Splenic Marginal Zone Lymphoma
Roberto N. Miranda, MD
Key Facts
Terminology
Splenic marginal zone lymphoma (SMZL), splenic B-cell marginal zone lymphoma (2008 WHO), splenic lymphoma with circulating villous lymphocytes (SLVL)
Clinical Issues
Splenomegaly & enlarged splenic hilar lymph nodes
Bone marrow involvement is very common
Peripheral blood lymphocytosis (so-called villous lymphocytes) in subset of patients
Clinical course is indolent; HCV(+) patients may respond to interferon-γ or ribavirin
Microscopic Pathology
Small lymphocytes replace white pulp and infiltrate red pulp
Ancillary Tests
Positive for B-cell markers: CD19, CD20, CD22, CD79a, and monotypic surface Ig light chain
Top Differential Diagnoses
Chronic lymphocytic leukemia/small lymphocytic lymphoma
Follicular lymphoma
Mantle cell lymphoma
Hairy cell leukemia
Diagnostic Checklist
Expanded white pulp by lymphoma with lesser red pulp infiltration
TERMINOLOGY
Abbreviations
Splenic marginal zone lymphoma (SMZL)
Synonyms
Splenic B-cell marginal zone lymphoma, splenic lymphoma with circulating villous lymphocytes (SLVL)
Definitions
B-cell neoplasm composed of small lymphocytes
Neoplastic lymphocytes replace white pulp germinal centers and mantle zones, merge with peripheral (marginal) zone of larger cells, and infiltrate red pulp
Splenic hilar lymph nodes and bone marrow often involved; leukemic involvement can occur (SLVL)
ETIOLOGY/PATHOGENESIS
Postulated Normal Counterpart
B cell of unknown differentiation stage
In approximately 50% of cases, precursor cells have differentiation stage compatible with antigen exposure
CLINICAL ISSUES
Epidemiology
Incidence
< 2% of lymphoid neoplasms
Age
Most patients over 50 years old
Gender
No sex predilection
Presentation
Splenomegaly
Enlarged splenic hilar lymph nodes but not usually peripheral lymph nodes
Bone marrow involvement
Peripheral blood lymphocytosis (so-called villous lymphocytes) in subset of patients; total white blood cell count can be high
Occasional autoimmune thrombocytopenia or anemia
Monoclonal serum protein in 1/3 of patients
Hyperviscosity and hypergammaglobulinemia are rare
Association with hepatitis C infection in 20% of cases in Southern Europe
Treatment
Response to chemotherapy used for chronic lymphocytic leukemia is often suboptimal
Splenectomy results in hematologic response and long-term survival
Patients with concomitant HCV(+) may respond to interferon-γ or ribavirin
Prognosis
Clinical course is indolent
Transformation to large cell lymphoma may occur in about 10% of cases
Adverse clinical prognostic factors include large tumor mass or poor general health status
P53 mutations, 7q deletion, and unmutated IgH variable region genes may show unfavorable outcome
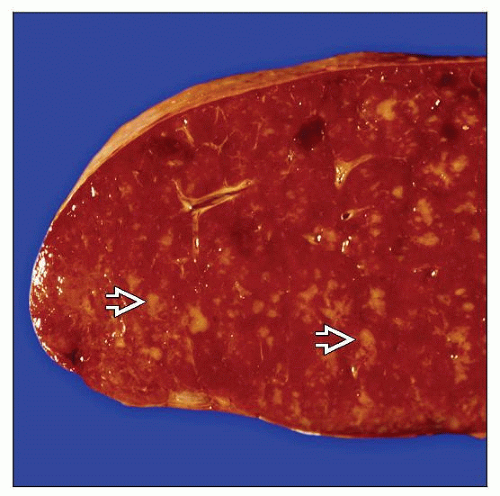
MACROSCOPIC FEATURES
General Features
Micronodular miliary-like pattern of white pulp upon serial sections
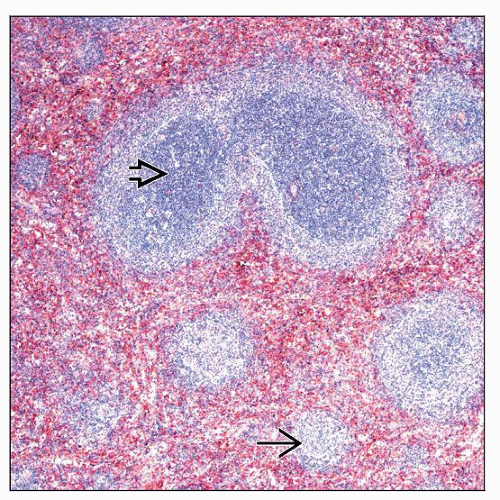
MICROSCOPIC PATHOLOGY
Histologic Features
Low-power magnification shows dark inner zone surrounded by light outer marginal zone (“biphasic pattern”)
Both components are considered part of neoplastic process
Germinal centers and mantle zones are usually effaced
Small lymphocytes replace white pulp and infiltrate red pulp
Predominance of small, round to slightly irregular lymphocytes with minimal cytoplasm
Mixture of small, medium, and larger lymphocytes with relatively abundant pale cytoplasm in peripheral (marginal) zones that merge with red pulp
Scattered large centroblasts are present
Mitotic figures are usually rare
Plasmacytoid differentiation is common in subset of cells and can be marked in some cases
Cords and sinuses of red pulp contain small aggregates of neoplastic cells; these can be associated with epithelioid histiocytes
Splenic hilar lymph nodes are typically partially replaced by SMZL and show dilated sinuses
Peripheral blood lymphocytes are small and often characterized by unipolar cytoplasmic projections (villous lymphocytes)
Bone marrow involvement can have nodular, paratrabecular, diffuse, or mixed pattern and has a sinusoidal component in a subset of cases
Immunohistochemistry of bone marrow commonly shows follicular dendritic cells (e.g., CD21[+], CD23[+]) within aggregates
Predominant Pattern/Injury Type
Lymphoid, marginal zone
Predominant Cell/Compartment Type
Hematopoietic, lymphoid
ANCILLARY TESTS
Immunohistochemistry
B-cell neoplasm positive for pan-B-cell antigens (CD20, CD79a, pax-5) and negative for pan-T-cell antigens
CD72 is positive in ˜ 75% of cases; similar to hairy cell leukemia (HCL)
Negative for cyclin-D1, CD10, Bcl-6, and annexin-A1; usually negative for CD5 and CD23
Flow Cytometry
Positive for monotypic surface immunoglobulin light chain, CD19, CD20, CD22, and CD79b
Positive for IgM and usually positive for IgD
Negative for CD10, CD43, and usually CD103
Neoplastic cells can dimly express CD5 or CD23 in ˜ 20% of cases
Cytogenetics
Allelic loss of 7q31-32 in 40% of cases
Specific chromosomal translocations (including those identified in MALT lymphoma) have not been consistently identified in SMZL
Chromosomal translocations involving the CDK6 gene at 7q21 have been identified
Gene expression profiling studies have suggested activation of AKT1 and B-cell receptor signaling pathways
PCR
Immunoglobulin heavy and light chain genes are clonally rearranged
1/2 of cases show somatic hypermutation of immunoglobulin genes; no relationship to prognosis
DIFFERENTIAL DIAGNOSIS
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (CLL/SLL)
Expansion of white pulp forming uniform nodules without marginal zone; extensive involvement of red pulp
Lymphocytes are round to oval with clumped chromatin and scant cytoplasm
Proliferation centers are unusual in spleen (compared with lymph nodes) but are helpful when identified
Lymphocytes are positive for CD5 and CD23 by immunohistochemistry or flow cytometry immunophenotyping
In bone marrow, paratrabecular pattern is rare in CLL/SLL; in blood, CLL/SLL cells do not have villous features
Follicular Lymphoma (FL)
Miliary pattern growing along preexisting follicles
Follicles can enlarge and coalesce to form large, grossly visible masses
Neoplastic lymphocytes are centrocytes and centroblasts
Neoplastic follicles similar to nodal follicular lymphoma; may have marginal zone appearance at periphery of nodules
Neoplastic lymphocytes are positive for CD10 and Bcl-6 by immunohistochemistry &/or flow cytometry immunophenotyping
In bone marrow, paratrabecular pattern is very common and a sinusoidal pattern is rare in FL
In peripheral blood, lymphocytes are cleaved with minimal cytoplasm
Hairy Cell Leukemia (HCL)
Patients present with splenomegaly and usually pancytopenia; monocytopenia is very common
Red pulp involvement with effacement of nodularity of white pulp
Red cell “lakes” and “pseudosinuses” represent areas of disruption of sheets of tumor cells
Indented nuclei with abundant clear cytoplasm
Lymphocytes are positive for CD11c (bright), CD22 (bright), CD25, CD103, and FMC7 by flow cytometry
Lymphocytes are positive for annexin-A1 by immunohistochemistry (but must be distinguished from granulocytes that are also positive)
Immunohistochemistry for tartrate-resistant acid phosphatase and CD72 supports diagnosis of HCL in absence of cell suspensions for flow cytometry immunophenotype
Currently rare to obtain spleen specimens with HCL because diagnosis can be made confidently based on peripheral blood, bone marrow, and immunophenotypic features
Hairy Cell Leukemia Variant (HCL-v)
Resembles HCL morphologically, but patients often have lymphocytosis and circulating monocytes; neoplastic lymphocytes often have small nucleolus
Negative for CD25 and annexin-A1; positive for CD103 in ˜ 70% of cases
Lymphoplasmacytic Lymphoma (LPL)
SMZL can be difficult to distinguish from LPL in patients with serum paraprotein and bone marrow involvement; usually spleen in LPL patients is not very large
Periarteriolar aggregates of small lymphocytes, plasmacytoid lymphocytes, plasma cells
Absence of marginal zone differentiation
del 6q favors LPL; del 7q and gains of 3q favor SMZL
Mantle Cell Lymphoma (MCL)
Splenic involvement by MCL is usually associated with splenomegaly
Enlarged white pulp nodules with frequent coalescence of nodules; residual germinal centers are occasionally detected
Lymphocytes are intermediate in size with irregular nuclear contours
Red pulp involvement shows small nodules or aggregates
Touch imprints or peripheral blood may show nucleolated lymphocytes
Lymphocytes are positive for CD5 and negative for CD23 by flow cytometry or immunohistochemistry
Translocation t(11;14) by classical cytogenetics, FISH, or RT-PCR
Cyclin-D1 positive by immunohistochemistry
Marginal Zone Lymphoma, Extranodal (MALT) or Nodal
Splenomegaly and lymphocytosis are usually not features of patients with MALT lymphoma
By definition, splenic involvement excludes diagnosis of nodal marginal zone lymphoma
Monocytoid cells surrounding germinal centers rarely occur in SMZL
Splenic Follicular or Marginal Zone Hyperplasia (SMZH)
Usually associated with autoimmune processes or idiopathic thrombocytopenic purpura
Spleen may be normal size but can also weigh up to 1,000 g
White pulp displays distinct germinal centers, mantle zones, and marginal zones (‘triphasic” pattern as compared with “biphasic” pattern of SMZL)
Red pulp is well preserved with only rare lymphocytes in sinuses or in splenic cords
Immunohistochemistry does not reveal abnormal distribution of Bcl-6 or CD10(+) lymphocytes, nor disruption of germinal centers by infiltrating marginal zone lymphocytes
Flow cytometry does not reveal evidence of immunoglobulin light chain restriction or aberrant B-cell immunophenotype
Splenic Diffuse Red Pulp Small B-cell Lymphoma
Spleen cut surface is homogeneously brown-red, without miliary-like nodularity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree