Sexual Disorders
INTRODUCTION
Sexuality is an integral human function that’s inevitably affected by many interrelated factors. Its expression reflects the interaction of the biological, psychological, and sociologic ingredients that affect a person’s self-image and behavior.
Depending on these complex factors, human sexuality can be healthy and enriching, or it can be the source of mental and physical distress. A sexually healthy person is commonly defined as a person who:
exhibits behavior that agrees with gender identity (persistent feeling of oneself as male or female)
can participate in a potentially loving or committed relationship
finds erotic stimulation pleasurable
can make decisions about sexual behavior that are compatible with values and beliefs
HAZARDS TO SEXUAL HEALTH
An important group of sex-related disorders results from infection that’s transmitted through sexual contact. These disorders include human immunodeficiency virus infection, gonorrhea, syphilis, chlamydial infections, genital herpes, genital warts, trichomoniasis, chancroid, and lymphogranuloma venereum. Sexually transmitted diseases (STDs) are among the most prevalent infections around the world; gonorrhea, chlamydial infections, and genital warts are approaching epidemic proportions in the United States.
Sexual dysfunction disorders, including arousal disorders, orgasmic disorders, erectile dysfunction, and sexual pain disorders (dyspareunia and vaginismus), may be caused by a general medical condition, psychological factors, or a combination of factors, or they may be substance-induced. Other disorders have a definite physical etiology.
Gender identity disorders and paraphilias are sexual disorders whose diagnostic criteria are found in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision.
PHYSICAL ASSESSMENT
Physical assessment, primarily a diagnostic tool, can also serve as an excellent opportunity for patient teaching.
During examination of the female, evaluate breast development, pubic hair distribution, and the development of external genitalia. With gloved hands, use a speculum to examine internal genitalia, including the cervix and vagina. Palpate the uterus and ovaries.
Take special care when examining an older woman because atrophic changes of the vaginal mucosa may increase her discomfort during a pelvic examination. Use a small speculum because of the decreased vaginal size. To ease insertion, dampen the speculum with warm water; don’t use a lubricant because it may alter Papanicolaou test results. Proceed slowly; abrupt insertion of the speculum may damage sensitive degenerating tissue.
During examination of the male, check pubic and axillary hair distribution. With a gloved hand, palpate the penis, scrotum, prostate gland, and rectum. Inspect the penis (shaft, glans, and urethral meatus) for lesions, swell ing, inflammation, scars, or discharge. In the uncircumcised male, retract the foreskin to visualize the glans. Examine the scrotum for size, shape, and abnormalities, such as nodules or inflammation. Check for the presence of both testes (the left testis is typically lower than the right) and testicular volume.
The testes of an older male may be slightly smaller than those of a younger male, but they should be equal in size, smooth, freely moveable, and soft without nodules.
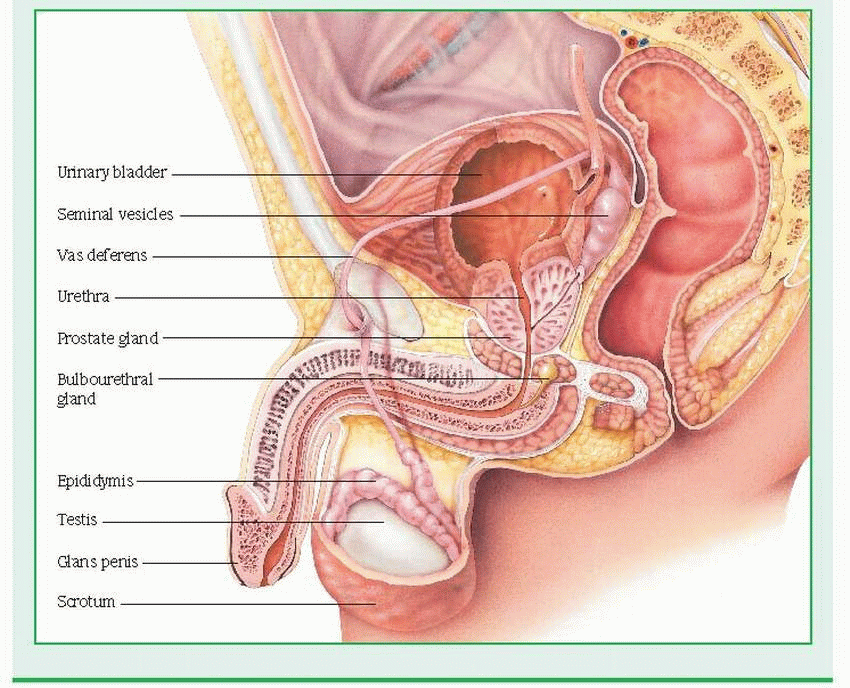
Inspect and palpate the inguinal canal; you shouldn’t observe any bulging of tissues or or gans. (See Male sexual anatomy.)
SEXUAL HISTORY
Careful assessment helps identify the cause of a sexual problem as psychological or physical. A sexual history provides the basis for prevention, diagnosis, and treatment.
Ensure privacy, as for physical assessment. Allow sufficient time so that the patient doesn’t feel rushed.
Approach a sexual history objectively. Remember, sexual health is relative; avoid making assumptions or judgments about the patient’s sexual activities.
After listening to the patient, determine his level of sexual understanding and phrase your questions in language that he can understand. Avoid technical terms.
Begin with the least threatening questions. Usually, a menstrual or urologic history helps lead into a sexual history.
Inquire about what the patient accepts as normal sexual behavior. Ask about sexual needs and priorities and whether the patient can discuss them with a sex partner.
Male sexual anatomy
The scrotum, which contains the testes, epididymis, and lower spermatic cords, maintains the proper testicular temperature for spermatogenesis through relaxation and contraction. The penis consists of three cylinders of erectile tissue: two corpora cavernosa and the corpus spongiosum, which contains the urethra.
The testes (gonads, testicles) produce sperm in the seminiferous tubules, with complete spermatogenesis developing in most males by age 15 or 16. In the fetus, the testes form in the abdominal cavity and descend into the scrotum during the seventh month of gestation. The testes also secrete testosterone in the interstitial cells (Leydig’s cells). Testosterone affects the development and maintenance of secondary sex characteristics and sex drive. It also regulates metabolism, stimulates protein anabolism (encouraging skeletal growth and muscular development), inhibits pituitary secretion of the gonadotropins (follicle-stimulating hormone and interstitial cell-stimulating hormone), promotes potassium excretion, and mildly influences renal sodium reabsorption.
The vas deferens connects the epididymis, in which sperm develop, mature, and are stored for 5 to 7 days, and the ejaculatory ducts. (Vasectomy achieves sterilization by severing and interrupting the vas deferens, as both ends are tied off.) The seminal vesicles, two convoluted membranous pouches, secrete a viscous liquid of fructose-rich semen and prostaglandins that facilitates fertilization. The prostate gland secretes the thin alkaline substance that comprises most of the seminal fluid; this fluid also protects sperm from acidity in the male urethra and in the vagina, increasing sperm motility.
The bulbourethral (Cowper’s) glands secrete an alkaline pre-ejaculatory fluid, probably similar in function to that produced by the prostate gland. The spermatic cords are cylindrical fibrous coverings in the inguinal canal, containing the vas deferens, blood vessels, and nerves.
 |
Assess risk behavior concerning selection of sex partners and specific sexual practices.
Ask about possible homosexual activity, which can influence the risk and treatment of some STDs.
Ask the female patient if she has adequate lubrication during intercourse and if she has ever experienced orgasm or pain with sexual contact. Ask the male patient if he has ever had difficulties with erection or ejaculation.
Ask about current or past contraceptive practices.
Try to use the history therapeutically by encouraging the patient to express anxiety. Such fears may be alleviated simply by providing factual information and answering questions.
TYPES OF SEX THERAPY
Sex therapy can be a vital therapeutic tool for treating sexual dysfunction. Before therapy begins, a history, a physical examination, and appropriate treatment must rule out organic causes of sexual dysfunction. The major forms of sex therapy include psychoanalysis, behavioral therapy, group therapy, classic (Masters and Johnson) therapy, and Kaplan’s sex therapy. The type of therapy appropriate for the patient depends on his problems, needs, and finances.
SEXUALLY TRANSMITTED DISEASES
Gonorrhea
A common sexually transmitted disease, gonorrhea is an infection of the genitourinary tract (especially the urethra and cervix) and, occasionally, the rectum, pharynx, and eyes. Untreated gonorrhea can spread through the blood to the joints, tendons, meninges, and endocardium; in females, it can also lead to chronic pelvic inflammatory disease (PID) and sterility. After adequate treatment, the prognosis for both males and females is excellent, although reinfection is common. Gonorrhea is especially prevalent among young people and people with multiple partners, particularly those between ages 15 and 29. In these patients, suspect concomitant chlamydia infection.
CAUSES AND INCIDENCE
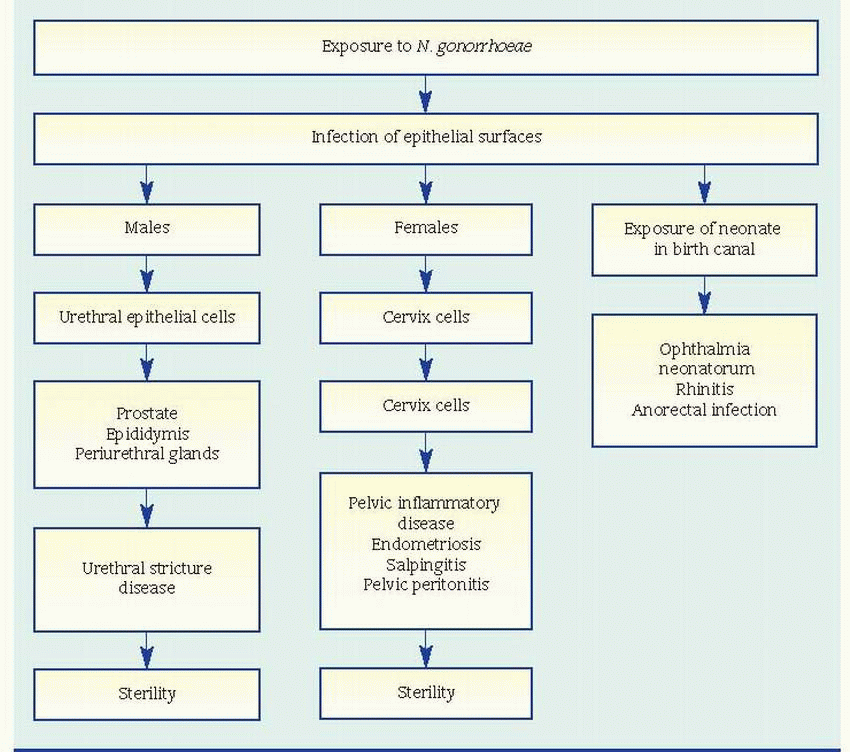
Transmission of Neisseria gonorrhoeae, the organism that causes gonorrhea, usually follows sexual contact with an infected person. Children born of infected mothers can contract gonococcal ophthalmia neonatorum during passage through the birth canal. Children and adults with gonorrhea can contract gonococcal conjunctivitis by touching their eyes with contaminated hands.
The Centers for Disease Control and Prevention estimates that there are about 700,000 new cases of gonorrhea each year; only about half of these cases are reported to health care officials.
COMPLICATIONS
Conjunctivitis
Dermatitis
Epididymitis
Perihepatitis
Proctitis
Salpingitis
Septic arthritis
SIGNS AND SYMPTOMS
Although many infected males may be asymptomatic, after a 3- to 6-day incubation period, some develop symptoms of urethritis, including dysuria and purulent urethral discharge, with redness and swelling at the infection site. Most infected females remain asymptomatic but may develop inflammation and a greenish yellow discharge from the cervix—the most common gonorrheal symptoms in females. (See What happens in gonorrhea.)
Other clinical features vary according to the site involved:
urethra: dysuria, urinary frequency and incontinence, purulent discharge, itching, and red and edematous meatus
vulva: occasional itching, burning, and pain due to exudate from an adjacent infected area (symptoms tend to be more severe before puberty or after menopause)
vagina (most common site in children older than age 1): engorgement, redness, swelling, and profuse purulent discharge
liver: right upper quadrant pain in a patient with perihepatitis
pelvis: severe pelvic and lower abdominal pain, muscle rigidity, tenderness, and abdominal distention. As the infection spreads, nausea, vomiting, fever, and tachycardia may develop in a patient with salpingitis or PID
Other possible symptoms include pharyngitis, tonsillitis, rectal burning and itching, and bloody mucopurulent discharge.
Gonococcal septicemia is more common in females than in males. Its characteristic signs
include tender papillary skin lesions on the hands and feet; these lesions may be pustular, hemorrhagic, or necrotic. Gonococcal septicemia may also produce migratory polyarthralgia and polyarthritis and tenosynovitis of the wrists, fingers, knees, or ankles. Untreated septic arthritis leads to progressive joint destruction.
include tender papillary skin lesions on the hands and feet; these lesions may be pustular, hemorrhagic, or necrotic. Gonococcal septicemia may also produce migratory polyarthralgia and polyarthritis and tenosynovitis of the wrists, fingers, knees, or ankles. Untreated septic arthritis leads to progressive joint destruction.
Signs of gonococcal ophthalmia neonatorum include lid edema, bilateral conjunctival infection, and abundant purulent discharge 2 to 3 days after birth. Adult conjunctivitis, most common in men, causes unilateral conjunctival redness and swelling. Untreated gonococcal conjunctivitis can progress to corneal ulceration and blindness.
DIAGNOSIS
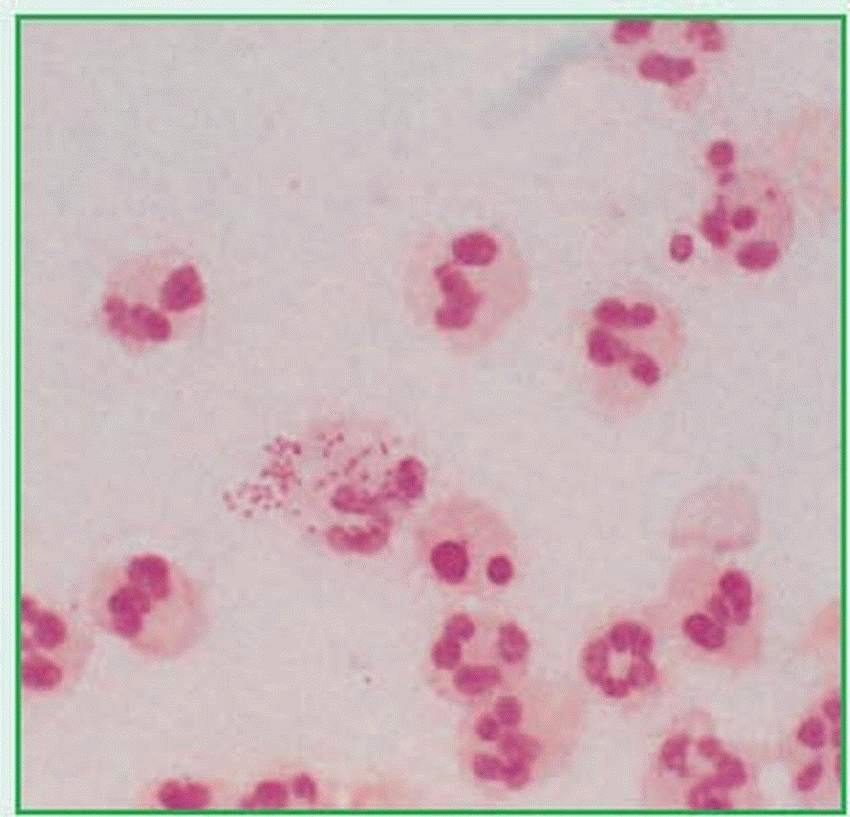
A culture from the infection site (urethra, cervix, rectum, or pharynx), grown on a Thayer-Martin or Transgrow medium, usually establishes the diagnosis by isolating N. gonorrhoeae. (See Neisseria gonorrhoeae, page 1088.) A Gram stain showing gram-negative diplococci supports the diagnosis and may be sufficient to confirm gonorrhea in males.
Ligase chain reaction is an assay that can detect N. gonorrhoeae and Chlamydia trachomatis from urethral or cervical swabs. It allows for rapid diagnosis and offers improved sensitivity and specificity compared to swab specimen cultures.
Confirmation of gonococcal arthritis requires identification of gram-negative diplococci on smears made from joint fluid and skin lesions. Complement fixation and immunofluorescent assays of serum reveal antibody titers four times the normal rate. Culture of conjunctival scrapings confirms gonococcal conjunctivitis.
TREATMENT
For adults and adolescents, the recommended treatment for uncomplicated gonorrhea caused by susceptible non-penicillinase-producing N. gonorrhoeae is a single dose of ceftriaxone or cefixime; for presumptive treatment of concurrent C. trachomatis infection, doxycycline. Gonorrhea may also be treated with a single dose of azithromycin. Common alternative prescriptions may include cefuroxime, cefpodoxime proxetil, or erythromycin. A follow-up visit 7 days after treatment to recheck cultures and confirm the cure of infection is recommended, especially for women who are asymptomatic or may not have symptoms associated with the infection. A single dose of ceftriaxone and erythromycin is recommended for pregnant patients and those allergic to penicillin.
Treatment of gonococcal conjunctivitis requires a single dose of ceftriaxone, and lavage of the infected eye with saline solution once.
Routine instillation of 1% silver nitrate drops or erythromycin ointment into the neonate’s eyes soon after delivery has greatly reduced the incidence of gonococcal ophthalmia neonatorum.
SPECIAL CONSIDERATIONS
Before treatment, establish whether the patient has any drug sensitivities, and watch closely for adverse drug reactions during therapy.
Warn the patient that, until cultures prove negative, he’s still infectious and can transmit gonococcal infection.
If the patient has gonococcal arthritis, apply moist heat to ease pain in affected joints.
Urge the patient to inform sexual contacts of his infection so that they can seek treatment, even if cultures are negative. Advise him to avoid sexual intercourse until treatment is complete.
Report all cases of gonorrhea to local public health authorities for follow-up on sexual contacts. Examine and test all people exposed to gonorrhea as well as children of infected mothers.
Routinely instill two drops of 1% silver nitrate solution or erythromycin ointment in the eyes of all neonates immediately after birth. Check the neonate of an infected mother for signs of infection. Take specimens for culture from the neonate’s eyes, pharynx, and rectum.
To prevent gonorrhea, tell patients to avoid anyone suspected of being infected. Tell them that abstinence is the only sure way to prevent gonorrhea. (See Preventing gonorrhea.)
Report all cases of gonorrhea in children to child abuse authorities.
Chlamydial infections
Chlamydial infections—including urethritis in men and urethritis and cervicitis in women— are a group of infections that are linked to one organism: Chlamydia trachomatis. Trachoma inclusion conjunctivitis, a chlamydial infection that seldom occurs in the United States, is a leading cause of blindness in Third World countries. Lymphogranuloma venereum, a rare disease in the United States, is also caused by C. trachomatis. (See Lymphogranuloma venereum, page 1090.)
Untreated, chlamydial infections can lead to such complications as acute epididymitis, salpingitis, pelvic inflammatory disease (PID) and, eventually, sterility. Some studies show that a chlamydial infection in a pregnant woman is associated with spontaneous abortion and premature delivery.
CAUSES AND INCIDENCE
Transmission of C. trachomatis primarily follows vaginal or rectal intercourse or orogenital
contact with an infected person. Because symptoms of chlamydial infections commonly appear late in the disease’s course, sexual transmission of the organism typically occurs unknowingly. Children born of mothers who have chlamydial infections may contract associated conjunctivitis, otitis media, and pneumonia during passage through the birth canal.
contact with an infected person. Because symptoms of chlamydial infections commonly appear late in the disease’s course, sexual transmission of the organism typically occurs unknowingly. Children born of mothers who have chlamydial infections may contract associated conjunctivitis, otitis media, and pneumonia during passage through the birth canal.
To prevent gonorrhea, teach your patient the following:
Tell the patient to avoid sexual contact until test cultures are negative and infection is gone.
Advise the partner of an infected person to be treated even if the partner doesn’t have a positive culture. Recommend that the partner avoid sexual contact with anyone until treatment is complete because reinfection is very common.
Advise the patient and all sexual partners to be tested for human immunodeficiency virus and hepatitis B infection.
Tell the patient to take anti-infective drugs for the length of time prescribed.
To prevent reinfection, tell the patient to avoid sexual contact with anyone suspected of being infected, to use condoms during intercourse, to wash genitalia with soap and water before and after intercourse, and to avoid sharing washcloths or using douches.
Advise the patient to return for follow-up testing.
Chlamydial infections are the most common sexually transmitted diseases in the United States, affecting an estimated 4 million people in the United States each year.
COMPLICATIONS
Epididymitis
Neonatal death
Pelvic inflammatory disease
Premature rupture of membranes
Preterm delivery
Salpingitis
Spontaneous abortion
Sterility
SIGNS AND SYMPTOMS
Both men and women with chlamydial infections may be asymptomatic or may show signs of infection on physical examination. Individual signs and symptoms vary with the specific type of chlamydial infection and are determined by the organism’s route of transmission to susceptible tissue.
A woman with cervicitis may develop cervical erosion, mucopurulent discharge, pelvic pain, and dyspareunia.
A woman with endometritis or salpingitis may experience signs of PID, such as pain and tenderness of the abdomen, cervix, uterus, and lymph nodes; chills; fever; breakthrough bleeding; bleeding after intercourse; and vaginal discharge. She may also have dysuria.
A woman with urethral syndrome may experience dysuria, pyuria, and urinary frequency.
A man with urethritis may experience dysuria, erythema, tenderness of the urethral meatus, urinary frequency, pruritus, and clear urethral discharge. In urethritis, such discharge may be copious and purulent or scant and clear or mucoid.
A man with epididymitis may experience painful scrotal swelling and urethral discharge.
A man with prostatitis may have lower back pain, urinary frequency, dysuria, nocturia, and painful ejaculation.
A patient with proctitis may have diarrhea, tenesmus, pruritus, bloody or mucopurulent discharge, and diffuse or discrete ulceration in the rectosigmoid colon.
DIAGNOSIS
A swab from the site of infection (urethra, cervix, or rectum) establishes a diagnosis of urethritis, cervicitis, salpingitis, endometritis, or proctitis. A culture of aspirated material establishes a diagnosis of epididymitis.
Antigen detection methods, including the enzyme-linked immunosorbent assay and the direct fluorescent antibody test, have long been used for identifying chlamydial infection. Tissue cell cultures, however, are more sensitive and specific. Newer nucleic acid probes using polymerase chain reactions are also commercially available and have become the diagnostic tests of choice.
TREATMENT
The recommended first-line treatment for adults and adolescents who have chlamydial
infections is drug therapy with tetracycline, erythromycin, or azithromycin.
infections is drug therapy with tetracycline, erythromycin, or azithromycin.
Lymphogranuloma venereum
A rare disease in the United States, lymphogranuloma venereum (LGV) is caused by serovars L1, L2, or L3 of Chlamydia trachomatis. The most common clinical manifestation of LGV among heterosexuals, especially male patients, is enlarged inguinal lymph nodes (usually unilateral). These nodes may become fluctuant, tender masses. Regional nodes draining the initial lesion may enlarge and appear as a series of bilateral buboes. Untreated buboes may rupture and form sinus tracts that discharge a thick, yellow, granular secretion.
Women and homosexually active men may have proctocolitis or inflammatory involvement of perirectal or perianal lymphatic tissues, resulting in fistulas and strictures.
By the time most patients seek treatment, the self-limited genital ulcer that sometimes occurs at the inoculation site is no longer present. The diagnosis usually is made serologically and by excluding other causes of inguinal lymphadenopathy or genital ulcers.
The treatment of choice is doxycycline. Treatment cures infection and prevents ongoing tissue damage, although the patient may develop a scar or an indurated inguinal mass. Buboes may require aspiration or incision and drainage through intact skin.
For pregnant women with chlamydial infections, erythromycin (stearate base) or azithromycin may be used.
SPECIAL CONSIDERATIONS
Practice standard precautions when caring for a patient with a chlamydial infection.
Make sure that the patient fully understands the dosage requirements of prescribed medications for this infection.
Stress the importance of completing the entire course of drug therapy even after the symptoms subside.
Teach the patient to follow meticulous personal hygiene measures as recommended.
Urge the patient to inform sexual contacts of his infection so that they can receive appropriate treatment.
If required in your state, report all cases of chlamydial infection to the appropriate local public health authorities, who will then conduct follow-up notification of the patient’s sexual contacts.
Suggest that the patient and his sex partners receive testing for the human immunodeficiency virus.
Tell the patient to return for follow-up testing.
Check the neonate of an infected mother for signs of chlamydial infection. Obtain appropriate specimens for diagnostic testing.
♦ To prevent eye contamination, tell the patient to avoid touching any discharge and to wash and dry his hands thoroughly before touching his eyes.
To prevent reinfection during treatment, urge the patient to abstain from sexual intercourse until he and his partner are free of infection.
Genital herpes
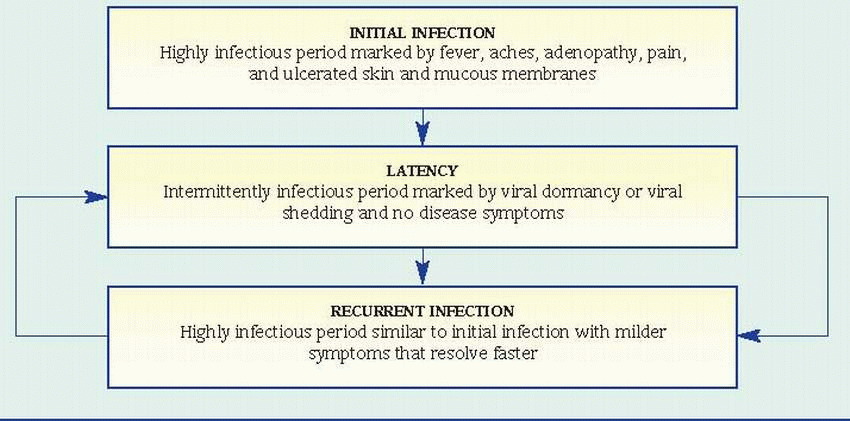
Genital herpes is an acute inflammatory disease of the genitalia. The prognosis varies, depending on the patient’s age, the strength of his immune defenses, and the infection site. Primary genital herpes is usually self-limiting but may cause painful local or systemic disease. (See Understanding the genital herpes cycle.) In neonates and patients who are immunocompromised, such as those with acquired immunodeficiency syndrome, genital herpes is usually severe, resulting in complications and a high mortality rate.
CAUSES AND INCIDENCE
Genital herpes is usually caused by infection with herpes simplex virus type 2, but some studies report increasing incidence of infection with herpes simplex virus type 1. This disease is typically transmitted through sexual intercourse, orogenital sexual activity, kissing, and hand-to-body contact. Pregnant women may transmit the infection to neonates during vaginal delivery if an active infection is present. Such transmitted infection may be localized (for instance, in the eyes) or disseminated and may be associated with central nervous system involvement.
An estimated 86 million people worldwide are thought to have genital herpes.
COMPLICATIONS
General
Increased risk of contracting other sexually transmitted diseases (STDs)
After a patient is infected with genital herpes, a latency period follows. The virus takes up permanent residence in the nerve cells surrounding the lesions, and intermittent viral shedding may take place.
Repeated outbreaks may develop at any time, again followed by a latent stage during which the lesions heal completely. Outbreaks may recur as often as three to eight times yearly.
Although the cycle continues indefinitely, some people remain symptom-free for years.
 |
During pregnancy
Neonatal brain damage
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree