests
↑ erythrocyte sedimentation rate, ↑ C-reactive protein
Treatment
Surgery
Sometimes excision of single lesion with no further recurrence
Immunosuppressive agents
Often given, at least initially
High-dose systemic corticosteroids
Chemotherapy
Recurrence or resistant cases treated with CHOP or CHOP-like therapy
Radiation
Sometimes for localized disease
Stem cell transplant
Can be considered for refractory/recurrent disease
Prognosis
Indolent disease
5-year overall survival ˜ 80%
Mostly stage I (confined to skin)
Rare systemic spread
Including lymph nodes
Often years after diagnosis
HPS poor prognostic indicator
Medium survival ˜ 2 years
IMAGE FINDINGS
CT Findings
Enhancing nodules in subcutaneous tissue
MICROSCOPIC PATHOLOGY
Histologic Features
Atypical T-cell infiltrate of subcutaneous fat lobules
Involves lobules, usually spares septa
Uncommon septal pattern represents spilling of T cells from lobules
Typically, no tumor in overlying dermis or epidermis
Malignant T cells rim individual adipocytes
Characteristic, but not specific for SPTCL
Neoplastic cells
Small to large in size
Mild to marked atypia with irregular nuclear contours
Hyperchromatic nuclei
Pale, clear cytoplasm
Karyorrhexis (apoptosis) and fat necrosis characteristic
Necrosis from released cytotoxic molecules
Initial biopsy commonly shows minimal T-cell atypia
Later biopsies show more atypia
Angioinvasion in some cases
Poor prognostic indicator
Reactive inflammatory cells
Histiocytes
Vacuolated foamy cytoplasm from imbibed material/lipid
Erythrophagocytosis or cytophagocytosis
Sometimes poorly formed granulomas with multinucleated giant cells
Usually lacks plasma cells, eosinophils, or neutrophils
ANCILLARY TESTS
Immunohistochemistry
T-cell antigens (+) (CD2, CD3, CD5, CD7)
May lack 1 or more T-cell antigens
CD8(+)/CD4(−) in > 95% of SPTCL
CD4(−)/CD8(−) and CD4(+)/CD8(−) rarely
TCR-βF1(+), TCR-δ-1(−) (alpha-beta T cells)
Cytotoxic markers (+) (perforin, TIA1, and granzyme)
But GZM-M negative, unlike other T-cell lymphomas
CD56(−), CD30(−), Bcl-2(−)
Cytogenetics
No specific cytogenetic abnormalities
In Situ Hybridization
Epstein-Barr encoded receptor (EBER) usually negative
Rare EBER(+) associated with immunocompromised and Asian patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree