Chapter 37 Speech–language pathology students
learning clinical reasoning
INTRODUCTION
In our chapter published in the previous edition of this book (McAllister & Rose 2000) we wrote:
Since we wrote that chapter, a paradox has emerged. Some discussions of applications of other professions’ models of clinical reasoning to speech-language pathology (SLP) models are appearing (McAllister & Lincoln 2004, Young 2001). However, there continues to be no substantial published research into the clinical reasoning practices of our profession. A 2005 search for references to research into clinical reasoning in SLP in academic databases and recent prominent texts on assessment and management of communication and swallowing disorders revealed minimal results. However, references to clinical reasoning are now quite common on university websites that describe their curricula, in professional association publications detailing professional competencies, and in texts describing clinically-related activities. Thus, while the profession appears to have become alerted to and interested in clinical reasoning as a necessary component of clinical practice, and is now using the term ‘clinical reasoning’ with greater frequency, it is used on the basis of a paucity of data about the actual clinical reasoning practices taking place in SLP.
SEEKING CLINICAL REASONING IN SLP
In this chapter we make a distinction between clinical decision making (a term more common in SLP) and clinical reasoning. We see clinical decision making as an end-product of clinical reasoning; that is, as the generation of tangible decisions about clinical management. In contrast we see clinical reasoning as the often intangible, rarely explicated thought processes that lead to the clinical decisions we make. We suggest that clinical reasoning utilizes metaprocesses, including an awareness or a becoming conscious of what we are thinking and what thought processes we are using. Reflection in and on action (Schön 1987) has a major role to play in clinical reasoning.
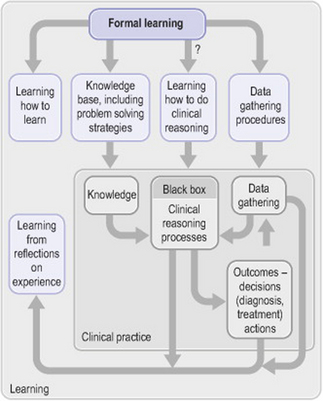
Based on our critical reading of the literature, we could describe the process of clinical reasoning in SLP as the ‘black box’ of information processing occurring between the input phase of data gathering and the output phase of producing decisions (concerning diagnosis and treatment) and taking action (Fig. 37.1). The reasons for this ‘black box’ state of affairs lie in the history and operation of our profession wherein clinical reasoning, being (broadly) the thinking associated with clinical practice, was assumed to be a skill that could be absorbed without explication. Kamhi (1998, p. 102), for instance, argued that ‘as clinicians become more experienced, they gradually internalise the framework of an assessment protocol and become proficient at analysing and interpreting test information and observational data’. The SLP profession seems to have adopted what Boshuizen & Schmidt (2000) referred to as a content-oriented approach to clinical reasoning. This approach assumes that knowledge and reasoning are interdependent. There is an expectation that with increasing knowledge and clinical experience, students and clinicians will be better able to reason and make clinical decisions. University curricula have concentrated more on knowledge acquisition and skills development while ‘issues specific to the decision-making process are relegated to the periphery of discussion’ (Records et al 1994, p. 74).
Another focus of our profession has been on outcomes and solving problems in clinical practice. Consider recent sources in the SLP literature: for example, Dodd’s 1995 text Differential Diagnosis and Treatment of Children with Speech Disorder contains a chapter on a problem-solving approach to clinical management. This problem-solving model begins at the stage of description of the current communication status (after diagnosis). Although it is an excellent model for problem solving in client management, it offers no clues to the clinical reasoning which lies behind the clinical problem solving. The Pocket Reference of Diagnosis and Management for the Speech-Language Pathologist (White 2000) contains a wealth of useful information to assist in clinical problem solving or decision making. It does not consider the clinical reasoning thinking processes underpinning diagnosis and management.
Another factor limiting understanding of clinical reasoning in SLP is that it has been seen as a linear or logical process, which obscures the ‘messiness’ and complexity of clinical reasoning in action. Duffy (1998, p. 96) suggested that the processes of decision making ‘became obscured with training that views diagnosis as a linear, test-oriented, and mechanistic process, and that often “teaches” diagnosis by starting with the target disorder (the diagnosis) and then proceeding back to its defining symptoms and signs’. Yoder & Kent (1988) published an influential series of decision-making trees for the diagnosis and management of communication disorders. They stated that the trees were not to be seen as recipes, but rather as a series of guidelines and prompts for the clinician engaged in decision making. ‘Cookbooks cannot deal with the unknown or the uncertain, but clinical decision making frequently encounters them’ (Yoder & Kent 1988, p. xi). This approach has the advantage of providing guidance without rigidity and recognizing the need for professional judgement as part of decision making. However, the focus is again on the decision steps to be taken rather than on the nature of thinking in which clinicians engage and how they might respond to the prompts provided. The approach reinforces the view that clinical reasoning and decision making are basically linear and logical, whereas we argue that they are not. Further, the responsibility for learning how to think lies with the clinician. It is not made explicit.
EMERGING DIRECTIONS AND CHALLENGES IN SLP CLINICAL REASONING
In their edited text Differential Diagnosis in Speech-Language Pathology, Philips & Ruscello (1998) provided a broader picture of the process of diagnosis. Although they referred readers to decision-making trees they moved beyond a formulaic data collection approach to an acknowledgment that ‘the speech-language pathologist’s curiosity and inquisitiveness drive the process of differential diagnosis. The clinician who accepts diagnostic challenges, is curious about missing information and inconsistencies, constantly questions, and searches for possible answers is most likely to solve puzzles presented by difficult problems’ (Philips & Ruscello 1998, p. 3). It is argued here that clinicians need to be aware of missing information and inconsistencies and to be thinking about them, questioning self, the process and the data. In other words, clinicians need to be engaged in metacognition, or thinking about thinking, a key component in the Higgs & Jones (2000) model of clinical reasoning. Kamhi (1998) and Deputy & Weston (1998) have reminded readers of the importance of asking causal questions but cautioned them about assuming linear causality. Asking questions about factors that may or may not cause communication disorders and that contribute to the data obtained in evaluation is an important component of what we would call clinical reasoning.
Records et al (1994) discussed clinical judgment. They emphasized not only the objective aspects of data collection, but also the subjective aspects of the decision-making process; the gut feelings, expertise and insights which are aspects of clinical reasoning. They considered clinical judgment to be a process poorly understood by speech-language pathologists. Scholten (2001) argued that both classroom and clinical experiences can be used to facilitate student clinical reasoning. She suggested that teachers should use authentic problems to develop students’ understanding of clinical problems and transfer of theoretical knowledge. However, again, such assertions were based on theory from medical education and student learning in general rather than specific evidence in speech language-pathology.
HOW DO SPEECH-LANGUAGE PATHOLOGISTS REASON?
In the relative absence of direct clinical reasoning research, writers in our discipline have resorted to supposition or analogy, drawing on research in other professions. Campbell (1998) outlined four approaches to diagnostic decision making found in clinical medicine that also apply to SLP: pattern recognition, decision-making trees, diagnosis by exhaustion (collecting all possible data), and hypothetical-deductive reasoning. Duffy (1998, p. 97) stated that ‘most good diagnosticians reach conclusions through a hypothetical-deductive strategy, with frequent reliance on pattern recognition’. The paucity of research into decision making and clinical reasoning in SLP does not provide data to test Campbell’s or Duffy’s assumptions. However, in their reflection on comparisons with reasoning approaches in other disciplines, Campbell and Duffy began to question possible reasoning strategies in SLP.
A promising discussion in our field comes from Hagstrom (2001) who presented a potential framework for using and building theory in clinical action in SLP. Hagstrom wrote about clinical action being guided by theory and proposed Bamberg’s (1997) six-element framework of theory analysis as a tool for reflection on practice. Table 37.1 illustrates the six aspects of Bamberg’s framework, with typical clinical questions that could be asked in SLP practice. Although Hagstrom did not directly discuss clinical reasoning and made no reference to research examining reasoning in other professions, it appears to us that there is a direct connection between her arguments and our discussion of clinical reasoning practices.
Table 37.1 Bamberg’s aspects of theorizing in action and their potential applications to speech-language pathology
| Aspect | Typical speech-language pathology clinical questions |
|---|---|
| Domain of inquiry | What knowledge base(s) could/should I be drawing on in working with this client/situation? |
| Person | Am I working with a client actively engaged in his/her care, or a passive client? |
| Course of development | Is change for this client/situation likely to happen step by step or can steps be merged or skipped? |
| Telos | What is the ideological endpoint for me and for my client in this situation? |
| Mechanism | What is likely to cause change to happen in this client/situation? |
| Methodology | What type of data should be collected? How will they be collected and documented? |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree