Subcutaneous Panniculitis-like T-cell Lymphoma
Tariq Muzzafar, MBBS
Key Facts
Terminology
Cytotoxic T-cell lymphoma that preferentially involves subcutaneous tissue and expresses TCR-αβ
Definition of SPTCL substantially revised in WHO 2008 classification
Cases that express TCR-γδ are excluded
Clinical Issues
Patients present with solitary or multiple subcutaneous nodules or plaques
Legs > arms > trunk
Full-blown HPS arises in ˜ 15-20% of patients
SPTCL is clinically indolent
Recent trend toward using single immunosuppressive agents, at least initially
Multi-agent chemotherapy reserved for patients with progressive disease
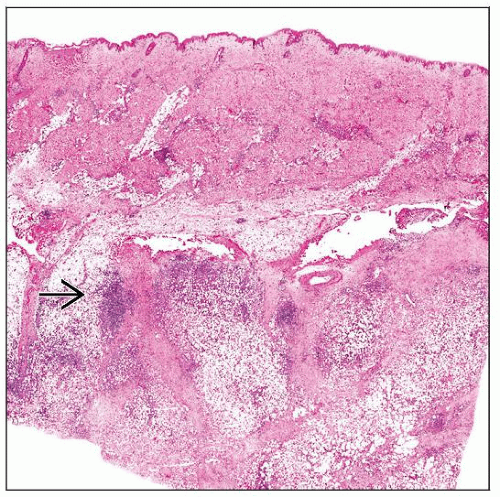
Microscopic Pathology
SPTCL primarily involves subcutaneous adipose tissue
Predominantly involves lobules and spares septa
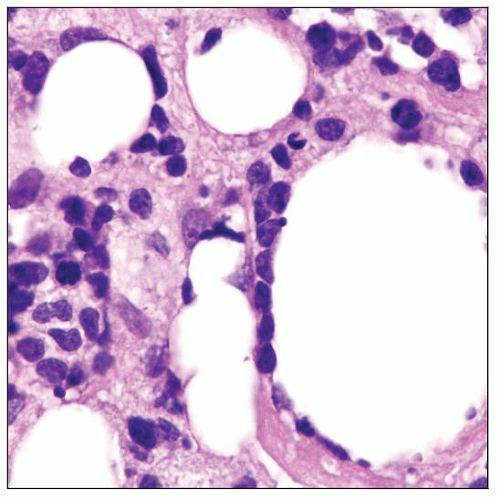
Neoplastic cells often rim individual adipocytes
Lymphoma cells small to intermediate in size
Apoptotic cells, karyorrhectic debris, fat necrosis
Ancillary Tests
βF1/TCR-αβ(+); pan-T-cell antigens(+)
CD8(+), CD4(-); cytotoxic proteins(+)
Monoclonal TCR gene rearrangements
Top Differential Diagnoses
Lupus erythematosus panniculitis
Primary cutaneous γ/δ T-cell lymphoma
Primary cutaneous CD30(+) lymphoproliferative disorders
TERMINOLOGY
Abbreviations
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL)
Synonyms
T-cell lymphoma involving subcutaneous tissue
Definitions
T-cell lymphoma that preferentially involves subcutaneous tissue and expresses T-cell receptor α/β and cytotoxic proteins
Definition of SPTCL was revised in World Health Organization (WHO) 2008 classification
Cases that express T-cell receptor γ/δ are now excluded
Instead, classified as primary cutaneous γ/δ T-cell lymphoma
In effect, SPTCL has become a more indolent disease by excluding patients with aggressive disease
ETIOLOGY/PATHOGENESIS
Infectious Agents
Rare cases of SPTCL are associated with Epstein-Barr virus infection
Usually in setting of immune suppression or dysregulation
e.g., methotrexate therapy for arthritis
Possible Role of Autoimmunity
Autoimmune diseases occur in ˜ 20% of patients
Systemic lupus erythematosus most common
Rheumatoid, juvenile rheumatoid, or psoriatic arthritis
Sjögren syndrome
Immune thrombocytopenic purpura
CLINICAL ISSUES
Epidemiology
Incidence
< 1% of non-Hodgkin lymphomas
Age
Median: ˜ 35 years (range: 9-79 years)
Gender
Female predominance (male:female ratio is 1:2)
Ethnicity
No ethnic predisposition
Site
Legs > arms > trunk (in frequency of involvement)
Lymph nodes are not involved at initial diagnosis
SPTCL can disseminate, though uncommon
Lymphadenopathy and leukemic phase of disease have been reported
Presentation
Patients present with solitary or multiple subcutaneous nodules or plaques
Size can range from 0.5-20 cm
Lesions often painless
Ulceration rare
Local symptoms related to ulceration or mass effect can occur
Skin lesions can regress, in part, and show a range in stages of “healing”
Systemic symptoms: ˜ 60% of patients
Fever most common; weight loss and night sweats can occur
Symptoms related to hemophagocytosis
Full-blown hemophagocytic syndrome (HPS) develops in ˜ 15-20% of patients
Hepatomegaly can occur; often associated with HPS
Substantial delay can occur between onset of symptoms and specific diagnosis of SPTCL
Laboratory Tests
Elevated erythrocyte sedimentation rate &/or C-reactive protein
Abnormalities often associated with onset of HPS
Anemia, leukopenia, thrombocytopenia
Elevated liver function tests
Natural History
SPTCL is clinically indolent
Disease can wax and wane
Prolonged remissions with therapy are common
Treatment
Surgical approaches
Rare patients with solitary lesion have undergone excision with no new lesions during follow-up
Drugs
Many patients have received conventional chemotherapy
Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP)
May be combined with alemtuzumab (anti-CD52)
Recent trend is toward using single immunosuppressive agents, at least initially
Corticosteroids, cyclosporine, chlorambucil
Long-term complete remission has been reported in subset of patients
Multi-agent chemotherapy reserved for patients with progressive disease
Radiation
May have role in localized disease
Can lead to long-term remissions
May have role in palliation
Stem cell transplantation appears to have role in patients with primary refractory, recurrent, or disseminated disease
Complete remission rate reported in subset of patients
Did these patients truly have SPTCL or primary cutaneous γ/δ T-cell lymphoma?
Reevaluation of earlier published case series is needed, as disease was redefined in WHO 2008 classification
Prognosis
Clinically indolent disease
˜ 80% 5-year overall survival (OS)
> 90% in patients who never develop HPS
Prolonged remission with therapy
Dissemination is rare
IMAGE FINDINGS
Ultrasonographic Findings
Diffuse, hyperechoic areas with linear vascular markings
CT Findings
Enhancing nodules with infiltrative pattern in subcutaneous tissue
F18 FDG PET Scan
SPTCL can be moderately avid
MICROSCOPIC PATHOLOGY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree