Sentinel Lymph Node Biopsy in Breast Cancer
Armando E. Giuliano
Sanjay P. Bagaria
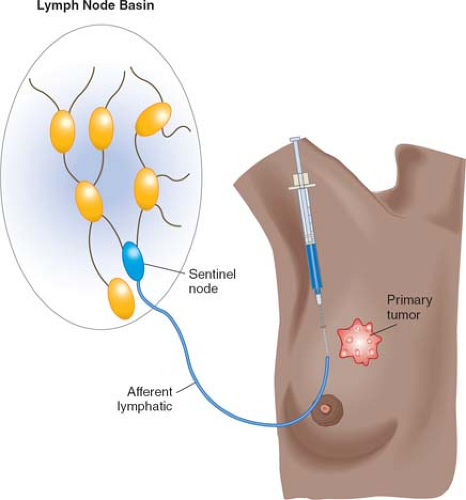
Sentinel node biopsy is based on the concept that an afferent lymphatic from a primary tumor drains first to the “sentinel” node before reaching second-tier (nonsentinel) nodes in the regional nodal basin. Because this sentinel node is the first node encountered by tumor cells as they metastasize to the regional nodal basin, it represents the tumor status of the entire nodal basin. Selective identification, removal, and histopathologic analysis of sentinel nodes therefore can be used to identify occult nodal metastasis without undertaking complete lymph node dissection.
Intraoperative lymphatic mapping and sentinel lymph node biopsy, or sentinel lymph node dissection (SLND), was pioneered in melanoma and subsequently adapted to breast cancer in the early 1990s. Although technical aspects of this procedure vary with the type of cancer, the overall approach is the same: a mapping agent is used to track the path of lymphatic drainage from a primary tumor to the first tumor-draining lymph node (sentinel node) in patients with clinically normal lymph nodes (Fig. 1). If this sentinel node contains tumor cells, then other nodes in the basin may harbor metastasis and complete nodal dissection should be performed. If the sentinel node is tumor-free, then regional nodal metastases are highly unlikely and further nodal resection is not indicated.
Because the tumor status of the axillary lymph nodes is one of the most important prognostic indicators for overall survival in breast cancer, the sentinel node concept has changed the paradigm for management of clinically localized disease. Instead of undertaking complete axillary lymph node dissection (ALND), which is associated with significant complications, surgeons can use SLND to stage the axilla and identify breast cancer patients with occult nodal disease. This minimally invasive sampling technique is less morbid than ALND; it is also far more accurate because it yields a small, high-risk nodal specimen that can be cost-effectively ultrastaged by immunohistochemistry (IHC) of multiple sections. Numerous studies report sentinel node identification rates of 95% or higher and false-negative rates of less than 5%. Histopathologic analysis of sentinel and nonsentinel nodes from the same drainage basin confirms a low rate of false-negative results for SLND: the rate of nonsentinel nodal metastasis is less than 5% when the sentinel node specimen is tumor-free. Thus, routine ALND for patients with clinically node-negative early breast cancer has been replaced by completion ALND only in patients with tumor-positive sentinel nodes.
SLND is appropriate for almost any patient who has early invasive breast cancer and presents without clinically palpable axillary lymph nodes. The use of SLND for large tumors (≥5 cm) remains controversial, though several studies have found high identification rates and accuracy for lymphatic mapping of large tumors. SLND in patients with multicentric and multifocal disease is currently acceptable. A multi-institutional study in patients with multicentric disease who underwent SLND followed by ALND demonstrated a sentinel node identification rate of 91.5% and a false-negative rate of 4%. Previous excisional biopsy is not a contraindication.
The timing of SLND in patients treated with preoperative chemotherapy is controversial. Patients receiving preoperative therapy may undergo SLND prior to chemotherapy to provide definitive staging information. If the sentinel node is positive, this approach commits the patient to completion ALND following chemotherapy and therefore negates the potential benefit of preoperative therapy downstaging. SLND performed after chemotherapy has been criticized for variable high false-negative rates. A meta-analysis of studies on SLND following preoperative chemotherapy showed a pooled sentinel node identification rate of 90% and an overall accuracy of 94%. While it is attractive to perform SLND after neoadjuvant therapy, until large trials establish the accuracy of SLND after preoperative chemotherapy and the safety of nonoperative management of the axilla in
patients whose cancers were downstaged from node positive to node negative, completion ALND should be performed by most surgeons if the sentinel node contains metastasis before chemotherapy.
patients whose cancers were downstaged from node positive to node negative, completion ALND should be performed by most surgeons if the sentinel node contains metastasis before chemotherapy.
Breast augmentation is usually not a problem for SLND, except when the implant is inserted through the axilla. A relative contraindication to SLND is recent major reduction mammoplasty or axillary surgery such as axillary node biopsy, as the lymphatic drainage of the cancer may be altered and may result in a false-negative sentinel node. However, SLND performed many years after reduction mammoplasty or even after prior SLND appears accurate. SLND in pregnancy is a relative contraindication because blue dye should be avoided. However, radiocolloid is most likely safe as it exposes the fetus to very little radiation, well below the limit set by the National Council on Radiation Protection and Measurements. Absolute contraindications to SLND include inflammatory breast cancer and the presence of metastatic axillary lymphadenopathy.
An understanding of mapping agents and surgical technique is essential to accurately identify the sentinel node with minimal morbidity. Two lymphatic mapping agents are usually used to identify sentinel nodes: blue dye or radiocolloid. Vital blue dye (1% isosulfan blue in the United States, patent blue V in Canada, Europe, or Australia) is injected intraoperatively and allows the surgeon to identify blue-stained lymph nodes during SLND. Alternatively or usually in addition, a radiocolloid such as technetium-labeled sulfur colloid is used. The radiocolloid is injected preoperatively usually in the nuclear medicine department the day before or the day of surgery. Lymphoscintigraphy with a gamma camera allows for identification of the radioactive sentinel nodes, with the skin overlying the “hot” (radioactive) area marked with indelible ink. A handheld gamma probe is used intraoperatively to identify radioactive nodes. Vital blue dye and radiocolloid can be used either alone or in combination. We prefer vital blue dye alone especially for outer quadrant lesions because of its accuracy and simplicity. Most authors have demonstrated improved accuracy with use of the two mapping agents together, but successful identification depends on the experience of the surgeon and not on the agents. We use a combination of vital blue dye and radiocolloid for medially located lesions or when SLND is performed for recurrent tumors, after prior axillary staging, or after prior axillary surgery.
There has been much debate about the technical aspects of SLND when radiocolloid is used. The timing and location of injection, the size of the colloid particle and volume, and whether to use filtered or unfiltered radiocolloid are issues that have not been standardized. We typically inject around the tumor or biopsy cavity with 8 cc of radiocolloid reconstituted in saline divided into six injections. While others favor smaller volumes of radiocolloid and different injection sites (subareolar, subcutaneous, or dermal), good results have been achieved with many lymphatic mapping techniques. The choice of radiocolloid is usually dictated by availability and approval by the national or state governing agencies.
The routine use of dynamic lymphoscintigraphy is also debated. A hard-copy lymphoscintigram obtained approximately 20 minutes after injection typically displays all drainage areas (Fig. 2). We prefer to obtain a lymphoscintigram for medial lesions because of the higher frequency of internal mammary drainage from the inner quadrants. Some clinicians may choose to extend the radiation fields or excise the internal mammary node(s) through an interspace if they are seen on the lymphoscintigram. If the lymphoscintigram fails to document drainage to an axillary node, intraoperative lymphatic mapping with blue dye will often still identify an axillary sentinel node.
We prefer general anesthesia but sedation and local anesthesia can be used. After induction, the patient is positioned supine, and the breast, chest wall, axilla, and entire arm are prepared and draped with the arm free. Using a 25-gauge needle, blue dye is injected in a fan-shaped manner to infiltrate the axillary side of the tumor or the subareolar region. Blue dye should not be injected intradermally or it may tattoo the skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree