3
Service and Procedural Coding: Current Procedural Terminology (CPT)
 Explain the structure, format, and conventions used in CPT (Current Procedural Terminology).
Explain the structure, format, and conventions used in CPT (Current Procedural Terminology).
 Identify CPT codes and explain their application within a medical office.
Identify CPT codes and explain their application within a medical office.
 Locate and use the appendices of CPT.
Locate and use the appendices of CPT.
 Assign correct Evaluation and Management (E&M) codes.
Assign correct Evaluation and Management (E&M) codes.
 Apply modifiers with an understanding of their importance in coding.
Apply modifiers with an understanding of their importance in coding.
 Identify services and procedures included in a surgical package.
Identify services and procedures included in a surgical package.
 Define the difference between a consult and a referral.
Define the difference between a consult and a referral.
 Identify and use the HCPCS (Healthcare Common Procedure Coding System) for Medicare claims.
Identify and use the HCPCS (Healthcare Common Procedure Coding System) for Medicare claims.
 Translate written documentation into a numerical language.
Translate written documentation into a numerical language.
 Identify and code services for entry on an insurance claim form.
Identify and code services for entry on an insurance claim form.
| Term | Definition |
| Adjunct Codes | Codes used to record additional services. |
| AMA | American Medical Association. |
| Audit | A process to determine if the information sent to the insurance company is supported by the documentation in the medical record. |
| Biopsy | Removal of a small amount of tissue to determine the extent of a disease or to determine a diagnosis. |
| Bundling Services | Combining lesser services with a major service so that one charge will include the variety of services. |
| CCI | Correct Coding Initiative: Bundling edits created by CMS to combine various component items with a major service or procedure. |
| CMS | Centers for Medicare and Medicaid Services: The federal agency responsible for maintaining and monitoring the Medicare program, beneficiary services, and Medicaid and state operations (formerly Health Care Financing Administration [HCFA] until 2001). |
| Comorbidity | An ongoing condition that exists with another condition for which the patient is receiving treatment. |
| Component Billing | Billing for each item or service provided to a patient in accordance with insurance carriers’ policies. |
| CPT | Current Procedural Terminology. Nomenclature published by the AMA as a means to describe services rendered to a patient through the use of numerical codes. |
| CPT Code | Procedural description with a five-digit identifying code number. |
| Diagnostic Services | Services performed to determine or establish a patient’s diagnosis. |
| E&M Codes | Evaluation and Management codes used to report patient visits, consults, hospital care, and so on. |
| Endoscopic Procedure | A procedure performed through an existing orifice with an endoscope to visualize an abnormality or to determine the extent of a disease. |
| Global Period | Specific time frames assigned to a code by an insurance company before additional payment will be made following a surgical procedure (e.g., 10 days, 90 days). |
| Global Procedures | Major surgical procedures that typically have a follow-up period of 30, 60, 90, or 120 days before you may begin to bill the patient for services related to the original procedure. |
| HCPCS | Healthcare Common Procedure Coding System: A coding system designed by CMS to report patient services that uses codes from CPT and other sources of alphanumeric codes. |
| HIPAA | Health Insurance Portability and Accountability Act: An act passed in 1996 to set standards for electronic health care transactions and to protect the privacy and security of patients’ health information. |
| Major Procedure | A packaged procedure that includes the operation, local infiltration, digital blocks, and follow-up care for a specific number of days. |
| Medicare Part A | A national health insurance program for persons over the age of 65 years and qualified disabled or blind persons regardless of income, administered by CMS to cover the cost of hospitalizations and nursing facility charges. |
| Medicare Part B | An elective coverage program offered by CMS for aged and disabled patients to provide benefits for physician and other medical services as part of the Medicare program. This program has a monthly premium that must be paid by the beneficiary to keep the policy in good standing. |
| Minor Procedures | Services identified by AMA as a starred procedure. For Medicare, these include services with either 0 or 10 days of follow-up care. |
| Modality | Any physical agent applied to produce therapeutic changes to biological tissues (e.g., thermal, acoustic, mechanical). |
| POS Codes | Place service (e.g., office, hospital) codes: A complete list of these codes is found in the introduction section of the professional version of the CPT manual. |
| Ranking Codes | Listing services in their order of importance by dates of service and values. Codes are usually ranked by value from highest to lowest charges. |
| RVU | Relative value unit: A method to calculate fees for services. A unit is translated into a dollar value using a conversion factor or dollar multiplier. The assigned value is generally based on three factors: physician work component, overhead practice expense, and malpractice insurance. |
| Superbill | A form designed by a medical practice listing the most frequently used diagnosis and procedure codes. |
| Therapeutic Services | Services performed for treatment of a specific condition. |
| Unbundling Services | Listing services or procedures as separate billable components. Although this practice may generate more revenue, it is often an incorrect reporting technique that could result in an insurance company auditing a practice or asking for refunds of paid monies. |
| UPIN | Unique Personal Identification Number. |
Training and Advancement
 AMA guidelines for coding applications
AMA guidelines for coding applications
 Centers for Medicare and Medicaid Services (CMS) mandates for procedural coding
Centers for Medicare and Medicaid Services (CMS) mandates for procedural coding
Certifications
The American Academy of Professional Coders grants the following certifications:
For more information contact the American Academy of Professional Coders, 309 West 700 South, Salt Lake City, UT 84101; 800-626-2633, http://www.aapc.com.
 Certified Coding Associate (CCA), intended as a starting point for a career as a coder
Certified Coding Associate (CCA), intended as a starting point for a career as a coder
 Certified Coding Specialist (CCS)
Certified Coding Specialist (CCS)
For more information contact the American Health Information Management Association (AHIMA), 919 North Michigan Avenue, Suite 1400, Chicago, IL 60611-1683; 312-787-2672, http://www.ahima.org.
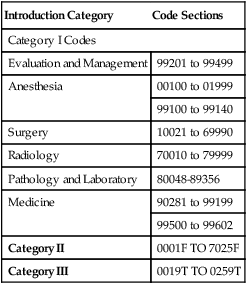
CPT Coding Sections
| Introduction Category | Code Sections |
| Category I Codes | |
| Evaluation and Management | 99201 to 99499 |
| Anesthesia | 00100 to 01999 |
| 99100 to 99140 | |
| Surgery | 10021 to 69990 |
| Radiology | 70010 to 79999 |
| Pathology and Laboratory | 80048-89356 |
| Medicine | 90281 to 99199 |
| 99500 to 99602 | |
| Category II | 0001F TO 7025F |
| Category III | 0019T TO 0259T |
CPT Coding Exercise 1
Coding Classification
Example: Code: 99242; Section: Medical section; Code range: 90281 to 99600
| CODE | SECTION | CODE RANGE |
| 1. 35501 | _______________ | _______________ |
| 2. 84234 | _______________ | _______________ |
| 3. 64575 | _______________ | _______________ |
| 4. 90802 | _______________ | _______________ |
| 5. 77305 | _______________ | _______________ |
| 6. 01400 | _______________ | _______________ |
| 7. 97750 | _______________ | _______________ |
| 8. 27370 | _______________ | _______________ |
| 9. 15002 | _______________ | _______________ |
| 10. 99215 | _______________ | _______________ |
CPT Format
Section Arrangement
Within each of the six sections of CPT, there is a repetitive, consistent structure.
| Section | Identifies the service and code range (e.g., Surgery) |
| Subsection | Identifies the type of service (e.g., Integumentary) |
| Heading | Identifies anatomical setting (e.g., Skin, subcutaneous and accessory structures) |
| Subheading | Identifies the service (e.g., Incision and drainage) |
Indented Format
A procedure description containing a semicolon (;) is divided into two parts:
1. The wording before (to the left of) the semicolon is considered the common language of the code.
2. The wording following (to the right of) the semicolon is a unique description pertinent only to that specific code.
Guidelines for Using Notes
 Notes that appear immediately after a heading or subheading apply to all entries in that heading or subheading.
Notes that appear immediately after a heading or subheading apply to all entries in that heading or subheading.
 Notes that appear in parentheses apply in general to the entry immediately above it or immediately below it.
Notes that appear in parentheses apply in general to the entry immediately above it or immediately below it.
 Notes that appear at the end of a series of codes may apply either to all of the preceding series or to only the code immediately above it.
Notes that appear at the end of a series of codes may apply either to all of the preceding series or to only the code immediately above it.
 A note in a block of type may apply to all entries beneath it as in the beginning of a heading or subheading, or it may apply to all of the preceding section.
A note in a block of type may apply to all entries beneath it as in the beginning of a heading or subheading, or it may apply to all of the preceding section.
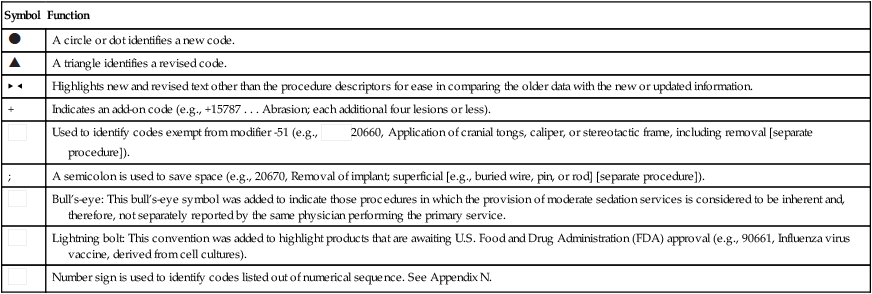
CPT Symbols
| Symbol | Function |
 | A circle or dot identifies a new code. |
 | A triangle identifies a revised code. |
| ▶ ◀ | Highlights new and revised text other than the procedure descriptors for ease in comparing the older data with the new or updated information. |
| + | Indicates an add-on code (e.g., +15787 . . . Abrasion; each additional four lesions or less). |
 | Used to identify codes exempt from modifier -51 (e.g.,  20660, Application of cranial tongs, caliper, or stereotactic frame, including removal [separate procedure]). 20660, Application of cranial tongs, caliper, or stereotactic frame, including removal [separate procedure]). |
| ; | A semicolon is used to save space (e.g., 20670, Removal of implant; superficial [e.g., buried wire, pin, or rod] [separate procedure]). |
 | Bull’s-eye: This bull’s-eye symbol was added to indicate those procedures in which the provision of moderate sedation services is considered to be inherent and, therefore, not separately reported by the same physician performing the primary service. |
 | Lightning bolt: This convention was added to highlight products that are awaiting U.S. Food and Drug Administration (FDA) approval (e.g., 90661, Influenza virus vaccine, derived from cell cultures). |
 | Number sign is used to identify codes listed out of numerical sequence. See Appendix N. |
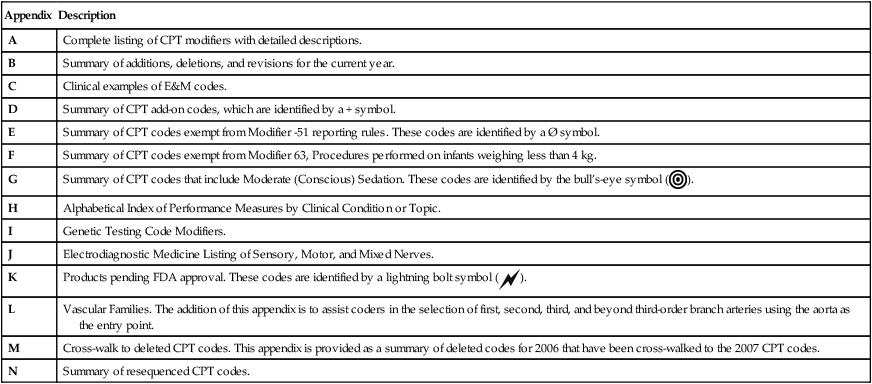
CPT Appendixes
| Appendix | Description |
| A | Complete listing of CPT modifiers with detailed descriptions. |
| B | Summary of additions, deletions, and revisions for the current year. |
| C | Clinical examples of E&M codes. |
| D | Summary of CPT add-on codes, which are identified by a + symbol. |
| E | Summary of CPT codes exempt from Modifier -51 reporting rules. These codes are identified by a Ø symbol. |
| F | Summary of CPT codes exempt from Modifier 63, Procedures performed on infants weighing less than 4 kg. |
| G | Summary of CPT codes that include Moderate (Conscious) Sedation. These codes are identified by the bull’s-eye symbol ( ). ). |
| H | Alphabetical Index of Performance Measures by Clinical Condition or Topic. |
| I | Genetic Testing Code Modifiers. |
| J | Electrodiagnostic Medicine Listing of Sensory, Motor, and Mixed Nerves. |
| K | Products pending FDA approval. These codes are identified by a lightning bolt symbol ( ). ). |
| L | Vascular Families. The addition of this appendix is to assist coders in the selection of first, second, third, and beyond third-order branch arteries using the aorta as the entry point. |
| M | Cross-walk to deleted CPT codes. This appendix is provided as a summary of deleted codes for 2006 that have been cross-walked to the 2007 CPT codes. |
| N | Summary of resequenced CPT codes. |
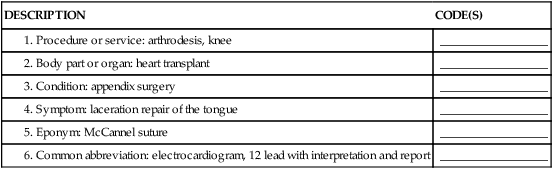
Index
The index offers the following four primary classes of main entries or ways to look up a code:
1. Name of procedure or service (e.g., Endoscopy)
2. Organ part or anatomical site (e.g., Colon)
3. Patient’s condition (e.g., Abscess)
4. Symptom, common abbreviation, or eponym (the name of person who developed the procedure or service)
CPT Coding Exercise 2
Index Guide
Directions: Find the code in the index. Underline the keyword used to find the code.
Example: Description: Consultation, x-ray; Code (s): 76140
| DESCRIPTION | CODE(S) |
| __________________ | |
| __________________ | |
| __________________ | |
| __________________ | |
| __________________ | |
| __________________ |
The Coding Process
General Guidelines
 Review information and identify services and procedures to code.
Review information and identify services and procedures to code.
 Review and understand the content of the terms contained in the medical record.
Review and understand the content of the terms contained in the medical record.
 Select and locate key terms in the index.
Select and locate key terms in the index.
 Locate the code in the body of the book.
Locate the code in the body of the book.
 Read the notes for using the codes, and select the most appropriate code.
Read the notes for using the codes, and select the most appropriate code.
Modifiers
Functions of a Modifier
The primary functions of modifiers are as follows:
 To record a service or procedure that has been modified but not changed in its identification or definition
To record a service or procedure that has been modified but not changed in its identification or definition
 To explain special circumstances or conditions of patient care
To explain special circumstances or conditions of patient care
 To indicate repeat or multiple procedures
To indicate repeat or multiple procedures
 To show cause for higher or lower costs while protecting charge history data
To show cause for higher or lower costs while protecting charge history data
| Modifiers | |||
| All of the modifiers are listed with examples of correct coding applications. | |||
-22 | Unusual Procedural Services | ||
| When the service provided is greater than the time or service usually required for the procedure. Example:A surgical procedure that usually takes 1 hour took 3 hours. A report or summary should accompany the claim to explain the reason for the increase in charges. | |||
| Correct Coding: | 58180-22 | (Supracervical abdominal hysterectomy) | |
-23 | Unusual Anesthesia | ||
| Occasionally, a procedure that usually requires either no anesthesia or local anesthesia must be done under general anesthesia because of unusual circumstances. This circumstance is reported by adding modifier -23 to the procedure code of the basic service. Example:During a sigmoidoscopic procedure, the patient required general anesthesia. | |||
| Correct Coding: | 45330 | Sigmoidoscopy, flexible | |
| 45330-23 | General anesthesia applied | ||
-24 | Unrelated Evaluation and Management Service by the Same Physician during a Postoperative Period | ||
| Use this modifier when the physician needs to indicate that an E&M service was performed during a postoperative period for a reason (or reasons) unrelated to the original procedure. Example:A patient had gallbladder surgery but came to the office because of a cold 3 weeks following the procedure (same physician). By using this modifier, the coder alerts the carrier that the office visit was not related to the surgical procedure. The physician will then be paid for the visit pertaining to the cold. | |||
| Correct Coding: | 99213-24 | (Established patient office visit) | |
-25 | Significant, Separately Identifiable E&M Service by the Same Physician on the Day of a Procedure | ||
| This modifier indicates that on the day a procedure or other service was performed, the patient’s condition required a significant, separately identifiable E&M service above and beyond the usual preoperative and postoperative care associated with the procedure that was performed. Example:A patient was seen for a sore throat and the removal of a wart. Both services (the office visit and the procedure) should be coded, because the reason for the office visit (sore throat) was unrelated to the reason for the surgery. | |||
| Correct Coding: | 17110 | Wart removal | |
| 99213-25 | Office visit | ||
-26 | Professional Component | ||
| Certain procedures are a combination of a physician component and a technical component. To report only the physician component, add this modifier to the CPT code number. Example:The patient has had a chest x-ray, and the physician is only interpreting the film. | |||
| Correct Coding: | 71010 | Radiology examination, chest, single | |
| 71010-26 | Interpretation only | ||
-32 | Mandated Services | ||
| This modifier applies to services related to mandated treatments or testing (e.g., third-party payer, governmental, legislative, or regulatory requirement). Example:Mandated service | |||
| Correct Coding: | 99243-32 | Outpatient consultation, mandated | |
-47 | Anesthesia by Surgeon | ||
| Use this modifier to code for the services of regional or general anesthesia when this service is provided by the surgeon. Do not use it to code local anesthesia. Example:The surgeon who drained the patient’s cyst also administered a regional anesthetic. | |||
| Correct Coding: | 40801-47 | Drainage of abscess, cyst, hematoma, vestibule of mouth; with application of anesthesia by the surgeon | |
-50 | Bilateral Procedure | ||
| When the same procedure is performed on both sides of the body, use this modifier to indicate that service. The modifier is appended to the second procedure. Example:The patient had two hernias, one in the right groin and one in the left groin that were repaired at the same operative session. | |||
| Correct Coding: | 49520 | Repair recurrent inguinal hernia, right side | |
| 49520-50 | Repair recurrent inguinal hernia, left side | ||
-51 | Multiple Procedures | ||
| When multiple procedures other than E&M services are performed on the same day or during the same operative session by the same provider. The services are reported as follows: Example:The surgeon removed the patient’s uterus and also cut an opening into the bladder to drain it. | |||
| Correct Coding: | Primary procedure: 58150 | Supracervical abdominal hysterectomy | |
| Secondary procedure: 51040-51 | Cystostomy with drainage | ||
-52 | Reduced Services | ||
| Under certain circumstances, a service or procedure is partially completed. This modifier alerts the carrier that a reason exists for a lower than usual charge. The reduced services modifier will protect the charge data for the practice. Example:93923, Noninvasive physiological studies of upper or lower extremity arteries, multiple levels or with provocative functional maneuvers, complete bilateral study (e.g., segmental blood). The study was performed on a patient with a history of amputation of the extremity. | |||
| Correct Coding: | 93923-52 | Noninvasive physiological studies of upper or lower extremity arteries | |
-53 | Discontinued Procedure | ||
| The physician may elect to terminate a procedure due to extenuating circumstances or because it threatens the well-being of the patient. Note: This modifier is not used to report the elective cancellation of a procedure before the patient’s anesthesia induction and/or surgical preparation in the operating suite. Example:The physician began a colonoscopy but had to discontinue the procedure because the patient had not been properly prepped. | |||
| Correct Coding: | 45378-53 | Colonoscopy, discontinued | |
-54 | Surgical Care Only | ||
| This modifier indicates that one physician performed a surgical procedure and another physician provided preoperative and/or postoperative management. Example:The physician performed only the laminectomy. | |||
| Correct Coding: | 63250-54 | Laminectomy, surgical procedure only | |
-55 | Postoperative Management Only | ||
| This modifier indicates that a physician other than the surgeon provided the postoperative care. Example:A physician other than the surgeon provided the postoperative management of the laminectomy. | |||
| Correct Coding: | 63250-55 | Laminectomy, postoperative management | |
-56 | Preoperative Management Only | ||
| This modifier indicates that a physician other than the surgeon provided the preoperative evaluation of the patient. Example:A physician, other than the surgeon, performed the preoperative evaluation before the patient was admitted for a laminectomy. | |||
| Correct Coding: | 63250-56 | Laminectomy, preoperative management | |
-57 | Decision for Surgery | ||
| Use this modifier for an E&M service that results in the initial decision to perform surgery. It applies only to major procedures (i.e., those with a 90-day global period) when surgery is performed within 24 hours of the decision for the surgery. Example:During the encounter with the surgeon, the decision was made to perform surgery the next day. | |||
| Correct Coding: | 99203-57 | Initial office visit with decision for surgery made at the time of the visit | |
-58 | Staged or Related Procedure or Service by the Same Physician during the Postoperative Period | ||
| This modifier is used when the physician needs to indicate that a procedure or service performed during the postoperative period was planned prospectively at the time of the original procedure (staged), was more extensive than the original procedure, or was performed for therapy following a diagnostic surgical procedure.Example:The patient had a breast biopsy. The results indicated a need for a partial mastectomy. The service was scheduled within the 10-day global period of the biopsy. | |||
| Correct Coding: | 19160-58 | Mastectomy, partial | |
-59 | Distinct Procedural Service | ||
| This modifier indicates that a procedure or service was distinct or independent from other services performed on the same day. It is used to identify procedures or services that are not normally reported together but are appropriate under the circumstances. This may represent a different patient encounter, different site or organ system, separate lesion, or separate injury not ordinarily encountered or performed on the same day by the same physician. Example:Removal of a lesion from the arm and another from the back. | |||
| Correct Coding: | 11601 | Excision, malignant lesion (first lesion) | |
| 11601-59 | Excision, malignant lesion (second lesion) | ||
-62 | Two Surgeons | ||
| Under certain circumstances, two surgeons (usually with different skills) may be required to manage a surgical procedure. Example:A laminectomy was performed by a neurosurgeon and an orthopedic surgeon. Each bills the same CPT code with modifier -62. | |||
| Correct Coding: | 63250-62 | Laminectomy, two surgeons | |
-63 | Procedure Performed on an Infant Weighing Less Than 4 kg | ||
| In some cases, the small size of a neonate or infant significantly increases the complexity and physician work components required for a procedure. This modifier is used only for procedures on patients in this circumstance. Example:The patient is a 3-kg infant who requires an enterectomy, resection of small intestine. | |||
| Correct Coding: | 44120-63 | Enterectomy, resection of small intestine; single resection and anastomosis | |
-66 | Surgical Team | ||
| Use this modifier when highly complex procedures (i.e., those requiring the concomitant services of several physicians, often of different specialties, plus other highly skilled, specially trained personnel and various types of complex equipment) are carried out under the “surgical team” concept. Example:A heart transplantation required the skills of a highly trained cardiovascular team. | |||
| Correct Coding: | 33945-66 | Heart transplant, with or without recipient cardiectomy | |
-76 | Repeat Procedure by Same Physician | ||
| Use this modifier when a physician needs to indicate that a procedure or service was repeated subsequent to the original service on the same day. Example:The patient had an ECG (93000) in the morning with a repeat ECG in the afternoon. | |||
| Correct Coding: | 93000-76 | ECG, repeat procedure | |
-77 | Repeat Procedure by Another Physician | ||
| This modifier indicates that a procedure had been performed by another physician on the same day and was repeated by a different physician. Example:The patient had an ECG (93000) at the primary care physician’s office and was sent to a cardiologist who repeated the ECG on the same day. | |||
| Correct Coding: | 93000-77 | ECG, repeat procedure | |
-78 | Return to the Operating Room for a Related Procedure | ||
| This modifier indicates that another procedure, related to the first procedure, was performed during the initial procedure’s postoperative period and required a return to the operating room. Example:The patient had abdominal surgery. Three days after surgery an infection occurs in the wound site, requiring the patient to return to the operating room for debridement of the wound site. | |||
| Correct Coding: | 11000-78 | Debridement of necrotic tissue, related procedure | |
-79 | Unrelated Procedure or Service in a Postoperative Period | ||
| When a patient is seen by the same physician for an unrelated problem or condition during the postoperative period, use this modifier. Example:A patient has a Maze procedure for the treatment of atrial fibrillation (33253) and goes home. The wound site is healing well. Two weeks later, the patient is seen by the same physician for pericardiotomy for removal of a foreign body (33020). Because the second procedure is within the global period for the original surgery, attach modifier -79 to the second procedure. | |||
| Correct Coding: | 33020-79 | Pericardiotomy | |
-80 | Surgical Assistant | ||
| This modifier identifies the services of another physician who acts as a second pair of hands for a surgical procedure. Example:A patient undergoes intestinal fistula closure (44640), requiring the assistance of another physician to complete. The primary surgeon would report the service as 44640. To report the services of the assistant, add modifier -80 to the same code. | |||
| Correct Coding: | 44640-80 | Closure of intestinal fistula (Surgical assisting coding only) | |
-81 | Minimum Assistant Surgeon | ||
| Use this modifier for a procedure that does not normally require a surgical assistant but because of extenuating circumstances requires the services of another physician for a short time.Note: Many commercial insurance companies allow this modifier to be used when assistance is provided by personnel other than an MD or DO. For Medicare carriers, you must use modifier -AS to report services provided by an assistant who is not an MD or DO. Example:A patient treated for gingivitis requiring a gingivectomy (41820, excision gingiva, each quadrant) required the assistance of another physician for a short period of time. Note: This modifier may also be used to report surgical assistance of a nurse practitioner or physician assistant based on insurance company policies. | |||
| Correct Coding: | 41820-81 | Gingivectomy, excision gingiva, each quadrant | |
-82 | Assistant Surgeon | ||
| Use this modifier when a qualified resident surgeon is not available. This modifier is typically reserved for teaching hospitals and teaching physician services. Example:A teaching physician required assistance to close an intestinal fistula. At the time of the procedure, a resident was not available to provide assistance. Another teaching physician had to assist with the procedure. | |||
| Correct Coding: | 44640-82 | Closure of intestinal fistula | |
-90 | Reference (Outside) Laboratory | ||
| This modifier is used when laboratory procedures are performed by a party other than the treating or reporting physician. Use this modifier with only the 80000 code series. Example:A patient with Conn’s disease is scheduled for aldosterone studies in the morning and in the afternoon to compare the results of electrolyte excretion by the kidneys. | |||
| Correct Coding: | 82088-90 | Aldosterone | |
-91 | Repeat Clinical Diagnostic Laboratory Test | ||
| Use this modifier to indicate a repeat of the same laboratory test on the same day to obtain subsequent (multiple) test results. Note: This modifier may not be used when tests are performed to confirm initial results; when specimen testing problems or equipment failure occur; or for any other reason when a normal, one-time, reportable is all that is required. This modifier may not be used when other code(s) describe a series of test results (e.g., glucose tolerance testing, evocative/suppression testing). | |||
| Correct Coding: | 82088 | Aldosterone | |
| 82088-91 | Aldosterone | ||
-92 | Alternate Laboratory Platform Testing | ||
| Use this modifier when laboratory testing is performed using a kit or transportable instrument. | |||
| Correct Coding: | 86701 86701-92 | HIV testing HIV testing | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


















