Patient Story
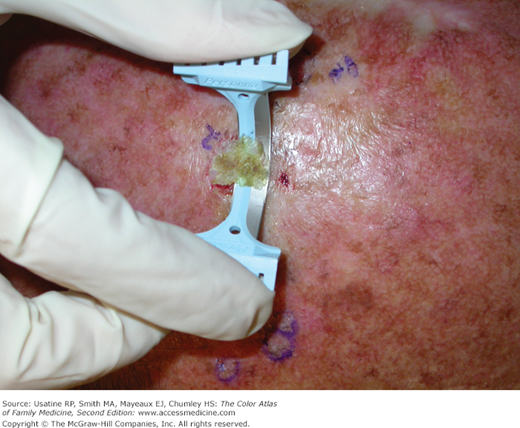
A 66-year-old farmer presents with new growths on his scalp (Figure 171-1). The patient admits to lots of sun exposure and has already had one squamous cell carcinoma (SCC) excised from the scalp 5 years ago. On close inspection there are many suspicious areas for SCC (Figure 171-1). Figure 171-2 demonstrates a shave biopsy of a SCC on a scalp using a dermablade. The pathology demonstrated that 2 of 3 biopsy sites were positive for SCC (E and G were SCC and F was read as actinic keratoses). The patient was referred for Mohs surgery. The Mohs surgeon recommended field treatment with 5-fluoruracil for 4 weeks before surgery to minimize the amount of cutting that would be needed to clear the SCC from this diffusely sun-damaged scalp.
Figure 171-1
Multiple squamous cell carcinomas on the scalp of a farmer with a lot of sun exposure. The pathology demonstrated that 2 of 3 biopsy sites were positive for squamous cell carcinoma (E and G were squamous cell carcinomas and F was read as actinic keratosis). (Courtesy of Richard P. Usatine, MD.)
Introduction
Epidemiology
- Mortality from SCC has been observed as 0.29 per 100,000 population.1
- Metastasis from SCC occurs in 2% to 9.9% of cases.2
- The incidence is increasing in all age groups and populations at a rate of 3% to 10%.2
- In the United States, approximately 2500 people die from SCC every year.3
- SCC is the second most common skin cancer and accounts for up to 25% of nonmelanoma skin cancers.4
- More than 250,000 new cases of invasive SCC are diagnosed annually in the United States.4
Pathophysiology
SCC is a malignant tumor of keratinocytes. Most SCCs arise from precursor lesions called actinic keratoses. SCCs usually spread by local extension but are capable of regional lymph node metastasis and distant metastasis. Human papillomavirus (HPV)-related lesions may be found on the penis, labia, and perianal mucosa, or in the periungual region or elsewhere associated with immunosuppression.5
Risk Factors
- Long-term cumulative UV exposure is the greatest risk factor.
- Childhood sunburns.
- Occupational exposure.
- Other UV exposure including PUVA therapy and tanning beds.
- Smoking.
- HPV exposure.
- Exposure to ionizing radiation.
- Arsenic exposure.
- Fair skin.
- Age older than 60 years.
- Male gender.
- Living at lower latitude and higher altitude.
- Nonhealing ulcers.
- Chronic or severe immunosuppression, including posttransplant immunosuppression, HIV, and long-term steroid use.
- Genetic syndromes, including Muir Torre, xeroderma pigmentosum, dystrophic epidermolysis bullosa, epidermodysplasia verruciformis, and oculocutaneous albinism.4
Diagnosis
- The only sure method of making the diagnosis is a biopsy. Biopsy suspicious lesions (thickened, tender, indurated, ulcerated, or crusting) especially in sun-exposed areas.
SCC often presents as areas of persistent ulceration, crusting, hyperkeratosis, and erythema, especially on sun-damaged skin.
Less common types of SCC:
- Marjolin ulcer—SCC of the extremities found in chronic skin ulcers or burn scars. This is a more common risk in darker pigmented individuals (Figure 171-3).
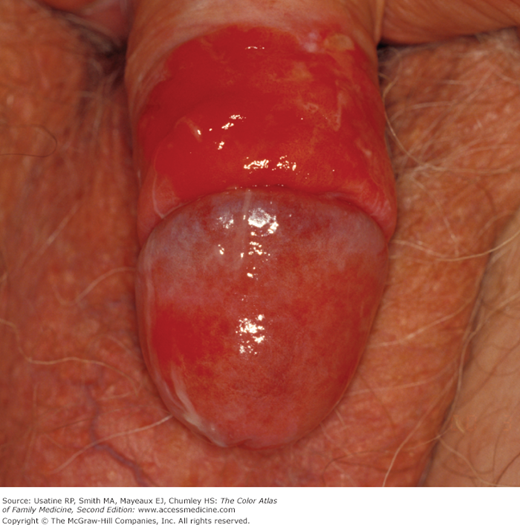
- Erythroplasia of Queyrat—SCC in situ on the penis or vulva related to HPV infection (Figure 171-4). This can progress to invasive SCC of the penis (Figure 171-5).
SCC is found in all sun-exposed areas and on mucus membranes. The most common sites are:
- Face (Figures 171-6 and 171-7).
- Lower lip (Figures 171-8 and 171-9).
- Ears (Figure 171-10).
- Scalp (Figures 171-1 and 171-11).
- Extremities—arm—(Figures 171-12 and 171-13).
- Hands (Figure 171-14).
- Fingers (Figure 171-15).
- Mucus membranes (Figure 171-16) (see Chapter 43, Oral Cancer).
Figure 171-7
A. Large cystic appearing squamous cell carcinoma on the face. Although this could have been a basal cell carcinoma, it definitely required a biopsy and excision. B. Small subtle invasive squamous cell carcinoma on the face that could have been overlooked or treated as an actinic keratosis. Any scaling lesion on the face that persists should be biopsied. (Courtesy of Richard P. Usatine, MD.)